Development of Clinical Nursing Practice Guidelines for Preventing Complications in Patients with Pulmonary Alveolar Proteinosis Undergoing General Anesthesia for Whole Lung Lavage
Abstract
This research and development project aimed to develop and study the feasibility of clinical nursing practice guidelines (CNPG) for preventing complications in patients with pulmonary alveolar proteinosis (PAP) undergoing general anesthesia for whole lung lavage (WLL) at Sunpasitthiprasong Hospital, Ubon Ratchathani, Thailand. The CNPGs were developed using the evidence-based practice model of Soukup, which has the following four steps: 1) Evidence-triggered phase, 2) Evidence-supported phase., 3) Evidence-observed phase, and 4) Evidence-based phase. The Phases 1 through 3 of the study were conducted from. There were 11 papers containing evidence best practices that were evaluated for reliability, and which were divided into eight level 4a papers, two level 4b papers, and one 4d paper. The participants for the pilot study were selected by purposive sampling according to specified qualifications and consisted of 45 nurse anesthetists to assess the feasibility of using the nursing practice guidelines, and two patients with PAP who underwent anesthesia for WLL. The research instruments consisted of 1) the CNPG and 2) a questionnaire on opinions toward the CNPG. The CNPGs were validated by three experts using the AGREE II (Appraisal of Guidelines for Research & Evaluation II) approach. Data were analyzed using descriptive statistics.
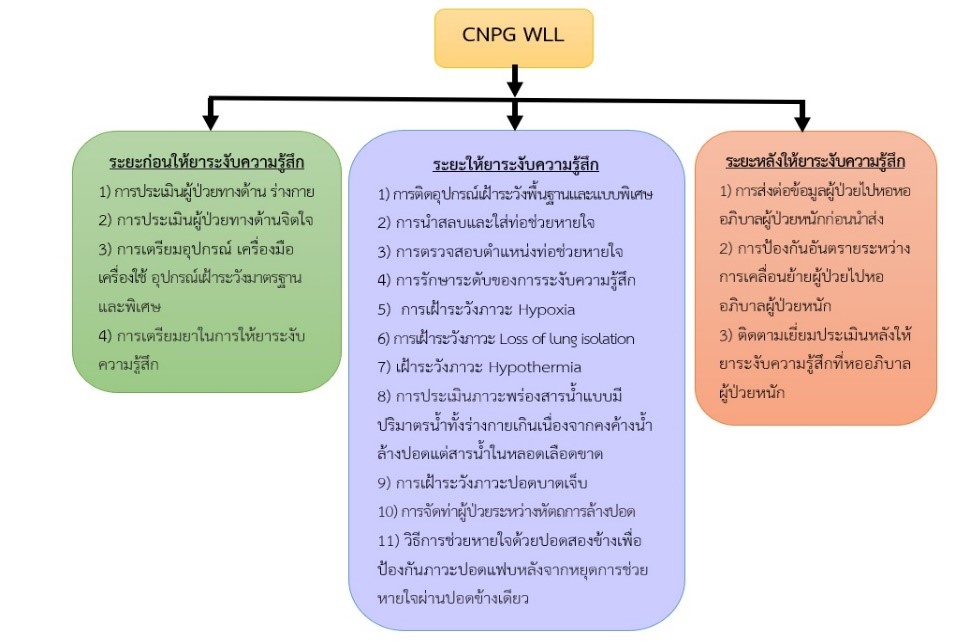
The results: revealed that 1) the CNPG consisted of 3 phases of nursing activities, including pre-anesthesia nursing, peri-anesthesia nursing, and post-anesthetic nursing; 2) the results of the expert's appraisal were 87.62% favorable; and 3) the feasibility study indicated that the CNPG had a good level of feasibility for being integrated into practice. Implementing nursing practice guidelines in a pilot study with patients found that nurse anesthetists could follow all the guidelines. A comparative study of the effectiveness of the CNPGs in relation to standard practices is recommended for the next research.
References
Abdelmalak BB, Khanna AK, Culver DA, Popovich MJ. Therapeutic whole-lung lavage for pulmonary alveolar proteinosis a procedural update. J Bronchol Intervent Pulmonol 2015;22:251-8. doi: 10.1097/LBR.0000000000000180.
Kumar A, Abdelmalak B, Inoue Y, Culver DA. Pulmonary alveolar proteinosis in adults: pathophysiology and clinical approach. Lancet Respir Med 2018;6:554–65. doi: 10.1016/S2213-2600(18)30043-2.
Awab A, Khan MS, Youness HA. Whole lung lavage-technical details, challenges and management of complication. J Thorac Dis 2017;9:1697-706. https://doi.org/10.21037/jtd.2017.04.10.
Shrestha D, Dhooria S, Munirathinam GK, Sehgal IS, Prasad KT, Ram B, et al. How we do it: whole lung lavage. Sarcoidosis Vasc Diffuse Lung Dis 2022;39:1-9. doi: 10.36141/svdld.v39i2.12884.
Kaenmuang P, Navasakulpong A. Efficacy of whole lung lavage in pulmonary alveolar proteinosis: a 20-year experience at a reference center in Thailand. J Thorac Dis 2021; 13:3539-48. doi: http://dx.doi.org/10.21037/jtd-20-3308.
Moreira JP, Ferraz S, Freitas C, Morais A, Albuquerque RR, Fiuza C. Whole-lung lavage for severe pulmonary alveolar proteinosis assisted by veno-venous extracorporeal membrane oxygenation: a case report. Can J Respir Ther 2019;55:9-12. doi:10.29390/cjrt-2018-019.
Soukup SM. The center for advanced nursing practice evidence-based practice model: Promoting the scholarship of practice. Nursing Clinics of North America 2000;35:301-9.
Thongpramoon W, Muntraporn N. One lung ventilation (OLV) anesthesia in patient who undergone thoracotomy: Role of nurse anesthetist. Thai Journal of Nursing and Midwifery Practice 2015;2:25-40.
Phiphanmekhaphon T. Intraoperative management for thoracic surgery. In: Phiphanmekhaphon T, Editor. Anesthesia for Thoracic Surgery. Chiangmai: Sangslip Printing Chiangmai; 2022. P.215-87.
Jensen KA. 7 STEPS TO THE PERFECT PICO SEARCH Evidence-Based Nursing Practice[Internet]. 2021 [cited 2021 Oct 26]. Available from: https://tinyurl.com/z9m5ecbf.
The Joanna Briggs Institute. New JBI Levels of Evidence. Level of Evidence and Grades of Recommendation Working Party October 2013 [Internet]. 2013 [cited 2020 Aug 1]. Available from: www.Joannabriggs.edu.au pubs/approach.php.
Ministry of Public Health Department of Medical Services. Appraisal of Guideline for Research & Evaluation II; AGREE II[Internet]. 2013 [cited 2023 Jan 9]. Available from: https://tinyurl.com/z9m5ecbf.
Vymazal T, Krecmerova M. Respiratory Strategies and Airway Management in Patients with Pulmonary Alveolar Proteinosis: A Review. BioMed Research International [internet]. 2015 [cited 2023 May 15]. Available from: http://dx.doi.org/10.1155/2015/639543
Mata-Suarez SM, Castro-Lalin A, Loughlin SM, Domini JD, Bianco JC. Whole lung lavage- a narrative review of anesthetic management. J Cardiothorac Vasc Anesth 2020;36:587-93. doi: https://doi.org/10.1053/j.jvca.2020.12.002
Pasitchakrit P, Sriramatr D, Limim J, Buppha P. Volatile anesthetic consumption by bispectral index monitoring compared to hemodynamic monitoring. J Med Health Sci 2017; 24:37-44.
Smith BB. Torres NE, Hyde JA, Barbara DW, Gillespie SM, Wylam ME, Smith MM. Whole-lung lavage and pulmonary alveolar proteinosis: review of clinical and patient-centered outcomes. J Cardiothorac Vasc Anesth 2019;33:2453-61. doi: 10.1053/j.jvca.2019.03.047.
Kiani A, Parsa T, Naghan PA, Dutau H, Razavi F, Farzanegan B, et al. An eleven-year retrospective cross-sectional study on pulmonary alveolar proteinosis. Adv Respir Med 2018;86:7–12. doi: 10.5603/ARM.2018.0003.
Jung JW, Lee H, Oh J. Anesthetic management during whole-lung lavage using lung ultrasound in a patient with pulmonary alveolar proteinosis: a case report. Yeungnam Univ J Med 2021;38:374-80. doi: https://doi.org/10.12701/yujm.2021.01284.
Raksakiattisak M. Anesthesia for thoracic spine surgery. In: Raksakiattisak M, Iamarun A, Editor. Anesthesia for spine surgery. Bangkok: Siriraj Publishing House; 2017. P. 159-70.
Bourn S, Wijesingha S, Nordmann G. Transfer of the critically ill adult patient. BJA Educ 2018;18:63–8. doi: 10.1016/j.bjae.2017.11.008.
Hanucharurnkul S. Improvement Science. Thai Journal of Nursing and Midwifery Practice 2016;3:5-14.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Boromarajonani College of Nursing Sunpasitthiprasong

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของวารสารวิทยาศาสตร์สุขภาพ วิทยาลัยพยาบาลบรมราชชนนี สรรพสิทธิประสงค์ ข้อความที่ปรากฏในบทความแต่ละเรื่องเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี สรรพสิทธิประสงค์ และคณาจารย์ท่านอื่นๆ ในวิทยาลัยพยาบาลฯ ความรับผิดชอบเกี่ยวกับบทความแต่ละเรื่องผู้เขียนจะรับผิดชอบของตนเอง


