The Effects of a Nutrition Promotion Program on Clinical Outcomes in Cancer Patients Undergoing Chemotherapy
Keywords:
nutritional promotion program, clinical outcome, chemotherapyAbstract
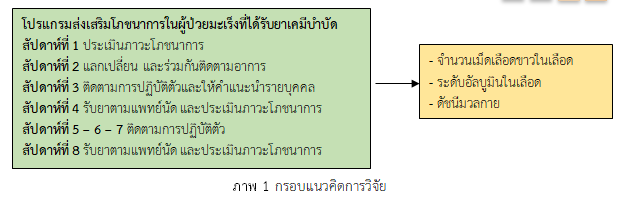
This quasi-experimental one group pre-posttest design research aimed to examine the effectiveness of a nutrition promotion program on clinical outcomes in cancer patients undergoing chemotherapy at Phrapokklao Hospital Chanthaburi. A total of 37 cancer patients were recruited using purposive sampling. The study was conducted between May and December 2021. The research instruments included a nutritional promotion program with a content validity index of .83, a general information questionnaire, a nutrition assessment questionnaire, a notebook for recording the type of food selection, and a Line application food tracking record form with a content validity index of 1.00 and 1.00, respectively. Data were analyzed using descriptive statistics and paired t-test.
The research results indicated that, after participating in the program, the median white blood cell count in the blood of the sample (Mdn=6,660, IQR=3,965) was higher than before (Mdn=5,690, IQR=3,210) with statistical significance (z=-3.07, p-value <.001). The albumin level in blood after participating in the program (M=4.46, SD=.39) was also higher than before (M=4.00, SD=.56) with statistical significance (t=3.25, p<.001). On the other hand, the body mass index of the participants (M=20.81, SD=3.80) was lower than before (M=21.32, SD=4.12) with statistical significance (t=-4.79, p-value <.001).
Nutrition promotion programs are an option for nurses and healthcare teams to apply to promote nutritional status in cancer patients undergoing chemotherapy, so to promote patient's readiness for chemotherapy and reduce the loss of treatment opportunities.
References
Arends, J., Bachmann, P., Baracos, V., Barthelemy, N., Bertz, H., Bozzetti, F., et al. (2017). ESPEN guidelines on nutrition in cancer patients. Clinical Nutrition, 36, 11e48 http://dx.doi.org/10.1016/j.clnu.2016.07.0150.
Boltong, A., Aranda, S., Keast, R., Wynne, R., Francis, P. A., Chirgwin, J., et al. (2014). Prospective cohort study of the effects of adjuvant breast cancer chemotherapy on taste function, food liking, appetite and associated nutritional outcomes. PLoS One, 9(7):e103512. doi:10.1371/journal.pone.0103512
Bourke, C. D., Berkley, J. A. & Prendergast, A. J. (2016). Immune dysfunction as a cause and consequence of malnutrition. Trends in Immunology, 37(6), 386-398.
Centers for Disease Control and Prevention. (2020). Neutropenia and Risk of Infection. Retrieved October 23, 2021 from https://www.cdc.gov/cancer/preventinfections /pdf/neutropenia.pdf
Gebremedhin, T. K., Cherie, A., Tolera, B. D., Atinafu, B. T., & Demelew, T. M. (2021). Prevalence and risk factors of malnutrition among adult cancer patients receiving chemotherapy treatment in cancer center, Ethiopia: cross-sectional study. Heliyon, 7(6), e07362. doi: 10.1016/j.heliyon.2021.e07362.
Grabiec, K., Burchert, M., Milewska, M., Błaszczyk, M., & Grzelkowska-Kowalczyk, K. (2013). Systemic and local mechanisms leading to cachexia in cancer. Postepy Hig Med Dosw (Online), 67, 1397– 1409. https://doi.org/10.5604/17322693.1085135
Kuakarn, J., Isaramalai, S., & Balti, Q. (2015). Impacts of a self-management programme for nutritional enhancement on the fatigue conditions of cancer patients undergoing radiotherapy. Thai Journal of Nursing Council, 30(2), 20-32. (in Thai).
Lookrak, S., Jirajaras, M., & Sirilerdtrakul, W. (2013). Self-care Guide while Receiving Chemotherapy. Retrieved October 13, 2021 from https://med.mahidol.ac.th/ cancer_center/sites/default/ files/public/pdf/Article/Selfcare.pdf. (in Thai).
Muscaritoli, M., Arends, J., Bachmann, P., Baracos, V., Barthelemy, N., Bertz, H., et al. (2021). ESPEN practical guideline: Clinical Nutrition in cancer. Clinical Nutrition, 40, 2898-2913.
National Cancer Institute. (2021). Hospital Based Cancer Registry 2020. Retrieved October 21, 2021 from https://www.nci.go.th/e_book/hosbased_2563/index.html. (in Thai).
Nurgali, K., Jagoe, R. T., Abalo, R. (2018). Editorial: Adverse effects of cancer chemotherapy: anything new to improve tolerance and reduce sequelae?. Front Pharmacol, 9, 245. doi: 10.3389/fphar.2018.00245.
Özkana, I., Taylanb, S., Eroğluc, N., & Kolaç, N. (2021). The Relationship between Malnutrition and Subjective Taste Change Experienced by Patients with Cancer Receiving Outpatient Chemotherapy reatment. Nutrition and Cancer, 74(5), 1670-1679.
Pattarakantakul, P. & Donlao, K. (2016). Effects of nutritional promotion program for chronic Obstructive pulmonary disease patients with malnutrition. Nursing Journal of The Ministry of Public Health, 27(2), 69-79. (in Thai).
Pimbung, N., Wattana, C. & Harnirattisai, T. (2015). The effects of a symptom-management program on severity of symptom and nutritional status among colorectal cancer patients receiving chemotherapy. Nursing Journal, 42, 73-83.
Prendergast, A. J. (2016). Immune dysfunction as a cause and consequence of malnutrition. Trends in Immunology, 37(6), 386-398.
Qin, N. & Jiang, G. (2019). Survey and analyze the nutritional status of postoperative chemotherapy patients with ovarian cancer. Journal of Parenteral and Enteral Nutrition, 26, 351–355. doi: 10.16151/j.1007-810x.2019.06.008
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer Journal for Clinicians, 71, 209–249.
Wang, Z., Zhang, L., Wang, J., Wang, Y., Dong, Q., Piao, H., et al. (2020). Prealbumin-to-globulin ratio can predict the chemotherapy outcomes and prognosis of patients with gastric cancer receiving first-line chemotherapy. Journal of immunology research, 2020. doi.org/10.1155/2020/6813176.
World Health Organization. (2021). Cancer. Retrieved September 23, 2021 from https://www.who.int/news-room/fact-sheets/detail/cancer.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 The Southern College Network Journal of Nursing and Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







