The Effects of a Hypertension Prevention Behavior Development Program with Telehealth on Hypertension Risk Groups in a Rural Udon Thani District
Keywords:
Hypertension, Telehealth, Risk Groups, Hypertension Prevention BehaviorAbstract
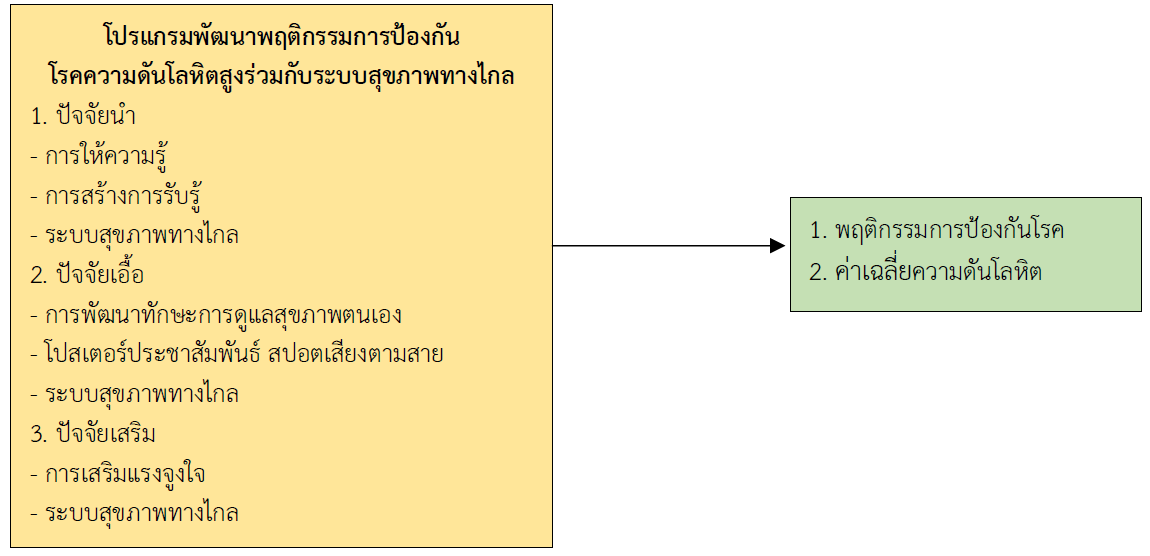
This quasi-experimental study investigated the effects of a hypertension prevention behavior modification program combined with telehealth on individuals at risk for hypertension. The study assessed changes in hypertension prevention behaviors and blood pressure levels within the experimental group before and after the intervention, and between the experimental and control groups after the intervention. Sixty individuals aged 35 – 59 at risk for hypertension were randomly assigned to either an experimental group (n = 30) or a control group (n = 30) using simple random sampling. The intervention was a hypertension prevention behavior modification program combined with telehealth, developed based on the PRECEDE model. A validated questionnaire, with content validity indices of .92 and .95 and a reliability coefficient of .71, was used to collect data on general information and hypertension prevention behaviors. Data were analyzed using descriptive statistics, paired t-tests, and independent t-tests. The results showed:
1. Post-intervention, the experimental group had significantly higher hypertension prevention behavior scores compared to both their pre-intervention scores and the control group (p-value < .01).
2. Post-intervention, the experimental group had significantly lower systolic and diastolic blood pressure levels compared to both their pre-intervention levels and the control group (p-value < .05).
These findings suggest that a hypertension prevention behavior development program combined with telehealth can be effective in promoting behavioral changes for hypertension prevention. This approach could be applied to prevent hypertension and other chronic diseases in the future.
References
Aekplakorn, W., Pakcharoen, H., & Sathiennoppakao, W. (2021). The Sixth Thai National Health Examination Survey, 2019-2020. Bangkok: Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Bashshur, R. L., Howell, J. D., Krupinski, E. A., Harms, K. M., Bashshur, N., & Doarn, C. R. (2016). The empirical foundations of telemedicine interventions in primary care. Telemedicine and e-Health, 22(5), 342–375. doi.org/10.1089/tmj.2016.0045
Bunyarang, S. (2018). The Effect of a Behavior Modification Program for Hypertension Prevention in at Risk Groups in Phen District, Udon Thani Province (Master’s thesis). Bangkok: Sukhothai Thammathirat Open University. (in Thai)
Caplin, A., Chen, F. S., Beauchamp, M. R., & Puterman, E. (2021). The effects of exercise intensity on the cortisol response to a subsequent acute psychosocial stressor. Psychoneuroendocrinology, 131, 105336. doi.org/10.1016/j.psyneuen.2021.105336
Chanaman, P. (2024). The effects of self-management promotion program using telenursing on stroke prevention behaviors in uncontrolled hypertensive patients. Journal of Nursing and Health Sciences, 4(3), 33-46. (in Thai)
Department of Disease Control. (2019). Blood Pressure: Measure Early, Know Eearly, Preventable. Nonthaburi: Bureau of Non-Communicable Diseases. (in Thai)
Department of Disease Control. (2022). Department of Disease Control Advises Citizens to Pay Attention to Health and Measure Blood Pressure Regularly to Prevent Hypertension. Retrieved May 25, 2023, from https://ddc.moph.go.th/brc/news.php?news=25290 &deptcode=brc&news_views=388 (in Thai)
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences*. Behavior Research Methods, 39(2), 175–191.
Filippini, T., Malavolti, M., Whelton, P. K., Naska, A., Orsini, N., & Vinceti, M. (2021). Blood pressure effects of sodium reduction: Dose-response meta-analysis of experimental studies. Circulation, 143(16). doi.org/10.1161/CIRCULATIONAHA.120.050371
Green, L. W., & Kreuter, M. W. (2005). Health Program Planning: An Educational and Ecological Approach (4th ed.). McGraw-Hill.
Hoffer-Hawlik, M., Moran, A. E., Zerihun, L., Usseglio, J., Cohn, J., & Gupta, R. (2021). Telemedicine interventions for hypertension management in low- and middle-income countries: A scoping review. PLOS ONE, 16(7), e0254222. doi.org/10.1371/journal.pone.0254222
Loucks, E. B., Schuman-Olivier, Z., Saadeh, F., Scarpaci, M. M., Nardi, W. R., Gutman, R., et al. (2022).
Mindfulness-Based Blood Pressure Reduction: Evidence from the AHA Scientific Sessions 2022. American Heart Association. Retrieved October 7, 2024, from https://professional.heart.org/en/meetings/scientific-sessions
Mangsakoo, U. (2019). The effects of health behavior modification program for elderly with hypertension at Suwannaphum District, Roi Et Province. Thai Journal of Nursing, 68(3), 1-10. (in Thai)
Santos, E. de S. G., & Souza, O. F. de. (2021). Evidence of the association between sleep duration and blood pressure in adolescents: A systematic review. Revista Paulista de Pediatria, 39, e2019225. doi.org/10.1590/1984-0462/2021/39/2019225
Schultz, M. G., La Gerche, A., & Sharman, J. E. (2017). Blood pressure response to exercise and cardiovascular disease. Current Hypertension Reports, 19(11), 89. doi.org/10.1007/s11906-017-0787-1
Srisatidnarakul, B. (2010). Nursing Research Methodology (5th ed.). U & I Intermedia. (in Thai)
Thai Hypertension Society. (2019). Guidelines for hypertension treatment in general practice, 2019. Chiang Mai: Trick Think. (in Thai)
Udon Thani Provincial Public Health Office, Health Data Center. (2023). Data to support the Service Plan in the field of non-communicable diseases (NCDs: DM, HT, CVD). Retrieved October 7, 2024 from https://udn.hdc.moph.go.th/hdc/reports/page.php?cat_id= 1ed90bc32310b503b7ca9b32af425a
Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Collins, K. J., Himmelfarb, C. D., et al. (2018). guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Journal of the American College of Cardiology, 71(19), e127–e248. doi.org/10.1016/j.jacc.2017.11.006
World Health Organization. (2021). Hypertension. Retrieved October 7, 2024 from https://www.who.int/news-room/fact-sheets/detail/hypertension
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The Southern College Network Journal of Nursing and Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







