สถานการณ์วัณโรคของอำเภอแม่ทะ จังหวัดลำปาง
คำสำคัญ:
วัณโรค, สถานการณ์, การวินิจฉัยบทคัดย่อ
การวิจัยครั้งนี้เป็นการศึกษาเชิงพรรณนาแบบย้อนหลัง (Retrospective Study) มีวัตถุประสงค์เพื่ออธิบายลักษณะทั่วไปของผู้ป่วยวัณโรคในอำเภอแม่ทะ จังหวัดลำปาง จำนวน 239 คน ที่ได้รับการวินิจฉัยเป็นวัณโรคและได้ขึ้นทะเบียนรักษาวัณโรคที่โรงพยาบาลแม่ทะในช่วงเวลา ตั้งแต่วันที่ 1 ตุลาคม พ.ศ. 2557 – 30 กันยายน พ.ศ. 2561 เก็บรวบรวมข้อมูลจากการทบทวนข้อมูลเวชระเบียน
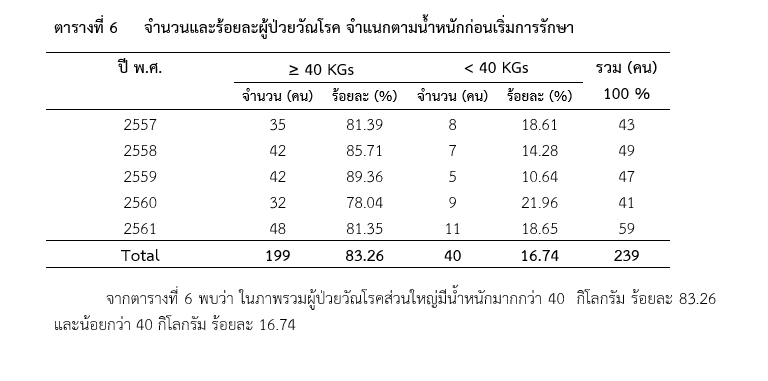
ผลการศึกษา พบว่า ผู้ป่วยวัณโรคเป็นเพศชาย ร้อยละ 79.50 เพศหญิง ร้อยละ 20.50 พบผู้ป่วยวัณโรค ที่มีน้ำหนักน้อยกว่า 40 กิโลกรัม ร้อยละ 16.74 ส่วนใหญ่ผู้ป่วยวัณโรคอยู่ในกลุ่มผู้สูงอายุที่มีอายุมากกว่า 60 ปี ร้อยละ 59.83 และเป็นผู้ป่วยวัณโรคประเภทวัณโรคปอดเสมหะพบเชื้อ ร้อยละ 83.68 ในกลุ่มผู้ป่วยวัณโรคปอดพบว่า ร้อยละ 67.94 ได้รับวินิจฉัยจากการตรวจเสมหะด้วยวิธี direct smear พบเชื้อ Acid fast bacilli (AFB) ร้อยละ 17.71 ได้รับการวินิจฉัยโดยใช้วิธีการตรวจหาโมเลกุลของเชื้อวัณโรค (Xpert MTB/RIF) และร้อยละ14.35 ได้รับการวินิจฉัยจากการตรวจเสมหะด้วยวิธี direct smear ให้ผล Acid fast bacilli (AFB) เป็นลบ นอกจากนี้ พบอุบัติการณ์การติดเชื้อเอชไอวีในผู้ป่วยวัณโรค ร้อยละ 2.93 อัตราผลสำเร็จของการรักษาน้อยกว่าร้อยละ 85 และอัตราการเสียชีวิตมากกว่าร้อยละ 10
การดำเนินงานด้านวัณโรคในอำเภอแม่ทะ จังหวัดลำปาง ยังไม่เป็นไปตามเป้าหมายตามที่กระทรวงสาธารณสุขกำหนดไว้ โดยเฉพาะตัวชี้วัดผลสำเร็จของการรักษาที่ต้องมากกว่าร้อยละ 85 และอัตราการเสียชีวิตน้อยกว่าร้อยละ 5 ดังนั้น ผู้ดำเนินงานด้านวัณโรคและผู้เกี่ยวข้องอื่นๆ กับผู้ป่วยวัณโรคทั้งในสถานบริการสุขภาพและชุมชน ควรได้มีส่วนร่วมวิเคราะห์ปัญหา สาเหตุ และแนวทางดำเนินการร่วมกันเพื่อให้เป็นไปตามเป้าหมายและพัฒนาคุณภาพชีวิตของผู้ป่วยวัณโรค ครอบครัว และชุมชน
เอกสารอ้างอิง
Department of Disease Control, Ministry of Public Health. (2018).National Tuberculosis Control Programme Guideline, Thailand, 2018. Bangkok: Aksorn Graphic and Design Publication Limited Partnership. (in Thai).
Iemrod K., Swaddiwudhipong† W. (2017). Situation of Tuberculosis among Hospital Personnel of the Ministry of Public Health, Tak Province. Journal of Healh Systems Research. 11(2), 286-295. (in Thai).
Khonsomsak R. (2017). Factors Associated with Mortality in Smear Positive Pulmonary Tuberculosis in Somdejprayanasangworn hospital, Chiangrai Province. Chiangrai Medical Journal. 9 (1). 19-27. (in Thai).
Lampang Provincial Health Office. (2017). Provincial Inspection Form, Fiscal Year 2018. Lampang: Lampang Provincial Health Office. (in Thai).
Makmuang J., et al. (2016). Factors Associated with Mortality rate in Tuberculosis Patients at Phayao Hospital. Chiangrai Medical Journal. 8(1) 53-59. (in Thai).
Malathum K.,et al.(2007). Infectious diseases in the elderly. Ramathibodi Nursing Journal.13(3), 272-287.
Mungkhetklang V., et al. (2016). Causes and Determinant Factors of Death among Tuberculosis Patients during Treatment in Khonkaen Province,Fiscal Year 2009 -2010.Journal of the office of DPC 7 Khon Kaen.23(1),22-34.(in Thai).
Prasopsuk K.(2018). Prevention and control of tuberculosis in Thailand. Nonthaburi: Strategy and Plannind Division, Office of the Minister, Ministry of Public Health. (in Thai).
Sae-tung J. (2017). Characteristics and risk factors associated with death during tuberculosis treatment among new patients with pulmonary tuberculosis in the Upper North of Thailand, year 2005-2014. Disease Control Journal. 43(4);436-447. (in Thai).
Tuberculosis Clinic, Mae Tha Hospital. (2018). Mae Tha Hospital Tuberculosis report and TBCMThailand Programe. Lampang: Lampang Provincial Health Office. (in Thai).
Wannaphongsapak A., Moonfong K.(2017). Patients’ characteristic and factors related to causes of death in new pulmonary Tuberculosis Patients in Lamphun Province. Lanna Public Health Journal.13(2); 72-85. (in Thai).
ดาวน์โหลด
เผยแพร่แล้ว
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารวารสารวิชาการสุขภาพภาคเหนือ ถือเป็นลิขสิทธิ์ของวารสารวารสารวิชาการสุขภาพภาคเหนือ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากวารสารวารสารวิชาการสุขภาพภาคเหนือก่อนเท่านั้น
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารวิชาการสุขภาพภาคเหนือถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
อนึ่ง ข้อความและข้อคิดเห็นต่างๆ เป็นของผู้เขียนบทความนั้นๆ ไม่ถือเป็นความเห็นของวารสารฯ และวารสารฯ ไม่จำเป็นต้องเห็นด้วยกับข้อความและข้อคิดเห็นใดๆ ของผู้เขียน วารสารฯ ขอสงวนสิทธิ์ในการพิจารณาตีพิมพ์ตามความเหมาะสม รวมทั้งการตรวจทานแก้ไขหรือขัดเกลาภาษาให้ถูกต้องตามเกณฑ์ที่กำหนด


