Multiple genotype infection of human papilloma virus is associated with cervical cytological abnormalities
Main Article Content
Abstract
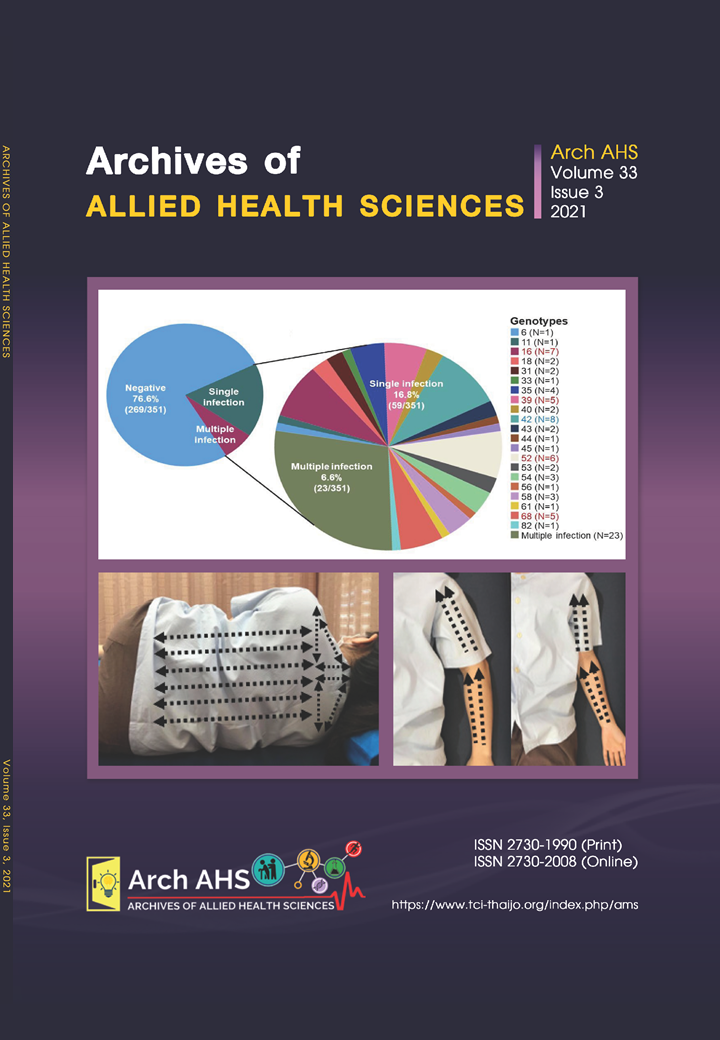
Development of cervical cancer is associated with persistent infection of human papillomavirus (HPV). The present study is aimed to determine the association of HPV infection and cervical cytological abnormalities. HPV genotypes and liquid-based cytological analyses were performed 351 cervical brush samples obtained from women visited Gynecology Clinic, Khon Kaen Hospital, Khon Kaen, Thailand. HPV was detected in 23.36% (82/351) of the cases. Among the HPV positive case, 71.95% (59/82) was found with single infection and 28.05% (23/82) were with multiple infections. Of 351 tested specimens, 7.6% (27/351) were presented with abnormal cytology, and 62% (17/27) of these 27 cases were found to positive for HPV. The cytological anomalies presented in HPV positive cases were 52.94% (9/17) of ASCUS, 28.41% (5/17) of LSIL and 17.64% (3/17) of HSIL. Our data showed that cytological abnormalities were more frequently observed in patients with multiple HPV infection, comparing to those with single infection (P < 0.001). However, among the patients with single HPV infection, cytological data were not different between patients with high-risk HPV (HR-HPV) and low-risk HPV(LR-HPV). In conclusion, our present study revealed the association between multiple HPV infection and cervical cytological abnormalities. This information emphasizes the important of HPV genotype analysis for cervical cancer screening and surveillance, those women with multiple HPV infection are strongly suggested to be treated and frequently followed up.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Priebe AM. 2012 cervical cancer screening guidelines and the future role of HPV testing. Clin Obstet Gynecol 2013; 56(1): 44-50.
Dong B, Sun P, Ruan G, Huang W, Mao X, Kang Y, et al. Type-specific high risk human papillomavirus viral load as a viable triage indicator for high grade squamous intraepithelial lesion: A nested case control study. Cancer Manage Res 2018; 10: 4839-51.
Munagala R, Kausar H, Munjal C, Gupta RC. Withaferin A Induces p53-dependent apoptosis by repression of HPV oncogenes and upregulation of tumor suppressor proteins in human cervical cancer cells. Carcinogenesis 2011; 32(11): 1697-705.
Wright T, Ronnett B, Kurman R, Ferenczy A. Precancerous lesions of the cervix. In: Kurman R, EllensonL, Ronnett B. Blaustein’s pathology of the female genital tract. 6th ed. New York: Springer Publisher;2011. p. 193-252.
Chan PK. Human papillomavirus type 58: the unique role in cervical cancers in East Asia. Cell Biosci 2012; 2(1): 17.
Kietpeerakool C, Kleebkaow P, Srisomboon J. Human Papillomavirus genotype distribution among Thai women with hogh-grade cervical intraepithelial lesions and invasive cervical cancer: a literature review. Asian Pac J Cancer Prev 2015; 16(13): 5153-8.
Song JS, Kim EJ, Choi J, Gong G, Sung CO. Significance of HPV-58 infection in women who are HPV-positive, cytology-negative and living in a country with a high prevalence of HPV-58 infection. PLoS One 2013; 8(3): e58678.
Assoumou SZ, Mbiguino AN, Mabika BM, Ogoula SN, Mzibri ME, Khattabi A, et al. Human papillomavirus genotypes distribution among Gabonese women with normal cytology and cervical abnormalities. Infect Agent Cancer 2016; 11: 2.
Krashias G, Koptides D, Christodoulou C. HPV prevalence and type distribution in Cypriot women with cervical cytological abnormalities. BMC Infect Dis. 2017; 17(1): 346.
Chaturvedi AK, Katki HA, Hildesheim A, Rodriguez AC, Quint W, Schiffman QM, et al. Human papillomavirus infection with multiple types: Pattern of coinfection and risk of cervical disease. J Infect Dis 2011; 203(7): 910-20.
Salazar KL, Zhou HS, Xu J, Peterson LE, Schwartz MR, Mody DR, et al. Multiple human papilloma virus infections and their impact on the development of high risk cervical lesions. Acta Cytol 2015; 59(5): 391-8.
Li M, Du X, Lu M, Zhang W, Sun Z, Li L, et al. Prevalence characteristics of single and multiple HPV infections in women with cervical cancer and precancerous lesions in Beijing, China. J Med Virol 2019;91(3): 473-81.
Anttila A, Kotaniemi-Talonen L, Leinomen M, Hakama M, Laurila P, Tarkkanen J, et al. Rate of cervical cancer, severe intraepithelial neoplasia, and adenocarcinoma in situ in primary HPV DNA screening with cytology triage: randomized study within organised screening programme. BMJ 2010; 340: c1804.
Leinonen MK, Nieminen P, Lonnberg S, Malila N, Hakama M, Pokhrel A, et al. Detection rate of precancerous and cancerous cervical lesions within one screening round of primary human papillomavirus DNA testing: prospective randomized trial in Finland. BMJ 2012; 345: e7789.
Chittihaworn S, Charakorn C, Kongsawatvorakul. Cervical cancer screening guidelines: An updated review. Thai J Obstet Gynaecol 2021; 29(4): 186-90.
Hesselink AT, Sahli R, Berkhof J, Snijders PJF, SalmML, Agard A et al. Clinical validation of AnyplexTM II HPV HR Detection according to the guidelines for HPV test requirements for cervical cancer screening, J Clin Virol 2016; 76: 36-9.
Wu RF, Dai M, Qiao YL, Clifford GM, Liu ZH, Arslan A, et al. Human papillomavirus infection in women in Shenzhen City, People’s Republic of China, a population typical of recent Chinese urbanisation. Int J Cancer 2007; 121(6): 1306-11.
Chen Q, Xie LX, Qing ZR, Li LJ, Luo ZY, Lin M, et al. Epidemiologic characterization of human papillomavirus infection in rural Chaozhou, eastern Guangdong Province of China. PLoS One 2012; 7(2): e32149.
Bosch FX, Burchell AN, Schiffman M, Giuliano AR, de Sanjose S, Bruni L, et al. Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine 2008; 26(Suppl 10): K1-16.
Tangsiriwatthana T, Pholampaisathit S, Chainual A, Boonsom K, Vittayanan S, Thichak S et al. HPV infection in Thai women with normal cytology. Bull Med Sci 2019; 61(2): 73-85.
Schmitt M, Depuydt C, Benoy I, Bogers J, Antoine J, Arbyn M, et al. Multiple human papillomavirus infections with high viral loads are associated with cervical lesions but do not differentiate grades of cervical abnormalities. J Clin Microbiol 2013; 51(5): 1458-64.
Lin M, Yang LY, Li LJ, Wu JR, Peng YP, Luo ZY. Genital human papillomavirus screening by gene chip in Chinese women of Guangdong province. Aust N Z J Obstet Gynaecol 2008; 48(2): 189-94.
Ye J, Cheng X, Chen X, Ye F, Lu W, Xie X. Prevalence and risk profile of cervical Human papillomavirus infection in Zhejiang Province, southeast China: a population-based study. Virol J 2010; 7: 66.
Anttila A, Kotaniemi-Talonen L, Leinonen M, Hakama M, Laurila P, Tarkkanen J, et al. Rate of cervical cancer, severe intraepithelial neoplasia, and adenocarcinoma in situ in primary HPV DNA screening with cytology triage: randomised study within organised screening programme. BMJ 2010; 340: c1804.
Antonsson A, Cornford M, Perry S, Davis M, Dunne MP, Whiteman DC. Prevalence and risk factors oral HPV infection in young Australians. Plos One 2014; 9(3): c91761.