ประสิทธิผลการใช้แนวปฏิบัติทางการพยาบาลเพื่อป้องกันภาวะตกเลือด 2 ชั่วโมงหลังคลอด แผนกห้องคลอด โรงพยาบาลอมก๋อย จังหวัดเชียงใหม่
คำสำคัญ:
แนวปฏิบัติทางการพยาบาล, ตกเลือดหลังคลอด, ความพึงพอใจของพยาบาล, ทักษะปฏิบัติทางการพยาบาลบทคัดย่อ
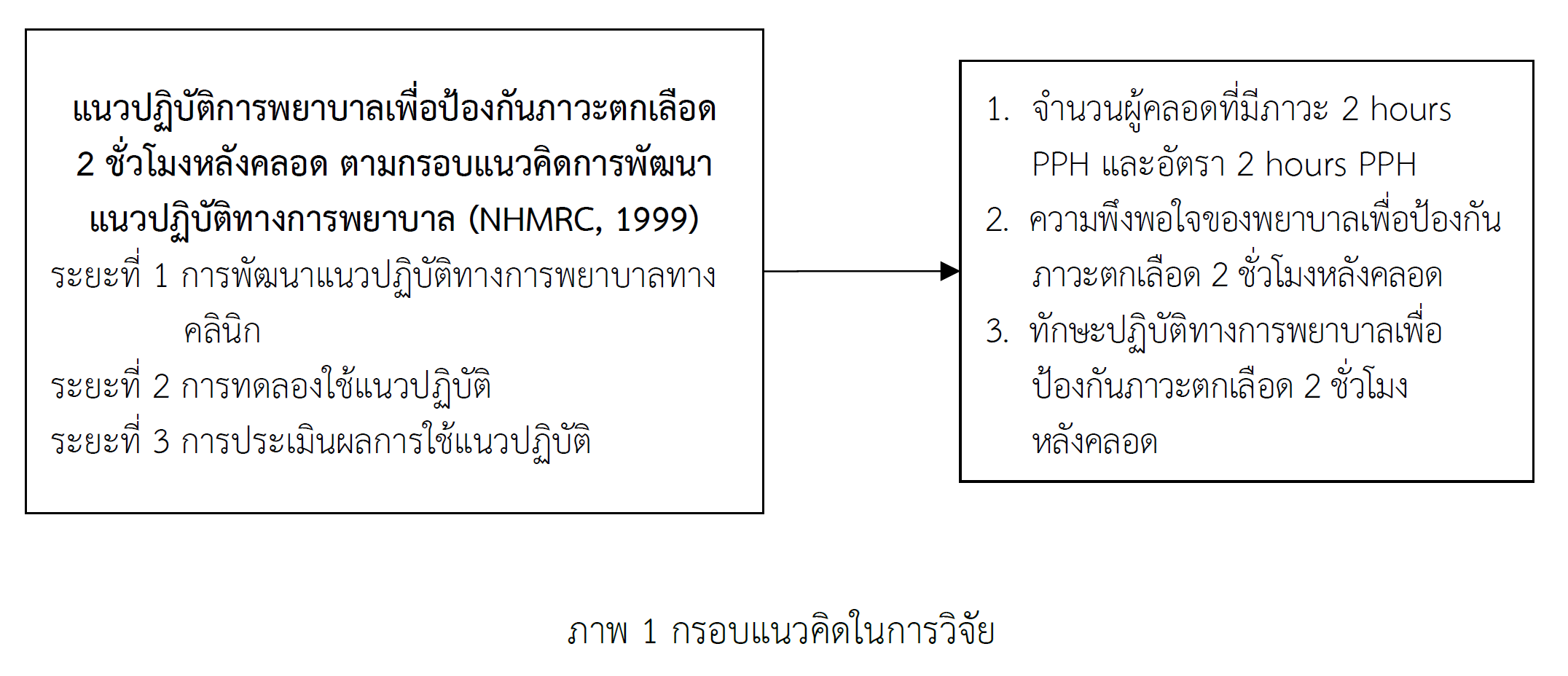
การศึกษาครั้งนี้เป็นการวิจัยกึ่งทดลอง มีวัตถุประสงค์เพื่อศึกษาอุบัติการณ์การตกเลือด 2 ชั่วโมงหลังคลอด ความพึงพอใจ และเปรียบเทียบทักษะปฏิบัติทางการพยาบาลก่อนและหลังการใช้แนวปฏิบัติทางการพยาบาลเพื่อป้องกันภาวะตกเลือด 2 ชั่วโมงหลังคลอด ตัวอย่าง คือ พยาบาลวิชาชีพที่ปฏิบัติงานหมุนเวียนในห้องคลอด จำนวน 14 คน และผู้คลอดอายุครรภ์ครบกำหนด จำนวน 57 คน ที่เข้ารับบริการระหว่างเดือน มีนาคม - เมษายน พ.ศ. 2567 เครื่องมือที่ใช้ในการดำเนินการวิจัย คือ แนวปฏิบัติทางการพยาบาลเพื่อป้องกันภาวะตกเลือด 2 ชั่วโมงหลังคลอด เครื่องมือที่ใช้ในการรวบรวมข้อมูล คือ แบบประเมินความพึงพอใจของพยาบาล และแบบประเมินทักษะในปฏิบัติทางการพยาบาลเพื่อป้องกันภาวะตกเลือด 2 ชั่วโมงหลังคลอด วิเคราะห์ข้อมูลด้วยสถิติพรรณนา ได้แก่ ความถี่ ร้อยละ ค่าเฉลี่ย ส่วนเบี่ยงเบนมาตรฐาน ความแปรปรวน และสถิติ Repeated Measurement ANOVA
ผลการศึกษา พบว่า 1) อุบัติการณ์ตกเลือด 2 ชั่วโมงหลังคลอด ภายหลังการทดลองลดลงจากก่อนการทดลอง 2) ตัวอย่างมีคะแนนเฉลี่ยความพึงพอใจของพยาบาลภายหลังการทดลองอยู่ในระดับปานกลาง (M = 18.00) 3) ตัวอย่างมีคะแนนเฉลี่ยทักษะปฏิบัติการพยาบาลหลังการทดลองทั้งเดือนที่ 1 และ 2 สูงกว่าก่อนการทดลองอย่างมีนัยสำคัญสถิติ และ 4) ตัวอย่างมีคะแนนเฉลี่ยทักษะปฏิบัติหลังการทดลองเดือนที่ 2 สูงกว่าทั้งก่อนการทดลอง และหลังการทดลองเดือนที่ 1 อย่างมีนัยสำคัญทางสถิติ
ดังนั้น แนวปฏิบัติทางการพยาบาลเพื่อป้องกันภาวะตกเลือด 2 ชั่วโมงหลังคลอดนี้จะช่วยให้พยาบาลผดุงครรภ์ผู้ปฏิบัติงานห้องคลอด โรงพยาบาลอมก๋อยดูแลผู้คลอดได้อย่างที่มีประสิทธิภาพและลดอัตราการตายของมารดาได้ ทั้งนี้ ควรทำการศึกษาความยั่งยืนของทักษะและผลลัพธ์ของแนวปฏิบัตินี้ในระยะยาว และควรสนับสนุนการใช้แนวปฏิบัติการพยาบาลนี้ในห้องคลอดโรงพยาบาลอื่นด้วย
Downloads
เอกสารอ้างอิง
Bloom, B. S. (1971). Handbook on formative and summative evaluation of student learning. New York, NY: McGraw–Hill.
Bureau of Health Promotion. (2022). The analysis of maternal death in Thailand in the last 6 months of the fiscal year 2022 (September 2021 – March 2022), the maternal mortality surveillance system. Retrieved from https://hp.anamai.moph.go.th/
Chantaburee, N., Siriphan, S., Tohpaeroh, M., & Maeka, S. (2024). Factors predicting maternal-infant attachment following unplanned cesarean section in Thai-Muslim mothers, Narathiwat province. Journal of The Police Nurses and Health Science, 16(1), 195-206.
Charoensri, P., Sarakarn, W., & Chaiyara, B. (2017). The development of a nursing model for pregnant women to prevent early postpartum hemorrhage. Journal of Nursing and Health Care, 35(3), 48-57.
Cohen, J. (1977). Statistical power for the behavioral sciences (2nd ed.). New York, NY: Academic Press.
Delivery Room, Omkoi Hospital. (2023). Summary of birth report for fiscal year 2020 - 2023, Omkoi Hospital. Chiang Mai: Omkoi Hospital.
Escobar, M. F., Nassar, A. H., Theron, G., Barnea, E. R., Nicholson, W., Ramasauskaite, D., . . . Nasner, D. (2022d). FIGO recommendations on the management of postpartum hemorrhage 2022. International Journal of Gynecology & Obstetrics, 157(S1), 3–50. https://doi.org/10.1002/ijgo.14116
Khamkruea, S., Srisuwan, T., & Kaewboonruang, R. (2018). Development of clinical practice guideline for early postpartum hemorrhage in labor room, Lamphun hospital. Lanna Journal of Health Promotion & Environmental Health, 8(1), 46-57.
Kunsete, P. (2021). Development of a clinical nursing practice guideline to prevent early postpartum hemorrhage for vaginal delivery in a labor room, Songkhla hospital. Journal of Nursing and Public Health Research, 1(2), 83-99.
Lowdermilk, D. L., Cashion, M. C., Alden, K. R., Olshansky, E., & Perry, S. E. (2024). Maternity and women’s health care (13th ed.). St. Louis, MO: Elsevier.
Maternal and Child Health Division, Department of Health. (2024). Maternal and child health division, Department of Health (April 2024 Situation), Ministry of Public Health. Retrieved from https://hp.anamai.moph.go.th/
Maternal and Child Health Section, Chiang Mai Provincial Public Health Office. (2023). Maternal and child health situation in Chiang Mai province. Retrieved from https://www.chiangmaihealth.go.th/document/230714168930015872.pdf
National Health and Medical Research Council (NMRC). (1999). A guide to the developmental, implementation and evaluation of clinical practice guidelines. Retrieved from http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/cp30.pdf
Pairoj, P., & Sirilert, S. (2025). Update management of postpartum hemorrhage. Retrieved from https://w1.med.cmu.ac.th/obgyn/lecturestopics/54198/
Pochana, W., Chaiwongsa, W., & Somchok, P. (2021). Development of the risk factor assessment and nursing practice guideline for prevention of early postpartum hemorrhage by knowledge management, Sawang Dandin Crown Prince Hospital. Research and Development Health System Journal, 14(2), 182-194.
Sanitlou, N., Satphet, W., & Naphaarak, Y. (2019). Sample size calculation using G*Power program. Journal of Suvarnabhumi Institute of Technology (Human and Social Sciences), 5(1), 496-507.
The Joanna Briggs Institute. (2013). New JBI levels of evidence: Level of evidence and grades of recommendation working party October 2013. Retrieved from http://www.Joannabriggs.edu.aupubs/approach.php
The Royal Thai College of the Obstetricians and Gynecologists. (2020). RTCOG, Clinical practice guideline prevention and management of postpartum hemorrhage. Retrieved from https://www.rtcog.or.th/photo/cpg/OB-63-020.pdf
Thiansawat, S. (2020). Instrument development for nursing research. Chiangmai: Siam Print Nana Company.
Ueatrongchit, K., Panpakdee, O., & Siripittayakunkit, A. (2012). Factors contributing to advanced practice nurses’ professional satisfaction. Thai Journal of Nursing Council, 27(2) 5-16.
Wongpon, P., & Somwong, S. (2024). Development of nursing practice guidelines to prevent of 24 hours postpartum hemorrhage by monitoring to prevent uterine atony in Saimoon hospital, Yasothon province. Retrieved from https://yasothon.moph.go.th/ssjyasothon/FrontEnd/report_AcademicWork_Read.php?racd_id=45&racdf_id=51
World Health Organization (WHO). (2023). WHO recommendations on the assessment of postpartum blood loss and use of a treatment bundle for postpartum haemorrhage. Geneva: World Health Organization. Retrieved from https://www.who.int/publications/i/item/9789240085398
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2025 วารสารพยาบาลตำรวจและวิทยาศาสตร์สุขภาพ

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ