Clinical Complication Factors Associated with Mortality Patients with Dengue Hemorrhagic Fever (DHF): A Literature Review
Keywords:
Dengue Hemorrhagic Fever, DHF, Complications, Mortality, Clinical Complications, Literature ReviewAbstract
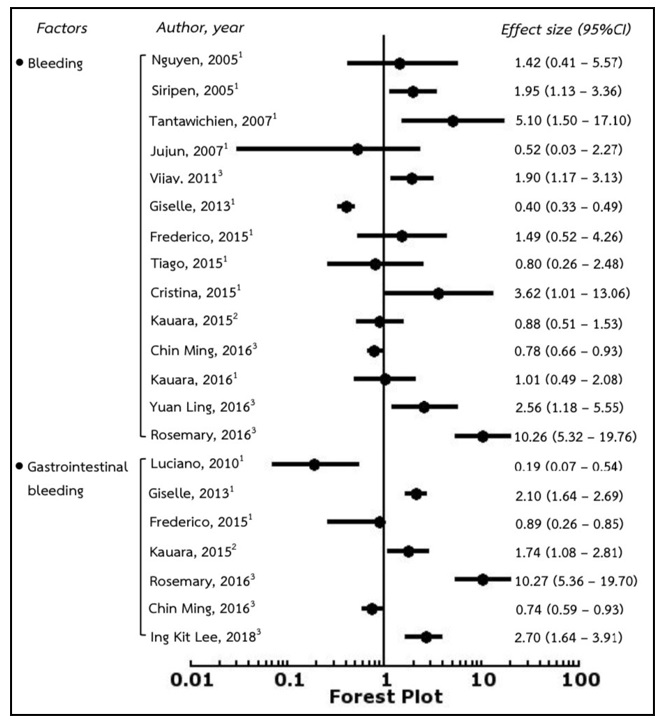
Dengue hemorrhagic fever (DHF) remains a major medical and public health problem in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Individuals diagnosed with DHF are more likely to die in case of lacking to access medical health services and receiving appropriate medical care immediately. The purpose of this article aimed to present a literature review related to clinical complication factors associated with mortality among patients with DHF. Thai national and international databases were systematically reviewed from Pubmed, Scopus, Mathscinet, ERIC and Web of Science. The results of reviewing related to clinical complication factors were presented as forest plot (or blobbogram) by determining odds ratio (OR) and 95% confidence interval (95%CI) from those reviewed research articles. Results revealed that clinical complication factors associated with mortality among patients with dengue hemorrhagic fever are as following: bleeding, plasma leakage, ascites, fluid overload, pleural effusion, prolonged shock, serous space, liver abscess, hepatic encephalopathy, hepatic failure, hepatomegaly, septic shock, acute kidney injury, nosocomial infection, and respiratory failure. Therefore, medical and health professionals should intensively attend patients with dengue hemorrhagic fever in order to surveillance those clinical complication factors associated with mortality.
References
Chaimay, B. (2019). Public Health Research Methods. (4th ed.). Songkhla: Numsin Advertisement. (in Thai)
Chin-Ming, C., Khee-Siang, C., Wen-Liang, Y., Kuo-Chen, C., Hui-Chun, C., Chiu-Yin, Y., et al. (2016). The Outcomes of Patients with Severe Dengue Admitted to Intensive Care Units. Medicine, 95, 1-5.
Cristina, G., Miyuru, C., Layani, C., Shirom, S. & Lakmini, W. (2015). Delayed Anxiety and Depressive Morbidity among Dengue Patients in a Multi‑Ethnic Urban Setting: First Report from Sri Lanka. Int J Ment Health Syst, 20, 1-7.
Department of Disease Control, Bureau of Epidemiology. (2019). Surveillance Database. Retrieved May 30, 2019 from https://apps.boe.moph.go.th/.
Frederico, A., Tiago, P., Cristina, H., Liliane, B., Daniela, P., Claudio, D., et al. (2015). Clinical Profiles and Factors Associated with Death in Adults with Dengue Admitted to Intensive Care Units Minas Gerais Brazil. Plos one, 10(1), 1-16.
Giselle, H, Eliane, D., & Elisabeth, C. (2013). Determinants of Mortality From Severe Dengue in Brazil: A Population-Based Case-Control Study. The American Society of Tropical Medicine and Hygiene, 88(1), 670-676.
Health Intervention and Technology Assessment Program. (2017). Health Technology Assessment Database in Thailand Health Technology Assessment Program and Policy. Nonthaburi. (in Thai)
Ing-Kit, L., Chung-Hao, H., Wen-Chi, H., Yi-Chun, C., Ching-Yen, T., Chang, K., et al. (2018). Prognostic Factors in Adult Patients with Dengue: Developing Risk Scoring Models and Emphasizing Factors Associated with Death 7 Days After Illness Onset and 3 Days After Presentation. Journal of Clinical Medicine, 396(1), 15-30.
Jirakanjanakit, N., Sanohsomneing, T., Yoksan, S., & Bhamarapravati, N. (2014). The Micro-Focus Reduction Neutralization Test for Determining Dengue and Japanese Encephalitis Neutralizing Antibodies in Volunteers Vaccinated Against Dengue. Trans Roy Soc Trop Med Hyg, 91(1), 614-617.
Jujun, J., Herry, G., & Djatnika, S. (2007). Clinical Risk Factors for Dengue Shock Syndrome in Children. Paediatr Indones, 47(1), 7-11.
Kalayanarooj, S. (2011). Dengue Classification: Current WHO VS. The Newly Suggested Classification For Better Clinical Application?. Journal of Med Assoc Thailand, 94(3), 74-84.
Kalayanarooj, S., Vangveeravong, M., & Vatcharasaevee, V. (2014). Clinical Practices Guidelines of Dengue, Dengue Hemorrhagic Fever for Asian Economic Community. Bangkok Medical Publisher, 4(1), 607-611.
Kauara, C., Ahmed, M., Husain, S., Frederico, F., & Valdelaine, E. (2016). Dengue Related Deaths at Ibn-Sina Hospital- Al-Mukalla: Causes and Alarming Signals. Copyright IMedPub, 16(1), 1-7.
Kauara, C., Frederico, F., Valdelaine, E., & Mari, C. (2015). Factors Associated with Death From Dengue in the Atate of Minas Gerais, Brazil: Historical Cohort Study. Tropical Medicine and International Health, 20(1), 211-218.
Khun, S., & Manderson, L. (2007). Health Seeking and Access to Care For Children with Suspected Dengue in Cambodia: an Ethnographic Study. BMC Public Health, 7(1), 262-269.
Luciano, P., Castelo, B., Dina, C., Susana, H., Kiliana, N., & Reinaldo, S. (2010). Clinical and Epidemiological Characterization of Dengue Hemorrhagic Fever Cases in Northeastern, Brazil. Revista Da Sociedade Brasileira De Medicina Tropical, 43(1), 355-358.
Luciano, P., Narayan, G., & Andrew, W. (2009). Diagnosis of Dengue: Strengths and Limitations of Current Techniques and Prospects for Future Improvements. Licensee InTech, 3(1), 56-73.
Muhammad, K., Jackson, T., Ashhad, U., Safia, A., & Manickam, R. (2014). Predictors of Hospital Stay and Mortality in Dengue Virus Infection-Experience from Aga Khan University Hospital Pakistan. BMC Research Notes, 473(1), 1-7.
Nguyen, T., Trong, L., Huan-yao, L., Lebich, L., Kao-jean, H., Chiou, F., et al. (2005). Association Between Sex Nutritional Status Severity of Dengue Hemorrhagic Fever and Immune Status in Infants with Dengue Hemorrhagic Fever. Am. J. Trop. Med. Hyg, 72(1), 370-374.
Rismala, D., Alan, R., & Damayanti, R. (2006). Clinical Features of Dengue Hemorrhagic Fever and Risk Factors of Shock Event. Paediatrica Indonesiana, 46(1), 144-148.
Rosemary, C., Daniel, B., Bernardino, C., Vanderson, S., Ricardo, A., Cristiano, F., Megumi, S., & Jose, B. (2016). Mortality Predictors in Patients with Severe Dengue, Brazil. PLOS ONE, 1884, 1-10.
Shigeki, H., Charnchudhi, C., Dusit, S., Indhira, K., Arino, Y., & Tadashi, S. (2008). Clinical Features and Differences between Child and Adult Dengue Infection in Rayong Province, Southeast Thailand. Southeast ASIAN J Trop Med Public Health, 39(1), 252-259.
Shi-Yu, H., Ing-Kit, L., Jien-Wei, L., Chia-Te, K., & Lin, W. (2015). Clinical Features of and Risk Factors for Rhabdomyolysis among Adult Patients with Dengue Virus Infection. The American Society of Tropical Medicine and Hygiene, 92(1), 75-81.
Siripen, K., & Suchitra, N. (2005). Is dengue Severity Related to Nutritional Status?. Arch Pathol Lab Med, 36(1), 378-384.
Siripen, K., Wangerawong, K., & Warunee W. (2013). Guidelines for Diagnosis and Treatment of Dengue Hemorrhagic Fever HM the King's 80th Birthday Anniversary. (2th ed.). Queen Sirikit National Institute of Child Health, Department of Medical Services, and Ministry of Public Health. (in Thai)
Surasak, S., & Nathapol, S. (2014). Critical Appraisal for Health Research Articles. Naresuan Phayao Journal, 7(1), 286-297.
Tantawichien, T. (2007). Dengue Fever and Dengue Hemorrhagic Fever in Adolescents and Adults. Paediatrics and International Child Health, 32(10), 22-27.
Tauqeer, H., Amer, H., Azmi, S., Azreen, S., & Yusra, H. (2017) Determinants of Mortality and Prolonged Hospital Stay among Dengue Patients Attending Tertiary Care Hospital: A Cross-Sectional Retrospective Analysis. BMJ Open, 1136, 1-12.
Thisyakorn, U., & Thisyakorn, C. (2014) Dengue Hemorrhagic Fever. In: Dupont HL, Steffen R, eds. Textbook of Travel Medicine and Health. B.C. Decker Inc, 52(3), 312-314.
Tiago, R., Antonio, G., Cedric, J., Catherine, A., Rochea, M., Adrian, R., et al. (2015). Nonlinear and Delayed Impacts of Climate on Dengue Risk in Barbados: A Modelling Study. Plos Medicine, 10(1), 1-24.
Tiawilai, A. (2013). Degue during Infancy. Thai J Pedriatr, 52(1), 56-60. (in Thai)
Vijay, G., Tribhuvan, P., Ravindra, M., Aaradhna, S., Meetu, G., Pradeep, K., et al. (2011). Risk Factors of Dengue Shock Syndrome in Children. Journal of Tropical Pediatrics, 57(1), 451-456.
Voranush, C., Yanee, H., & Yong, P. (2009). Liver Function Test Results and Outcomes in Children with Acute Liver Failure Due to Dengue Infection. Southeast ASIAN J Trop Med Public Health, 40(1), 47-53.
World health Organization. (2012). Handbook for Clinical Management of Dengue. Geneva: WHO, p.1-10.
Yamada, K., Takasaki, T., Nawa, M., Kurane, I. & Yamada, K. (2012). Virus Isolation as One of The Diagnostic Methods for Dengue Virus Infection. Journal Clin Virol, 24(3), 203-209.
Yuan-Liang, W., Chee-Peng, H., Narwani, H., Ariza, Z., Pik Pin, G., & Wee-Kooi, C. (2016). A Two-Year Review on Epidemiology and Clinical Characteristics of Dengue Deaths in Malaysia, 2013-2014. PLOS Neglected Tropical Diseases, 1371, 1-16.
Yuwadee, K. (2016). Comparison of Clinical Features of Dengue Fever and Dengue Hemorrhagic Fever in Pediatric Patients in Phatthalung Hospital. Medical Journal, 30(1), 139-147. (in Thai)
Downloads
Published
Issue
Section
License
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารเครือข่าย วิทยาลัยพยาบาลและการสาธารณสุขภาคใต้ ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการหรือเครือข่ายวิทยาลัยพยาบาลและวิทยาลัยการสาธารณสุขภาคใต้ ไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารเครือข่ายวิทยาลัยพยาบาลและการสาธารณสุขภาคใต้







