Effects of Telemedicine through VDO Call on Self-Care Behavior and Glycated Hemoglobin Levels among Thai Muslim Patients with Diabetes
Keywords:
Diabetes, Telemedicine, In-person Medical Care, Self-Care Behavior, Glycated Hemoglobin (HbA1c) LevelsAbstract
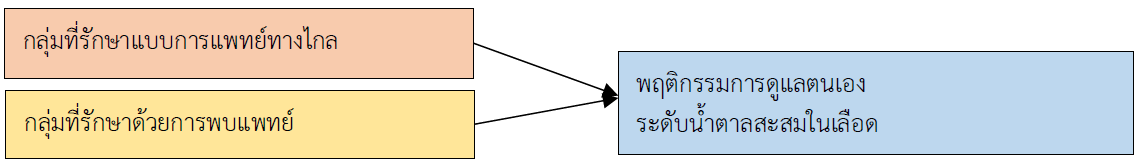
This quasi-experimental study with a two-group pretest-posttest design aimed to compare self-care behavior scores and glycated hemoglobin (HbA1c) levels in diabetic patients in Yi-ngo District, Narathiwat Province, between those receiving telemedicine treatment and those receiving in-person medical care. The study included 102 diabetic patients who received services at sub-district health-promoting hospitals, in a Muslim cultural context. The experimental tools used were telemedicine treatment and in-person medical care. Data collection instruments included a self-care behavior questionnaire and a glycated hemoglobin (HbA1c) level record. The content validity index (CVI) of the instruments was 0.91, and the Cronbach’s alpha reliability coefficient was 0.778. Data were analyzed using frequency, percentage, mean, standard deviation, Chi-square test, Fisher’s Exact Test, Mann-Whitney U Test, Independent T Test, Dependent T Test, and Wilcoxon Signed Rank Test. The research findings revealed as follows.
1. For the in-person medical care group: After the experiment, the overall self-care behavior score increased, and glycated hemoglobin (HbA1c) levels significantly decreased at the .05, .01, and .001 levels. However, there was no significant difference in stress management behavior before and after the experiment. For the telemedicine treatment group: The overall self-care behavior score increased, and glycated hemoglobin (HbA1c) levels significantly decreased at the .05, .01, and .001 levels. However, there were no significant differences before and after the experiment in dietary habits, stress management, and continuity of care behaviors.
2. Comparison between the two groups after the experiment: The in-person medical care group had significantly higher overall and domain-specific self-care behavior scores than the telemedicine group. Glycated hemoglobin (HbA1c) levels were significantly lower in the in-person medical care group compared to the telemedicine group at the .05, .01, and .001 levels.
Therefore, both treatment methods should be integrated to align with the Thai Muslim context in Narathiwat Province and the southern border provinces. This approach could enhance patient confidence in treatment while reducing hospital overcrowding.
References
Chirawatkul, A. (2013). Designing Questionnaires for Research. Bangkok: Witthayapat. (in Thai)
Dawson, K. G., Jin, A., Summerskill, M., & Swann, D. (2021). Mobile diabetes telemedicine clinics for aboriginal first nation people with reported diabetes in British olumbia. Canadian Journal Diabetes, 45(1), 89-95. doi: 10.1016/j.jcjd.2020.05.018.
Department of Medical Services. (2021). Guidelines for Using DMS Telemedicine, Department of Medical Services. Nonthaburi: Ministry of Public Health. (in Thai)
Diabetes Association of Thailand. (2023). Clinical Practice Guidelines for Diabetes 2023. Bangkok: Srimuang Pringing. (in Thai)
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175-191.
Hair, F. J., Black, C. W., Babin, J. B., & Anderson, E. R. (2019). Multivariate Data Analysis. (7th ed). New Jersey: Pearson Education.
Intarachote, U. (2020). The results of supporting participatory self-management in diabetic patients, Na Fai subdistrict, Muang district, Chaiyaphum province. Chaiyaphum Medical Journal, 40(1), 137-147. (in Thai)
Internation Diabetes Federal [IDF]. (2021). IDF Diabetes Atlas. Retrieved June 28, 2024 from https://www.diabetesatlas.org/
Jin, M. X., Kim, S., Miller, L. J., Behari, G., & Correa, R. (2020). Telemedicine: Current impact on the future. Cureus,12(8), e9891. doi:10.7759/cureus.9891
Kang, J. Y., Jung, W., Kim, H. J., An, J. H., Yoon, H., Kim, T., et al. (2024). Temporary telemedicine policy and chronic disease management in south korea: Retrospective analysis using national claims data. JMIR Public Health Surveillance, 10, e59138. doi: 10.2196/59138.
Kisling, L. A., & Das, J. M. (2024). Prevention Strategies. Retrieved June 30, 2024 from https://www.ncbi.nlm.nih.gov/books/NBK537222/
Lohsoonthorn, V. (2018). Epidemiology. Bangkok: Chulalongkorn University Press. (in Thai)
Ming, W. K., Mackillop, L. H., Farmer, A., Loerup, L., Bartlett, K., Levy, J. C., et al. (2016). Telemedicine technologies for diabetes in pregnancy: A systematic review and meta-analysis. Journal of Medical Internet Research, 18(11), e290. doi: 10.2196/jmir.6556.
Pragosuntung, N. (2024). The effect of telenursing program with glycemic control in type 2 diabetes mellitus patients authors. Journal of Research and Health Innovative Development, 5(2), 100-111. (in Thai)
Siangdang, S. (2019). Foot care behaviors with type 2 diabetes at diabetes clinic of Singhanakorn hospital, Songkhla. Thai Journal of Public Health and Health Sciences, 2(3), 1–15. (in Thai)
Somton, T. (2024). Comparative effect of telemedicine on glycemic control management among diabetes mellitus type II patients in Suratthani’s prison healthcare unit. Region 11 Medical Journal, 38(2), 1-10. (in Thai)
Sudnongbua, R. (2024). A comparison efficacy of telemedicine platform and traditional algorithm in patient with diabetes mellitus for control blood sugar in Mahachanachai hospital Yasotorn hospital. Academic Journal of Community Public Health, 10(2), 200-210.
Sun, C., Sun, L., Xi, S., Zhang, H., Wang, H., Feng, Y., et al. (2019). Mobile phone-based telemedicine practice in older chinese patients with type 2 diabetes mellitus: Randomized controlled trial. JMIR mHealth and uHealth, 7(1), e10664. doi.org/10.2196/10664
Tuomilehto, J., Lindstrom, J., Eriksson, J. G., Valle, T. T., Hamalainen, H., Ilanne-Parikka, P, et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med, 344(18),1343-1350.
Wongsuphee, P., Chusak, T., & Banchonhattakit, P. (2024). Effects of telemedicine on self-care behaviors and blood sugar level of diabetic patients with uncontrolled blood glucose levels in Huai Khot hospital, Uthai Thani province. Singburi Hospital Journal, 33(2), B49-B61. (in Thai)
Yingo Hospital. (2024). HDC Program. Narathiwat: Yingo Hospital. (in Thai)
Zamani-Alavijeh, F., Araban, M., Koohestani, H. R., & Karimy, M. (2018). The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetology & Metabolic Syndrome, 10, 39. doi.org/10.1186/s13098-018-0342-5.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The Southern College Network Journal of Nursing and Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







