การเปรียบเทียบสัดส่วนการจัดสรรงบประมาณกองทุนประกันสุขภาพแห่งชาติ ระหว่างคู่สัญญาบริการสาธารณสุขระดับปฐมภูมิให้กับโรงพยาบาลส่งเสริมสุขภาพตำบล ที่ถ่ายโอนและไม่ถ่ายโอนไปองค์กรปกครองส่วนท้องถิ่น
คำสำคัญ:
กองทุนประกันสุขภาพแห่งชาติ, การจัดสรรงบประมาณ, การถ่ายโอน , องค์กรปกครองส่วนท้องถิ่น, โรงพยาบาลส่งเสริมสุขภาพตำบลบทคัดย่อ
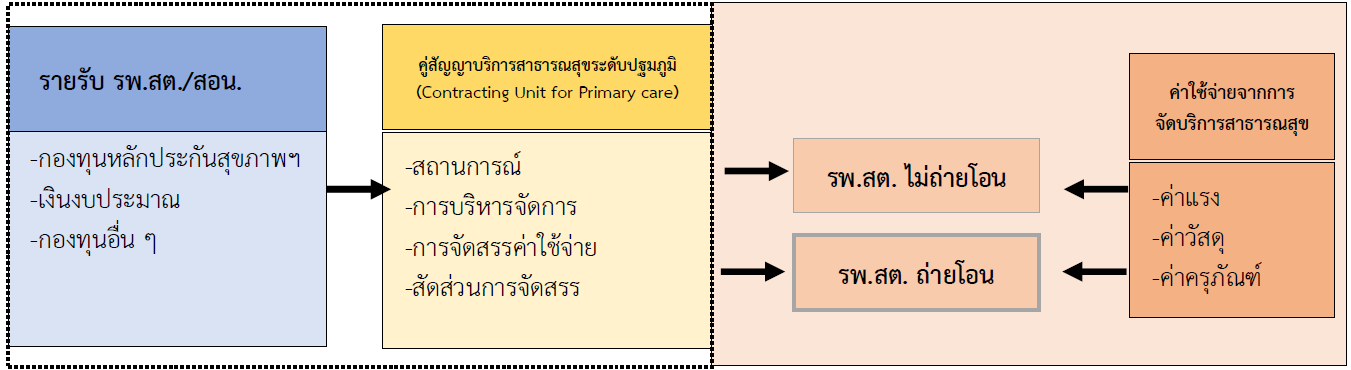
การวิจัยแบบผสมวิธีนี้มีวัตถุประสงค์เพื่อ 1) ศึกษาสถานการณ์ การบริหารจัดการ และการจัดสรรค่าใช้จ่ายเพื่อบริการสาธารณสุขกองทุนประกันสุขภาพของคู่สัญญาบริการสาธารณสุขระดับปฐมภูมิ (CUP) โดยการสัมภาษณ์เชิงลึกในกลุ่มคู่สัญญา จำนวน 4 คน และผู้อำนวยการโรงพยาบาลส่งเสริมสุขภาพตำบล (รพ.สต.) จำนวน 16 คน โดยการวิเคราะห์เนื้อหา 2) เปรียบเทียบสัดส่วนการจัดสรรค่าใช้จ่าย โดยใช้ข้อมูลจาก CUP, สำนักงานหลักประกันสุขภาพเขต, และ รพ.สต. 3) พัฒนาข้อเสนอรูปแบบการบริหารจัดการและการจัดสรรค่าใช้จ่าย โดยการวิเคราะห์ สังเคราะห์ งานวิจัย แนวคิด ทฤษฎี และบริบทที่เกี่ยวข้องกับการบริหารงบประมาณในปัจจุบันและในอนาคต ผลการวิจัยพบว่า
1. รูปแบบการจัดสรรขึ้นอยู่กับข้อตกลงของคณะกรรมการประสานงานระดับอำเภอ (คปสอ.) โดยจัดสรรเป็นมูลค่าเงิน เวชภัณฑ์ ครุภัณฑ์ และการจ่ายเป็นอัตราคงที่ (Fixed Cost)
2. CUP จัดสรรให้กับ รพ.สต. ไม่ถ่ายโอน เป็นเงินร้อยละ 73.05 เป็นสิ่งของร้อยละ 26.95 ส่วนรพ.สต. ถ่ายโอน เป็นเงินร้อยละ 54.78 เป็นสิ่งของร้อยละ 45.22
3. เพื่อให้เกิดความเป็นธรรมต่อการจัดบริการจึงเสนอ รูปแบบที่ 1 กรณี CUP เดิม (รพ.แม่ข่ายไม่เรียกเก็บค่าบริการ) ในบริบทแก้ไขระเบียบเงินบำรุง รูปแบบที่ 2 กรณี CUP เดิม (รพ.แม่ข่ายไม่เรียกเก็บค่าบริการ) ร่วมกับการโอนตรงไปที่ รพ.สต. ในบริบทไม่แก้ไขระเบียบเงินบำรุง และรูปแบบที่ 3 กรณี CUP ใหม่ (รพ.แม่ข่ายไม่เรียกเก็บค่าบริการ) ร่วมกับการโอนตรงไปที่ รพ.สต.
4. ข้อเสนอกองทุนประกันสุขภาพแห่งชาติควรทบทวนปรับรูปแบบการจัดสรรให้เกิดความเป็นธรรม และไม่เกิดความเหลื่อมล้ำในการจัดสรรค่าใช้จ่ายบริการทางการแพทย์ให้กับ รพ.สต. ถ่ายโอนและไม่ถ่ายโอน
กระทรวงสาธารณสุข กรมส่งเสริมการปกครองท้องถิ่น และสำนักงานหลักประกันสุขภาพสามารถนำไปใช้เพื่อพิจารณารูปแบบ กลไก สัดส่วนการจัดสรรค่าใช้จ่ายเพื่อบริการสาธารณสุขให้กับ รพ.สต. ที่ถ่ายโอน
เอกสารอ้างอิง
Barasa, E., Mathauer, I., Kabie, E., Ezumah, N., Mbau, R., Honda, A., et al. (2021). How do healthcare providers respond to multiple funding flows? A conceptual framework and options to align them. Health Policy and Planning, 36(6), 861–868.
Cashin, C., Ankhbayar, B., Phuong, HT., Jamsran, G., Nazad, O., Phuong, NK., et al. (2015). Assessing Health Provider Payment Systems: A Practical Guide for Countries Moving toward UHC. Washington DC: Joint Learning Network for Universal Health Coverage.
Chiangchaisakulthai, K., Wongsin, U., Isayathikom, K., Suppradist, W., Samiphuk, N. (2021). Unit cost of services in primary care cluster. Journal of Health Systems Research, 13(2), 175-187. (in Thai)
Chiangchaisakulthai, K., Wongsin, U. (2018). Cost of primary care service network in health region 8. Journal of Health Systems Research, 12(4), 681-690. (in Thai)
Chu, A., Kwon, S., Cowley, P. (2019). Health financing reforms for moving towards universal health coverage in The Western Pacific Region. Health Systems & Reform, 5(1), 32-47.
Department of Local Administration. (2021). List of Sub-District Health Promoting Hospitals and Health Stations that are Transferred to Local Administrative Organizations. Bangkok: Ministry of Interior. (in Thai)
Faramnuayphol, P. (2008). Money Allocation and Financial Situation of Primary Care Facilities (Health Center) Under the Creation of Universal Health Insurance. Bangkok: Health Information Development Office. (in Thai)
Joint Learning Network. (2016). Financing and Payment models for Primary Health Care Six Lesson from JLN Country Implementation Experience. USA: Joint Learning Network for Universal Healht Coverage.
Kulthanmanusorn, A., Saengruang, N., Wanwong, Y., Kosiyaporn, H., Witthayapipopsakul, W., Srisasalux, J., et al. (2018). Evaluation of the Devolved Health Centers: Synthesis Lesson Learnt from 51 Health Centers and Policy Options. Nonthaburi: Health Systems Research Institute. (in Thai)
Local Government Commission. (2017). Transferring Missions from Tambon Health Promoting Hospital to Local Government. Bangkok: The National Legislative Assembly. (in Thai)
National Health Security Office. (2022). Guidelines for the Practice of Claiming Expenses for Health Services for Fiscal Year 2022. Nonthaburi: Sahamitr Printing & Publishing Company Limited. (in Thai)
Phodha, T., Singweratham, N., Rochanathimoke, O., Techakehakit, W., Bunpean, A.. (2023). A compared cost analysis for health care services in tambon health promotion hospitals before and during the covid-19 pandemic period fiscal year 2019-2021. The Southern College Network Journal of Nursing and Public Health, 10(1), 170-181. (in Thai)
Quality and Standard Service Unit Support office. (2016). Service Unit Registration Audit Guideline for Main Contractor Service Unit, Primary Care Service Unit, Coordinate Service Unit. Bangkok: National Health Security Office. (in Thai)
Rutjamathamrong, P., Singweratham, N., Techakehakij, W., Boontiam, N., Kaewsing, P., Bunpean, A., et al. (2022). Development of Management Guideline for the Health Security Funds to Allocate Budget for The District Health Promoting Hospitals Transferred to the Local Administrative Organizations. Nontaburi: Health Systems Research Institute (HSRI). (in Thai)
Singweratham, N., Khunboonchan, T., Nawsuwan, K., Atitdid, P., Adulyarat, M. (2022). Unit cost of thai traditional medicine service activities for health promotion and disease prevention in health care providers under Ministry of Public Health for the 2018 fiscal year. Princess of Naradhiwas University Journal, 13(3), 89-107. (in Thai)
Sri-ngernyuang, L., Siriwan, P., Vongjinda, S., Chuenchom, S. (2012). Health Center Devolution: Lesson Learned and Policy Implications. Nonthaburi: Health Systems Research Institute. (in Thai)
Srisasalux, J., Vichathai, C., Kaewvichian, R. (2009). Experience with public health decentralization: The health center transfer model. Journal of Health Systems Research, 3(1), 16-34. (in Thai)
Sudhipongpracha, T., Choksettakij, W., Phuripongthanawat, P., Kittayasophon, U., Satthatham, N., Onphothong, Y. (2021). Policy Analysis and Policy Design for the Transfer of Subdistrict Health Promotion Hospitals to Provincial Administrative Organizations (PAOs). Nontaburi: Health Systems Research Institute (HSRI). (in Thai)
Suppatheerathada, J. (2020). Policy Recommendation for Budget Allocation on Subsidy Expenditure Budget for Local Government under Transfer Mission: Case Study in Tumbon Health promoting hospital. Bangkok: The Secretariat of the House of Representatives. (in Thai)
Techaatik, S., Nakham, P. (2009). Studying and Monitoring the Development of the Transfer System of Public Health Centers to Local Government Organizations. Journal of Health Systems Research, 3(1), 113-130. (in Thai)
Techakehakij, W., Singweratham, N., Wongyai, D., Nawsuwan, K. (2020). Unit costs of primary care units: a case study in Kamphaeng Phet, Fiscal Year 2018. Journal of Safety and Health, 13(2), 192-204. (in Thai)
Wongsin, U., Wannasri, A., Thamwanna, P., Pongpattrachai, D., Chiangchaisakulthai, K., Sakunphanit, T. (2017). Estimate Unit Cost per Capita of Services Provided at CUP Network. Journal of Health Systems Research, 10(2), 207-302. (in Thai)
ดาวน์โหลด
เผยแพร่แล้ว
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







