Soluble Vascular Cell Adhesion Molecule as a Predictor of Arteriovenous Fistula Maturation: A Pilot Study
Main Article Content
Abstract
Background: Predicting arteriovenous fistula (AVF) maturation in patients with end-stage kidney disease remains challenging. Soluble vascular cell adhesion molecule (sVCAM) is involved in vascular remodeling, but its predictive value is not well established. This study evaluated whether sVCAM levels can predict AVF maturation 8 weeks after creation.
Methods: In this prospective pilot diagnostic study, 19 patients undergoing AVF creation were enrolled. sVCAM levels were measured preoperatively and 4 weeks postoperatively. AVF maturation was assessed at 8 weeks using ultrasonographic criteria.
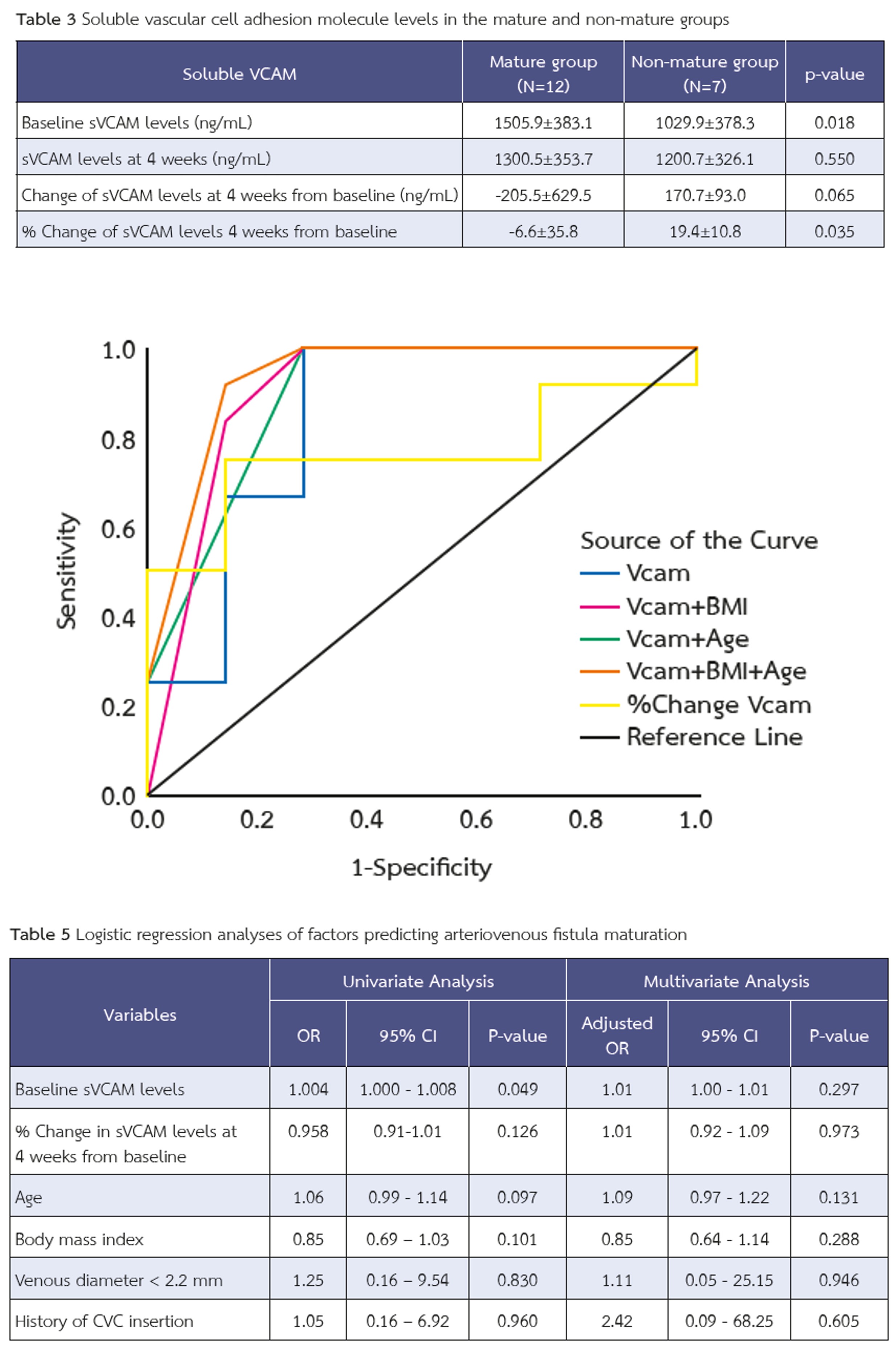
Results: Twelve patients (63%) achieved AVF maturation. Those with mature AVFs had significantly higher baseline sVCAM levels than those without maturation (1505.9±383.1 vs. 1029.9±378.3 ng/mL, p = 0.018). The percentage change in sVCAM levels also differed significantly between groups (mature: –6.6±35.8% vs. non-mature: +19.4±10.8%, p = 0.035). A baseline sVCAM threshold of ≥985.9 ng/mL yielded 100% sensitivity and 71.4% specificity for predicting AVF maturation (AUC = 0.845, 95% CI: 0.632–1.000). Combining sVCAM levels with clinical parameters, including age <73 years and BMI <30 kg/m², further improved predictive accuracy, achieving the highest AUC of 0.935 (95% CI: 0.804–1.000).
Conclusions: Preoperative sVCAM level is a promising biomarker for predicting successful AVF maturation. Incorporating clinical parameters alongside sVCAM further enhances predictive performance.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020;75(4 Suppl 2):S1-S164. doi: 10.1053/j.ajkd.2019.12.001
González I, Maldonado-Agurto R. The role of cellular senescence in endothelial dysfunction and vascular remodelling in arteriovenous fistula maturation. J Physiol. 2025; 20. doi: 10.1113/jp287387
Garmy-Susini B, Jin H, Zhu Y, Sung R-J, Hwang R, Varner J. Integrin alpha4beta1-VCAM-1-mediated adhesion between endothelial and mural cells is required for blood vessel maturation. J Clin Invest. 2005;115(6):1542-51. doi: 10.1172/jci23445
Kanwar YS. Functional duality of progenitor cells influxing into arterio-venous fistula during its neoangiogenesis. Am J Physiol Renal Physiol. 2007;293(2):F468-9. doi: 10.1152/ajprenal.00237.2007
Saito O, Usui M, Abe M, Okada K, Takei T, Ito Y, Nagata M. Serum endothelial injury markers in hemodialysis patients with arteriovenous fistula stenosis. Jichi Medical University Journal. 2012;35:1-6.
Cai W, Zhu L, Chen X, Chen J, Su S, Li J, et al. Association of advanced glycoxidation end products and inflammation markers with thrombosis of arteriovenous grafts in hemodialysis patients. Am J Nephrol. 2006;26(2):181-5. doi: 10.1159/000093122
Beathard GA, Lok CE, Glickman MH, Al-Jaishi AA, Bednarski D, Cull DL, Lawson JH, Lee TC, Niyyar VD, Syracuse D, Trerotola SO, Roy-Chaudhury P, Shenoy S, Underwood M, Wasse H, Woo K, Yuo TH, Huber TS. Definitions and End Points for Interventional Studies for Arteriovenous Dialysis Access. Clin J Am Soc Nephrol. 2018;13(3):501-12. doi: 10.2215/cjn.11531116
Kitpanit, N. and Makprasert, P. 2021. Maturation Rate of Brachiocephalic VS Brachioantecubital Arteriovenous Fistula; A Prospective Cohort Study. Journal of the Association of General Surgeons of Thailand under the Royal of Patronage of HM the King. 2021; 6 (1):16–23
Martinez LI, Esteve V, Yeste M, Artigas V, Llagostera S. Clinical Utility of a New Predicting Score for Radiocephalic Arteriovenous Fistula Survival. Ann Vasc Surg. 2017;41:56-61. doi: 10.1016/j.avsg.2016.09.022
Siddiqui MA, Ashraff S, Santos D, Rush R, Carline T, Raza Z. Predictive parameters of arteriovenous fistula maturation in patients with end-stage renal disease. Kidney Res Clin Pract. 2018;37(3):277-86. doi: 10.23876/j.krcp.2018.37.3.277
Robbin ML, Chamberlain NE, Lockhart ME, et al. Hemodialysis arteriovenous fistula maturity: US evaluation. Radiology. 2002;225:59–64. doi: 10.1148/radiol.2251011367
Akoglu H. User’s guide to sample size estimation in diagnostic accuracy studies. Turk J Emerg Med. 2022;22(4):177-85. doi: 10.4103/2452-2473.357348
Wongmahisorn Y. Development and validation of a clinical score to predict 1-year survival of arteriovenous fistula access: a diagnostic study. Ann Surg Treat Res. 2020;98(1):44-50. doi: 10.4174/astr.2020.98.1.44
Yan R, Song A, Zhang C. The Pathological Mechanisms and Therapeutic Molecular Targets in Arteriovenous Fistula Dysfunction. Int J Mol Sci. 2024; 25:9519. doi: 10.3390/ijms25179519
Kaur G, Sharma D, Bisen S, et al. Vascular cell-adhesion molecule 1 (VCAM-1) regulates JunB-mediated IL-8/CXCL1 expression and pathological neovascularization. Commun Biol. 2023; 6:516. doi: 10.1038/s42003-023-04905-z
Giannikouris IE, Spiliopoulos S, Giannakopoulos T, Katsanos K, Passadakis P, Georgiadis G. Evaluation of arteriovenous fistula maturation and early prediction of clinical eligibility, using ultrasound: The Fistula Maturation Evaluation (FAME) Study. J Vasc Access. 2024;26(3):926-36. doi: 10.1177/11297298241255519