Factors associated with mortality rates in acute ischemic stroke patients after rt-PA administration in Saraburi hospital
Keywords:
acute stroke, stroke outcomes, mortality, risk factorAbstract
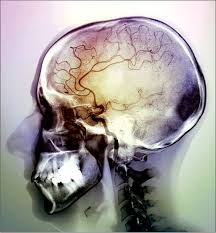
Ischemic stroke is a main Thai public health issue and leading cause of death in both men and women. The information on precise predictors of in-hospital stroke mortality is insufficient but often requested in clinical practice. Therefore, we aimed to study the significant factors that increasing mortality tPA given acute ischemic stroke patients. This was retrospective study using data from all patients that was diagnosed acute ischemic stroke and was given tPA admitted in Saraburi stroke unit between 2015 and 2021. All baseline characteristics and complications data were analyzed using univariate and multivariate binary logistic regression analysis to estimate crude and adjusted odds ratio (OR). Total 287 patients diagnosed with acute ischemic stroke were included in this analysis (52.9% older than 60 years, 55.3% men). The mortality rate at the stroke unit was 13% and median stay of deceased patients was 5 days. In non-survivor group the median NIHSS score was 17 higher than in NIHSS 10 in survivor group. Etiology of stroke by TOAST classification, 55.3% was cardio-embolic stroke followed by 34.2% large artery atherosclerosis, most common sites is MCA (81.6%). Main factors that increased risk of in-hospital death as following MCA with an OR of 6.10 (95%CI 6.10 –17.16), AOC with an ORs 4.89(95% CI 1.60-14.93), given IV antihypertensive before tPA with OR 3.89 (95%CI 1.50-10.11), also swollen dysfunction and gaze disturbance. Complications increased mortality as following pneumonia with OR 9.77 (95%CI4.49-21.27), intracranial hemorrhage with ORs 3.41 (95% CI 1.64-7.09), progressive stroke with an OR 7.75 (95%CI 3.24-18.51) brain herniation with ORs 16.33(95%CI 4.64-57.51), and arrythmia with an OR 4.34 (95%CI 2.14-8.82). These results might help physicians planning the care team management, recognizing the need for intensified monitoring and providing the information to help in the communication with family members or care-giver.
References
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al.; Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010.Lancet. 2014; 383:245–254.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review.Lancet Neurol. 2009; 8:355–369.
Saposnik G, Kapral MK, Liu Y, Hall R, O’Donnell M, Raptis S, et al.; Investigators of the Registry of the Canadian Stroke Network; Stroke Outcomes Research Canada (SORCan) Working Group. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke.Circulation. 2011; 123:739–749
Ganesh A, Lindsay P, Fang J, Kapral MK, Côté R, Joiner I, et al.. Integrated systems of stroke care and reduction in 30-day mortality: a retrospective analysis.Neurology. 2016; 86:898–904.
Gattringer T, Posekany A, Niederkorn K, Knoflach M, Poltrum B, Mutzenbach S, Haring HP, Ferrari J, Lang W, Willeit J, Kiechl S, Enzinger C, Fazekas F; Austrian Stroke Unit Registry Collaborators. Predicting Early Mortality of Acute Ischemic Stroke. Stroke. 2019 Feb;50(2):349-356.
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581–7
Bateman BT, Schumacher HC, Boden-Albala B, Berman MF, Mohr JP, Sacco RL, Pile-Spellman J. Factors associated with in-hospital mortality after administration of thrombolysis in acute ischemic stroke patients: an analysis of the nationwide inpatient sample 1999 to 2002. Stroke. 2006 Feb;37(2):440-6.
Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, Kissela BM, Kittner SJ, Lichtman JH, Lisabeth LD, Schwamm LH, Smith EE, Towfighi A; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014 Jan;45(1):315-53.
Kaduka L, Muniu E, Oduor C, Mbui J, Gakunga R, Kwasa J, Wabwire S, Okerosi N, Korir A, Remick S: Stroke Mortality in Kenya’s Public Tertiary Hospitals: A Prospective Facility-Based Study. Cerebrovasc Dis Extra 2018;8:70-79.
Viderman, Dmitriy & Issanov, Alpamys & Temirov, Talgat & Goligher, Ewan & Fleur, Philip. (2020). Outcome Predictors of Stroke Mortality in the Neurocritical Care Unit. Frontiers in Neurology. 11. 10.3389/fneur.2020.579733.
Kortazar-Zubizarreta I, Pinedo-Brochado A, Azkune-Calle I, Aguirre-Larracoechea U, Gomez-Beldarrain M, Garcia-Monco JC. Predictors of in-hospital mortality after ischemic stroke: A prospective, single-center study. Health Sci Rep. 2019 Feb 17
Alene, M., Assemie, M.A., Yismaw, L. et al. Magnitude of risk factors and in-hospital mortality of stroke in Ethiopia: a systematic review and meta-analysis. BMC Neurol 20, 309 (2020).
Koton S, Schneider AL, Rosamond WD, Shahar E, Sang Y, Gottesman RF, Coresh J. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014 Jul 16;312(3):259-68.
Wirat Onsee, M.D., Mortality Rate of Ischemic Stroke Patients after Establish Stroke Fast Tract in Phetchabun Hospital, Department of Internal Medicine, Phetchabun Hospital, Phetchabun Province, Thailand, Journal of Health Science 2015;24:876-84.
Kaarisalo MM, Immonen-Räihä P, Marttila RJ, Salomaa V, Kaarsalo E, Salmi K, Sarti C, Sivenius J, Torppa J, Tuomilehto J. Atrial fibrillation and stroke. Mortality and causes of death after the first acute ischemic stroke. Stroke. 1997 Feb;28(2):311-5.
De la Fuente-Martínez J, Infante-Valenzuela A, Martínez-Roque D, Cruz-Moreno M, Góngora-Rivera F. Impact of Arrhythmia in Hospital Mortality in Acute Ischemic Stroke Patients: A Retrospective Cohort Study in Northern Mexico. J Stroke Cerebrovasc Dis. 2022 Feb;31(2):106259.
Tu HTH, Campbell BCV, Christensen S, Collins M, De Silva DA, Butcher KS, Parsons MW, Desmond PM, Barber PA, Levi CR, et al. Pathophysiological determinants of worse stroke outcome in atrial fibrillation. Cerebrovasc Dis. 2010; 30:389–395.
Kaarisalo MM, Immonen-Räihä P, Marttila RJ, Salomaa V, Kaarsalo E, Salmi K, Sarti C, Sivenius J, Torppa J, Tuomilehto J. Atrial fibrillation and stroke. Mortality and causes of death after the first acute ischemic stroke. Stroke. 1997 Feb;28(2):311-5.
Beume L‐A, Hieber M, Kaller CP, Nitschke K, Bardutzky J, Urbach H, Weiller C, Rijntjes M. Large vessel occlusion in acute stroke. Stroke. 2018; 49:2323–2329.
Rao NM, Levine SR, Gornbein JA, Saver JL. Defining clinically relevant cerebral hemorrhage after thrombolytic therapy for stroke: analysis of the National Institute of Neurological Disorders and Stroke tissue-type plasminogen activator trials. Stroke. 2014 Sep;45(9):2728-33.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Thai Journal Citation Index Centre

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Journal of TCI is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) licence, unless otherwise stated. Please read our Policies page for more information.





