Clinical Factors Associated with Mortality among Patients with Leptospirosis: A Systematic Review
Keywords:
Leptospirosis, Clinical Signs and Symptoms, Clinical Complications, Mortality, Systematic ReviewAbstract
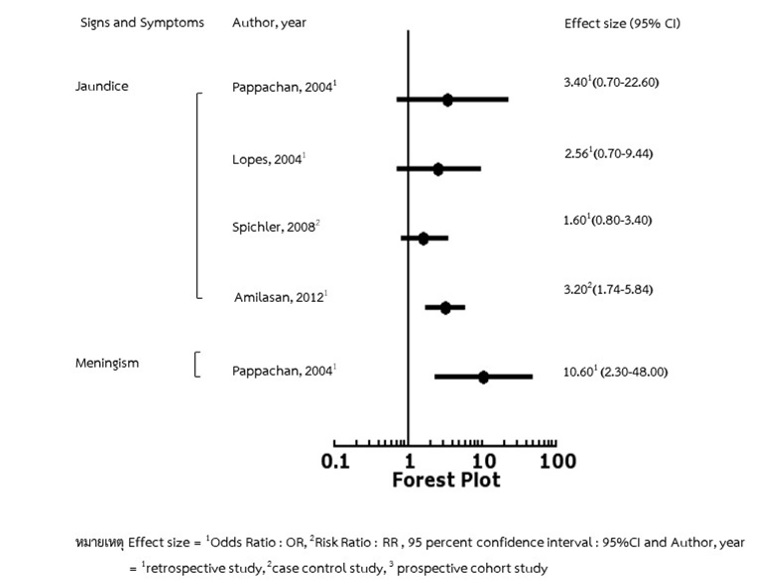
Leptospirosis is a blood infection caused by a bacteria. It is a zoonotic communicable disease that needs surveillance and that is a global health burden. Patients with leptospirosis who have severe clinical signs and symptoms and complication factors are more likely to die. This article aimed to review clinical factors associated with mortality among patients with leptospirosis. The published research articles were reviewed in national and international databases such as PubMed, Google Scholar, and ThaiJo Web of Science. There were 14 articles that were compatible with selection criteria and article quality assessment. Those were presented by forest plots which determined by effect size (Odds Ratio (OR) and Risk Ratio (RR)) and 95% confidence Interval (95%CI). The results of this review were classified into 2 factors associated with mortality consisting of 1) clinical sign and symptom factors, and 2) clinical complication factors. The clinical sign and symptom factors were jaundice and meningism. The clinical complication factors included oliguria, hypotension, dyspnea, hemoptysis, pulmonary disorder, thrombocytopenia, leukocytosis, hyperkalemia, hemorrhage, septic shock, and cirrhosis. Of those factors associated with mortality among patients with leptospirosis, medical and health professionals should implement the surveillance intensively for the clinical signs, symptom and complication factors in order to prevent severity and risk of mortality among patients with leptospirosis.
References
Amilasan, A. T., Ujiie, M., Suzuki, M., Salva, E., Belo, M. C.P., Koizumi et al. (2012). Outbreak of Leptospirosisafter Flood, the Philippines, 2009. Emerging Infectious Diseases, 18, 1.
Bureau of General Communicable Disease, Department of Disease Control, Ministry of Public Health. (2015). Handbook for Leptospirosis Disease; Agricultural Cooperative Assembly of Thailand. ISBN: 978-616-11-2536-3. (in thai)
Daher, E., Zanetta, D., Avalcante, M., & Abdulkader, R. (1999). Risk Factors For Death And Changing Patterns in Leptospirosis Acute renal Failure. The American Society of Tropical Medicine and Hygiene. The American Journal of Tropical Medicine and Hygiene, 61(4), 630–634.
Daher, E. F., Silva Junior, G. B., Silveira, C. O., Falcao, F.S., Alves, M. P., Mota, J. A., et al., (2014). Factors Associated with Thrombocytopenia in Severe Leptospirosis (Weil’s disease). Clinics, 69(2), 106-110.
Department of Disease Control, Bureau of Epidemiology. (2015). Surveillance Database. Retrieved June 30, 2019 from https://apps.boe.moph.go.th/ (in Thai).
Department of Disease Control, Ministry of Public Health. (2017). Document for Leptospirosis Symposium 2017. (pp. 14). Nakhon Si Thammarat. Graphics and design font. (in Thai)
Dolhnikoff, M., Mauad, T., Bethlem, E., & Carvalho, C. (2007). Pathology and Pathophysiology of Pulmonary Manifestations in Leptospirosis. The Brazilian Journal of Infectious Diseases, 11, 142-8.
Dupont, H., Perdrizet, D., Zehner, J., Jarrige, B., & Daijardin, J. (1997). Leptospirosis: Prognostic Factors Associated with Mortality. French. Clinical Infectious Diseases, 25, 720–4.
Esen, S., Sunbul, M., Leblebicioglu, H., Eroglu, C., & Turan, D. (2004). Impact of Clinical and Laboratory Findingson Prognosis in Leptospirosis. Swiss Medical Weekly, 134, 347-352.
Galdino, G., Silva G., Rocha, H., Mendes, M., Guimaraes, M., Miranda, T., et al. (2016). Predictors of Acute Kidney Injury and Mortality in Severe Leptospirosis (Weil Disease). Nephrology Dialysis Transplantation, 31, 151.
Goyal, O., Kaur, D., Goyal, P., & Chhina, R. (2016). Hepatic Dysfunction and Predictors of Mortality in Leptospirosis: A Re-Emerging Tropical Disease in Northern India. Tropical Gastroenterology, 37(4), 248-257.
Hartskeerl, R. A., Collares-Pereira, M., & Ellis, W. A. (2011) Emergence, Control and Re-Emerging Leptospirosis: Dynamics of Infection in the Changing Word. Clinical Microbiology and Infection, 17(4), 494-501.
Hinjoy, S. (2014) Epidemiology of Leptospirosis from Thai National Disease Surveillance System, 2003-2012. Outbreak, Surveillance, Investigation & Response, 7(2), 1-5.
Janwitthayan, W. (2015). Leptospira Collagenase Gene Cloning and Protein Production for Enzymatic Activity and Immunoreactivity Study. Chilalongkorn University Intellectual Repository. Retrieved June 30, 2019 from http://cuir.car.chula.ac.th/handle/123456789/50245. (in Thai)
Krairotchananan, P., (2017). “Leptospirosis (LEPTOSPIROSIS). In Khunchoo N., Sanhea P.” Document for Leptospirosis Symposium 2017. (pp. 20). Bankkok: Aksorn Graphic and Design Company. (in Thai)
Lopes, A., Costa, E., Costa, Y., Sacramento, E., Oliveira, A., Lopes, M. et al. (2004). Comparative Study of the in-Hospital Case-Fatality Rate of Leptospirosis Between Pediatric and Adult Patients of Different Age Groups. Revista do Instituto de Medicina Tropical de São Paulo, 46(1), 19-24
Marotto, P., Ko, A., Nascimento, C., Seguro, A., Prado, R., Barbosa, et al., (2010). Early Identification of Leptospirosis-Associated Pulmonary Hemorrhage Syndrome by Use of a Validated Prediction Model. The Brazilian Journal of Infectious Diseases, 60(3), 218-223
Marotto, P., Nascimento, C., Neto, J., Marotto, M., Andrade, L., Sztajnbok, J., et al. (1999). Acute Lung Injury in Leptospirosis: Clinical and Laboratory Features, Outcome, and Factors Associated with Mortality. Brazil. The Infectious Diseases Society of America. Clinical Infectious Diseases, 29, 1561-3
Panaphut, T., Domrongkitchaiporn, S., & Thinkamrop, B. (2002). Prognostic Factors of Death in Leptospirosis: a Prospectivecohort Study in Khon Kaen, Thailand. International Journal of Infectious Diseases, 6, 52-59.
Pappachan, M., Mathew, S., Aravindan, K., Khader, A., Bharghavan, P., Kareem, M., et al. (2004). Risk Factors for Mortality in Patients with Leptospirosis During an Epidemic in Northern Kerala. The National Medical Journal of India, 17, 240–243
Petchkanchanaphong, W. (2019). General Knowledge about Infectious Diseases and Carriers Leptospirosis (Leptospirosis). Infectious and Carrier Disease Information Center. Retrieved July 5, 2019 from http://webdb.dmsc.moph.go.th/ifc_nih/a_nih_1_ 001c.asp?info_id=214 (in Thai)
Pottha, U., & Amphon, K. (1970). Leptospirosis in Thailand. Journal of Medical Technology Chiang Mai, 3, 1 (in Thai)
Saokaew, S., & Sumsiwan, N. (2014). Critical Reading of Health Research. Naresuan Phayao Journal, 7(3), 286-297. (in Thai)
Saraya, S. (2015). Disease During the Flood (Part 3) Leptospirosis. Retrieved September 3, 2019 from www.pharmacy.mahidol.ac.th. (in thai)
Siriwanij, T., Suttinont, C., Tantawichien, T., Chusil, S., Kanjanabuch, T., & Sitprija, V. (2005). Haemodynamics in Leptospirosis: Effects of Plasmapheresis and Continuous Venovnoushaemofiltration. Nephrology (Carlton), 10, 1-6
Spichler, A. S., Vilaca, P. J., Athanazio, D. A., Albuquerque, J. O., Buzzar, M., Castro, B., et al., (2008). Predictors of Lethality in Severe Leptospirosis in Urban Brazil. The American Society of Tropical Medicine and Hygiene, 79, 911-914
Surasak, S., & Nathapol, S. (2014). Critical Appraisal for Health Research Articles. Naresuan Phayao Journal, 7(1), 286-297. (in Thai)
Tangkanakul, W., Tharmaphornpil, P., Plikaytis, B., Bragg, S., Boonsuksombat, D., Choomkasien, P. (2000). Risk with Leptospirosis in Northeastern Thailand. The American Journal of Tropical Medicine and Hygiene, 63(3, 4), 204-208.
Terpstra, W. J. (2003). Human Leptospirosis: Guildance for Diagnosis, Surveillance and Control. World Health Organization. Retrieved June 30, 2019 from http://whqlibdoc.who.int
The Joanna Briggs Institute. (2017). Critical Appraisal Tools. Retrieved July 5, 2019 from http://joannabriggs.org /research/critical-appraisal-tools.html.
Thipmontree, W., Suputtamonkul, Y., Tantibhedhyangkul, W., Suttinont, C., Wongswat, E., & Silpasakorn, S. (2014). Human Leptospirosis Trends: Northeast Thailand, 2001-20012. International Journal of Environtmental and Public Health, 11, 8542-8551.
Wang, H., Lee, M., Chen, Y., Hsueh, P., & Chang, S. (2018). Factors Associated with Severity and Mortality in Patients with Confirmed Leptospirosisat a Regional Hospital in Northern Taiwan, Journal of Microbiology, Immunology and Infection, 1-8.
Wilairat, P. (2008). Leptospirosis.Faculty of Tropical Medicine, Mahidol University. Retrieved July 5, 2019 from https: //www.tm.mahidol.ac.th/clinic/? Q = th% 2FLepto. (in Thai)
World Health Organization (WHO). (2009). Estimating the Global Burden of Human Leptospirosis. Retrieved June 30, 2019 from https://www.who.int/zoonoses/ diseases/Lerg_brochure.pdf.
Zetun, C., Hoffmann, J., Silva, R., Souza, L., & Langoni, H. (2009). Leptospira spp. And Toxoplasma Gondii Antibodies in Vampire bats (Desmodus rotundus) in Botucatu Region, SP, Brazil. International Journal of Medical Microbiology and Tropical Diseases, 15, 546-552.
Downloads
Published
Issue
Section
License
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







