Development of a Thai Culturally - Based Mutual Support Group Program for Supporting the Elders with Behavioral and Psychological Symptoms of Dementia
Keywords:
Mutual Support, Thai Culture, Elders with BPSDAbstract
This research mainly consisted in the development of a mutual support group program, based on Thai culture, for supporting the elders with behavioral and psychological symptoms of dementia (BPSD). The development was divided in 3 phases. The first phase was to study the caring needs of elders with BPSD. Samples were selected by purposive sampling, for a group of 5 elders with BPSD and their family caregivers as well as 12 experts in dementia care. Data were collected by focus groups and analyzed by content analysis. The second phase was to develop a mutual support group program for the elders with BPSD, based on Thai culture. The third phase was to examine the effectiveness of the program on the quality of life the elders with BPSD. Thirty-two elders with BPSD and their family caregivers were randomly assigned to experiment and control groups so to compare the level of quality of life, which was measured by a quality of life questionnaire. Data were analyzed by paired t-test and Independent t-test. The results showed as follows.
1. Caring needs of the elders with BPSD consisted of: 1) enhancing their self-care skills, 2) encouraging emotional/stress management, 3) supporting social relationship skills, and 4) improving environmental management.
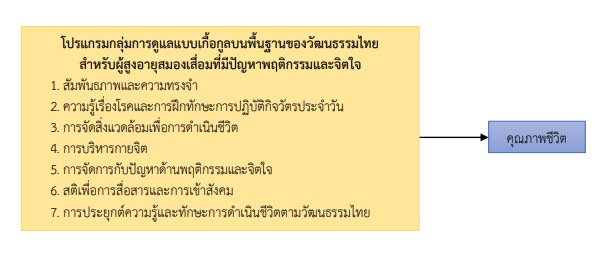
2. Thai culturally-based mutual support group program for supporting the elders with BPSD consisted of 7 activities of 60-90 minutes each, once a week, 2-3 activities each time, for a total of 3 weeks, as follows: 1) relationships and memory rehabilitation, 2) knowledge of disorder and activities of daily of life, 3) environmental management for lifestyle, 4) physical and mental exercises, 5) BPSD management in elderly with dementia, 6) mindfulness for communication and socialization, and 7) the application of knowledge and skills for lifestyle in Thai culture.
3. After 1 month participating in the program, the mean score of overall quality of life in experimental group was statistically significantly higher than control groups at .01 (t=3.139; p=002). The mean score of overall quality of life in the experimental group after 1 month participating in the program was statistically significantly higher than before participating the program at .001 (t=5.888; p<.001).
Enhancing the quality of life for elders with BPSD should consider a group therapy that both caregivers and elders with BPSD are mutually sharing experiences. The program should be consistent relevant to the culture of the elders with dementia.
References
Adlbrecht, L., Bartholomeyczik, S., Hildebrandt, C. & Mayer, H. (2021). Social Interactions of Persons with Dementia Living in Special Care Units in Long-Term Care: A Mixed-Methods Systematic Review. Dementia, 20(3), 967-984. http://doi: 10.1177/1471301220919937.
Baharudin, A. D., Din, N. C., Subramaniam, P. & Razali, R. (2019). The Associations Between Behavioral Psychological Symptoms of Dementia (BPSD) and Coping Strategy, Burden of Care and Personality Style among Low-Income Caregivers of Patients with Dementia. BMC Public Health, 19(Suppl 4), 447. http://doi.org/10.1186/s12889-019-6868-0.
Bandura, A. (1976). Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall.
Barreto, P. D, Demougeot, L., Pillard, F., Lapeyre-Mestre, M. & Rolland, Y. (2015). Exercise Training for Managing Behavioral and Psychological Symptoms in People with Dementia: A Systematic Review and Meta-Analysis. Ageing Research Reviews, 24, 274–285. http://doi: 10.1016/j.arr.2015.09.001
Bernard, H. (2000). Social Research Methods: Qualitative and Quantitative ApproachesSage, Thousand Oaks.
Braun, A., Trivedi, D. P., Dickinson, A. Hamilton, L., Goodman, C., Gage, H., et al. (2019). Managing Behavioural and Psychological Symptoms in Community Dwelling Older People with Dementia: A Systematic Review of Qualitative Studies. Dementia, 18(7–8), 2950–2970. http://doi: 10.1177/1471301218762856.
Chaichumni, N. (2014). The Effect of a Thai Culturally-Based Mutual Support Program on Social Functioning of Persons with Schizophrenia. (Unpublished Doctoral Dissertation). Prince of Songkla University, Songkhla, Thailand. (in Thai)
Chapman, K. R., Tremont, G., Malloy, P. & Spitznagel, M. B. (2020). The Role of Sexual Disinhibition to Predict Caregiver Burden and Desire to Institutionalize among Family Dementia Caregivers. Journal of Geriatric Psychiatry and Neurology, 33(1), 42–51. http://doi: 10.1177/0891988719856688
Chien, W. T., Norman, I. & Thompson, D. R. (2006). Perceived Benefits and Difficulties Experienced in a Mutual Support Group for Family Carers of People with Schizophrenia. Qualitative Health Research, 16(7), 962-981.
Chien, W. T. & Norman, I. (2009). The Effectiveness and Active Ingredients of Mutual Support Groups for Family Caregivers of People with Psychotic Disorders: A literature Review. International Journal of Nursing Studies, 46, 1604-1623. http://doi: 10.1016/j. ijnurstu. 2009.04.003
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences. (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers.
Douglass, C., Keddie, A., Brooker, D. & Surr, C. (2010). Cross-Cultural Comparison of the Perceptions and Experiences of Dementia Care Mapping "Mappers" in the United States and the United Kingdom. Journal of Aging and Health, 22(5), 567-588. http://doi:10.1177/0898264310362541
Feast, A., Orrell, M., Charlesworth, G, Melunsky, N., Poland, F. & Moniz-Cook, E. (2016). Behavioural and Psychological Symptoms in Dementia and the Challenges for Family Carers: Systematic Review. The British Journal of Psychiatry, 208, 429–434. http://doi: 10.1192/bjp.bp.114.153684
Forbes, D., Forbes, S. C, Blake, C. M., Thiessen, E. J. & Forbes, S. (2015). Exercise Programs for People with Dementia. Cochrane Database of Systematic Reviews, (4), CD006489. http://doi: 10.1002/14651858.CD006489.pub4.
Galinsky, M. J. & Schopler, J. H. (1995). Support Groups: Current Perspectives on Theory and Practice. New York, NY: Harworth Press.
Gitlin, L. N., Piersol, C. V., Hodgson, N., Marx, K., Roth, D. L., Johnson, D., et al. (2016). Reducing Neuropsychiatric Symptoms in Persons with Dementia and Associated Burden in Family Caregivers using Tailored Activities: Design and Methods of a Randomized Clinical Trial. Contemp Clin Trials, 49, 92–102. http://doi: 10.1016/j.cct.2016.06.006.
Hsu, T. J., Tsai, H. T., Hwang, A. C., Chen, L. Y. & Chen, L. K. (2017). Predictors of Non-Pharmacological Intervention Effect on Cognitive Function and Behavioral and Psychological Symptoms of Older People with Dementia. Geriatrics & Gerontology International, 17(Suppl 1), 28-35. http://doi: 10.1111/ggi.13037. PMID: 28436192.
Kerpershoek, L., de Vugt, M., Wolfs, C., Woods, B., Jelley, H., Orrell, M., et al. (2018). Needs and Quality of Life of People with Middle-Stage Dementia and Their Family Carers from the European Act if Care Study. When Informal Care Alone May Not Suffice. Aging & Mental Health, 22(7), 897-902. https://doi.org/10.1080/13607863.2017.1390732.
Livingston, G., Johnston, K., Katona, C., Paton, J. & Lyketsos, C. G. (2005). Systematic Review of Psychological Approaches to the Management of Neuropsychiatric Symptoms of Dementia. American Journal of Psychiatry, 162, 1996–2021.
Macleod, S. H., Elliott, L. & Brown, R. (2011). What Support can Community Mental Health Nurses Deliver to Carers of People Diagnosed with Schizophrenia? Findings from a Review of the literature. International Journal of Nursing Studies, 48(2011) 100–120. http://doi: 10.1016/j.ijnurstu.2010.09.005
Mahatnirunkul, S., Tantipiwattanaskul, W., Wongsuwan, K., & Prommanajirangkul, W. (1998). Comparison of the WHOQOL-100 and the WHOQOL-BREF (26items). Journal of Mental Health Thailand, 5, 4-15. (In Thai)
O'Dwyer, S. T., Moyle, W., Zimmer-Gembeck, M. & De Leo, D. (2016). Suicidal Ideation in Family Carers of People with Dementia. Aging and Mental Health, 20(2), 222-230. http://doi: 10.1080/13607863.2015.1063109.
Pijl-Zieber, E. M., Awosoga, O., Spenceley, S., Hagen, B., Hall, B. & Lapins, J. (2018). Caring in the Wake of the Rising Tide: Moral Distress in Residential Nursing Care of People Living with Dementia. Dementia, 0(0), 1–22. http://doi: 10.1177/1471301216645214
Phothisita, C. (2011). The Science and Art of Quality Study. (5th ed.). Bangkok: Amarin Print and Blushing. (In Thai)
Quinn, C., Clare, L. & Woods, R. T. (2015). Balancing Needs: The Role of Motivations, Meanings and Relationship Dynamics in the Experience of Informal Caregivers of People with Dementia. Dementia, 14(2), 220-237. http://doi. org/10.1177/1471301213495863
Schoenmakers, B., Buntinx, F. & DeLepeleire, J. (2010). Supporting the Dementia Family Caregiver: The Effect of Home Care Intervention on General Well-Being. Aging and Mental Health, 14, 44–56. http://doi: 10.1080/13607860902845533.
Sopina, E., Sorensen, J., Beyer, N., Hasselbalch, S. G. & Waldemar, G. (2017). Cost Effectiveness of a Randomized Trial of Physical Activity in Alzheimer's Disease: A Secondary Analysis Exploring Patient and Proxy-Reported Health-Related Quality of Life Measures in Denmark. BMJ Open, 7(6), e015217. http://doi: 10.1136/ bmjopen-2016-015217.
Yoddanan-Attigg, B. & Tangchonlatip, K. (2009). Qualitative Data Analysis: Recording Information, Interpreting and Finding Meaning. Bangkok: Chino. (In Thai)
Wilson, J. (1995). How to Work with Self-Help Group: Guidelines for Professionals’ Arena. Alder Shot, Hants: United State of Kingdom, England.
World Health Organization. (2017). Global Action Plan on the Public Health Response to Dementia 2017 – 2025, WHO Document Production Services, Geneva, Switzerland. Retrieved September 25, 2021, from https://apps.who.int/iris/bitstream/handle/10665/259615/9789241513487-eng.pdf
World Health Organization. (2021). Dementia: Fact Sheet. Retrieved September 25, 2021, from https://www.who.int/en/news-room/fact-sheets/detail/dementia.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 The Southern College Network Journal of Nursing and Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







