ผลของแนวปฏิบัติการจัดการความปวดและเพิ่มการเคลื่อนไหวของลำไส้ ในผู้ป่วยหลังผ่าตัดเปิดช่องท้องแบบเร่งด่วน
คำสำคัญ:
แนวปฏิบัติการพยาบาล, การจัดการความปวด, การเคลื่อนไหวของลำไส้, การผ่าตัดเปิดช่องท้องแบบเร่งด่วน, การฟื้นตัวหลังผ่าตัดบทคัดย่อ
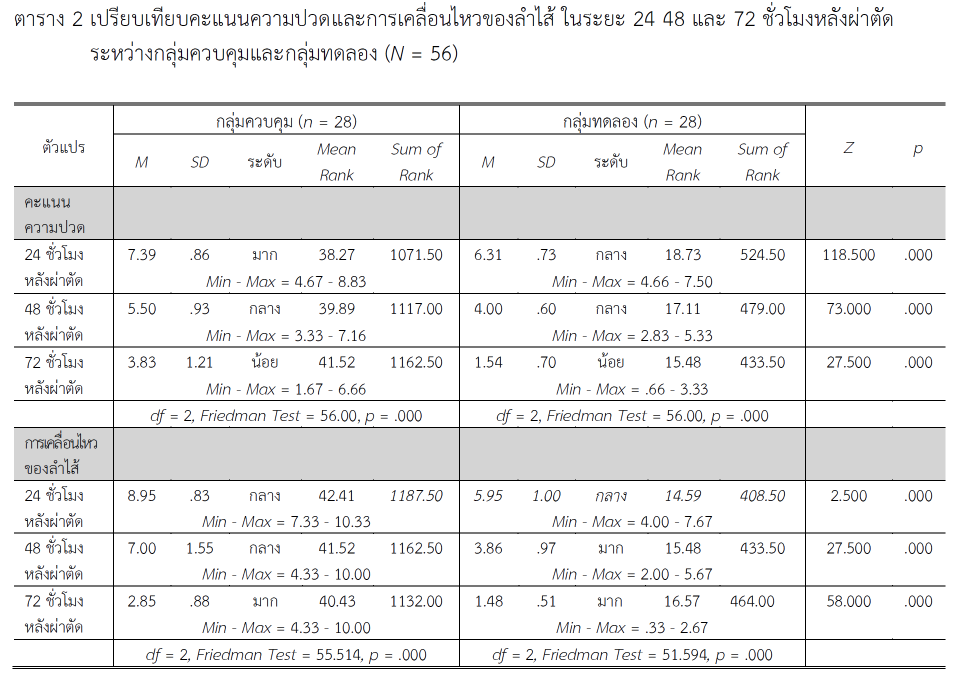
การวิจัยกึ่งทดลองครั้งนี้มีวัตถุประสงค์เพื่อเปรียบเทียบคะแนนความปวด การเคลื่อนไหวของลำไส้ จำนวนวันนอนโรงพยาบาล และค่าใช้จ่ายการรักษาพยาบาล ระหว่างกลุ่มทดลองที่ได้รับแนวปฏิบัติการจัดการความปวดและเพิ่มการเคลื่อนไหวของลำไส้ที่พัฒนาขึ้น กับกลุ่มควบคุมที่ได้รับการดูแลตามแนวปฏิบัติมาตรฐานของโรงพยาบาล ในผู้ป่วยหลังผ่าตัดเปิดช่องท้องแบบเร่งด่วน ตัวอย่างเป็นผู้ป่วยหลังผ่าตัดเปิดช่องท้องแบบเร่งด่วนที่เข้ารับการรักษาในหอผู้ป่วยศัลยกรรมชาย 1 โรงพยาบาลพระนารายณ์มหาราช จังหวัดลพบุรี จำนวน 56 ราย แบ่งเป็นกลุ่มทดลองและกลุ่มควบคุม กลุ่มละ 28 ราย กลุ่มควบคุมได้รับการดูแลตามแนวปฏิบัติมาตรฐาน ขณะที่กลุ่มทดลองได้รับแนวปฏิบัติที่เน้นการใช้ยาแก้ปวดร่วมกับการฝึกหายใจ การเคี้ยวหมากฝรั่ง และการกระตุ้นการเคลื่อนไหวร่างกาย ในระยะ 24 48 และ 72 ชั่วโมงหลังผ่าตัด เครื่องมือที่ใช้ในการเก็บข้อมูลเป็นแบบบันทึกข้อมูลส่วนบุคคล ความปวด การเคลื่อนไหวของลำไส้ ระยะเวลานอนโรงพยาบาล และค่าใช้จ่ายการรักษาพยาบาล การวิเคราะห์ข้อมูลโดยใช้สถิติเชิงพรรณนา และสถิติไม่อิงพารามิเตอร์ ได้แก่ แมน-วิทนีย์ ยู ไค-สแควร์ ฟรีดแมน และการวิเคราะห์สัมประสิทธิ์สหสัมพันธ์ของสเปียร์แมน
ผลการวิจัยพบว่า กลุ่มทดลองมีค่ามัธยฐานคะแนนความปวดในระยะ 24 48 และ 72 ชั่วโมงหลังผ่าตัด เท่ากับ 6.33 (ระดับปานกลาง) 4.00, (ระดับปานกลาง) และ 1.33 (ระดับน้อย) ตามลำดับ ซึ่งต่ำกว่ากลุ่มควบคุมอย่างมีนัยสำคัญทางสถิติ (p < .05) โดยมีค่าสถิติ Z = 118.50, 73.00 และ 27.00 ตามลำดับ การเคลื่อนไหวของลำไส้ในกลุ่มทดลองมีค่ามัธยฐานเท่ากับ 5.83 (ระดับปานกลาง), 3.66 (ระดับมาก) และ 1.33 (ระดับมาก) ซึ่งดีกว่ากลุ่มควบคุมอย่างมีนัยสำคัญทางสถิติ (Z = 2.50, 27.50 และ 58.00 ตามลำดับ; p < .05) อย่างไรก็ตาม จำนวนวันนอนโรงพยาบาลและค่าใช้จ่ายการรักษาพยาบาลของทั้งสองกลุ่มไม่มีความแตกต่าง อย่างมีนัยสำคัญทางสถิติ (p > .05)
ผลการศึกษานี้สนับสนุนว่า แนวปฏิบัติที่พัฒนาขึ้นสามารถนำไปใช้กับผู้ป่วยกลุ่มนี้ได้อย่างเหมาะสม โดยเฉพาะในสถานพยาบาลที่ต้องการลดความปวดและเร่งการฟื้นฟูการทำงานของลำไส้ภายหลังการผ่าตัดได้อย่างมีประสิทธิภาพ
Downloads
เอกสารอ้างอิง
Anekar, A. A., & Cascella, M. (2021). WHO analgesic ladder. In StatPearls. StatPearls Publishing.
Aydemir, M., & Asgarpour, H. (2020). Effects of mechanical bowel preparation on physiological parameters of patients undergoing elective colorectal surgery: A quasi-experimental hospital-based study. International Journal of Caring Sciences, 13(1), 73-80.
Campbell, T. S., Johnson, J. A., & Zernicke, K. A. (2020). Gate control theory of pain. In Encyclopedia of behavioral medicine. Springer International Publishing, 914-916.
Dias, K. J., & Ferreira, G. (2022). Anatomy of the cardiovascular and pulmonary systems. Essentials of cardiopulmonary physical therapy (pp. 1-28) (5th ed.). St. Louis, Missouri: Elsevier.
El-Shewy, A. H., Abdalla, W. M., & Baghdadi, M. A. (2020). Enhanced recovery after surgery protocol in colorectal surgery. The Egyptian Journal of Surgery, 39(1), 94-101.
Gangamma, K., Manoj, P., & Shashikumar, H. B. (2022). Post-operative complications rates in patients undergoing emergency laparotomy in tertiary care hospital. Asian Journal of Medical Sciences, 13(4), 177-181.
Harnsberger, C. R., Maykel, J. A., & Alavi, K. (2019). Post operative ileus. Clinics in Colon and Rectal Surgery, 32(3), 166-170.
Hendriksen, B. S., Keeney, L., Morrell, D., Candela, X., Oh, J., Hollenbeak, C. S., & Amponsah-Manu, F. (2020). Epidemiology and perioperative mortality of exploratory laparotomy in rural Ghana. Annals of Global Health, 86(1), 1-7.
Jafari, H., Courtois, I., Van den Bergh, O., Vlaeyen, J. W., & Van Diest, I. (2017). Pain and respiration: A systematic review. Pain, 158(6), 995-1006.
Jaywant, S. S., & Pai, A. V. (2003). A comparative study of pain measurement scales in acute burn patients. The Indian Journal of Occupational Therapy, 35(3), 13-17.
Joseph, A. E., Moman, R. N., Barman, R. A., Kleppel, D. J., Eberhart, N. D., Gerberi, D. J., & Hooten, W. M. (2022). Effects of slow deep breathing on acute clinical pain in adults: A systematic review and meta-analysis of randomized controlled trials. Journal of Evidence-Based Integrative Medicine, 27(1), 1-10. https://www.doi.org/10.1177/2515690X221078006
Karabulut, İ., Yılmaz, A. H., & Yılmazel, F. (2020). The efficacy of chewing gum in postoperative ileus management after robot assisted laparoscopic radical prostatectomy: A prospective randomized study. Journal of Contemporary Medicine, 10(1), 96-101.
Khoyun, S., Poothawee, W., & Srisoy, A. (2019). Effect of post-operative recovery program with the use of easy walk equipment to prevent complications in abdominal surgery patients. Srinagarind Medical Journal, 34(4), 386-392.
Koesanthia, S., Wongkongkam, K., Danaidutsadeekul, S., & Thawitsri, T. (2022). Impact of early mobility programme on open abdominal surgery patients’ post-operative bowel function recovery during the first 72 hours. Journal of Thailand Nursing and Midwifery Council, 37(2), 61-80.
Mendell, L. M. (1966). Physiological properties of unmyelinated fiber projection to the spinal cord. Experimental Neurology, 16(3), 316-332.
Office of Strategy and Planning, Office of the Permanent Secretary, Ministry of Public Health. (2023). Summary of sick report. Gastrointestinal Disease Statistics 2021-2023. Retrieved from https://spd.moph.go.th/illness-report/
Oumer, K. E., Ahmed, S. A., Tawuye, H. Y., & Ferede, Y. A. (2021). Outcomes and associated factors among patients undergone emergency laparotomy: A retrospective study. International Journal of Surgery Open, 36(1), 1-10.
Patil, J. D., & Sefen, J. A. N. (2022). A mini review: Exploring non-pharmacological methods for pre-operative pain management. Frontiers in Surgery, 9(1), 1-5.
Poulton, T., Murray, D., & National Emergency Laparotomy Audit (NELA) Project Team. (2019). Pre-optimisation of patients undergoing emergency laparotomy: A review of best practice. Anaesthesia, 74(1), 100-107.
Roslan, F., Kushairi, A., Cappuyns, L., Daliya, P., & Adiamah, A. (2020). The impact of sham feeding with chewing gum on postoperative ileus following colorectal surgery: A meta-analysis of randomised controlled trials. Journal of Gastrointestinal Surgery, 24(11), 2643-2653.
Rosowicz, A., Brody, J. S., Lazar, D. J., Bangla, V. G., Panahi, A., Nobel, T. B., & Divino, C. M. (2022). Early ambulation is associated with improved outcomes following colorectal surgery. The American Surgeon™, 89(12), 5225-5233.
Ruttanapun, T., Chinnawong, T., & Naka, K. (2021). Development and evaluation of clinical nursing practice guideline for promoting recovery in elderly patients after abdominal surgery. Journal of Research in Nursing-Midwifery and Health Sciences, 41(4), 60-73.
Sauro, K. M., Smith, C., Ibadin, S., Thomas, A., Ganshorn, H., Bakunda, L., & Nelson, G. (2024). Enhanced recovery after surgery guidelines and hospital length of stay, readmission, complications, and mortality: A meta-analysis of randomized clinical trials. JAMA Network Open,7(6), 1-16.
Shapter, S. L., Paul, M. J., & White, S. M. (2012). Incidence and estimated annual cost of emergency laparotomy in England: is there a major funding shortfall? Anaesthesia, 67(5), 474-478.
Sharma, J., Kumar, N., Huda, F., & Payal, Y. S. (2021). Enhanced recovery after surgery protocol in emergency laparotomy: A randomized control study. The Surgery Journal, 7(2), 92-99.
Shida, D., Tagawa, K., Inada, K., Nasu, K., Seyama, Y., Maeshiro, T., & Umekita, N. (2017). Modified enhanced recovery after surgery (ERAS) protocols for patients with obstructive colorectal cancer. BMC Surgery, 17(1), 1-6.
Simpson, J. C., Bao, X., & Agarwala, A. (2019). Pain management in enhanced recovery after surgery (ERAS) protocols. Clinics in Colon and Rectal Surgery, 32(2), 121-128.
Stethen, T. W., Ghazi, Y. A., Heidel, R. E., Daley, B. J., Barnes, L., Patterson, D., & McLoughlin, J. M. (2018). Walking to recovery: The effects of missed ambulation events on postsurgical recovery after bowel resection. Journal of Gastrointestinal Oncology, 9(5), 953-961.
Syed, W. H., Ahmed, R., Qureshi, U., Khan, J. S., Shafique, S., Azhar, F., & Farooqi, S. A. (2020). Exploratory laparotomies in the emergency room: Increasing burden and implications in Pakistan. Rawal Medical Journal, 45(4), 798-801.
The Joanna Briggs Institute. (2019). Joanna Briggs Institute reviewer manual 2019. Retrieved from https://wiki.joannabriggs.org/display/MANUAL/JBI+Reviewer%27s+Manual
The Royal College of Anesthesiologists of Thailand and Thai Association for the Study of Pain. (2019). Clinical guidance for acute postoperative pain management. Bangkok: The Royal College of Anesthesiologists of Thailand.
Tra, A., Tintin, S., & Ilya, K. (2020). A review on reducing the incidence of postoperative ileus by chewing gum, consuming coffee or warm water post abdominal surgery. Jurnal Medisains/Jurnal Ilmiah Kesehatan, 18(1), 24-34.
Weindelmayer, J., Mengardo, V., & Carlini, M. (2021). ERAS protocols for gastrectomy. Gastric Cancer: the 25-year R-Evolution, 245-251.
Whittemore, R., & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546-553.
Wongruang, W., Vuttanon, N., & Udomkhamsuk, W. (2020). Effect of gum chewing on bowel function recovery in post abdominal surgery patients. Nursing Journal, 47(3), 157-167.
Yang, P., Long, W. J., & Li, W. (2018). Chewing xylitol gum could accelerate bowel motility recovery after elective open proctectomy for rectal cancer. Revista de Investigacion Clinica, 70(1), 53-58.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2025 วารสารพยาบาลตำรวจและวิทยาศาสตร์สุขภาพ

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ