PREVALENCE, RISK FACTORS, AND SHORT-TERM OUTCOMES AMONG LOW-BIRTH WEIGHT NEONATES BORN AFTER THE COVID-19 PANDEMIC IN A TERTIARY HOSPITAL IN NORTHERN THAILAND
Keywords:
low birth weight, gestational hypertension, premature birth, nutrition in pregnancy, quality criteria of antenatal visitsAbstract
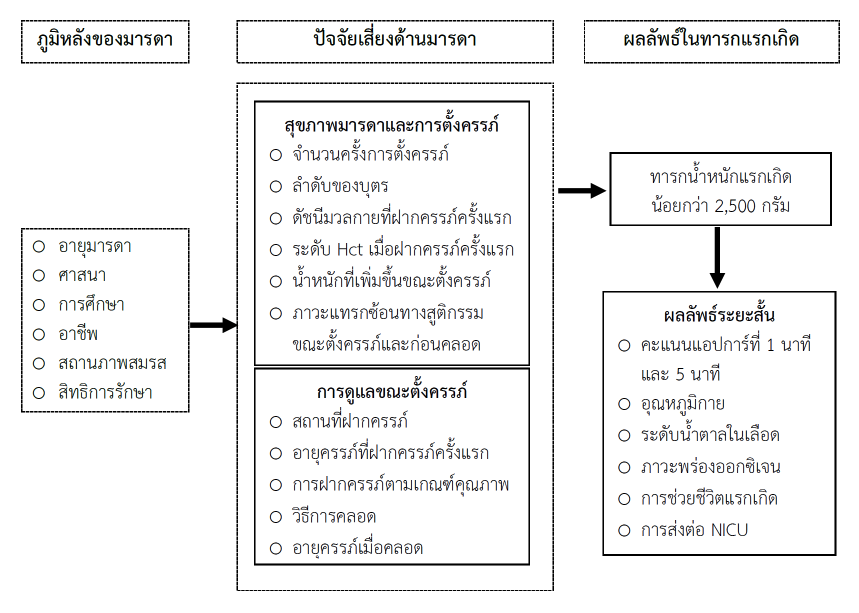
This retrospective, matched case-control study aimed to assess the prevalence and determine maternal factors and short-term outcomes associated with low birth weight in neonates born after the COVID-19 outbreak at a tertiary hospital in northern Thailand between October 1, 2022, and April 30, 2023. The sample group consisted of 183 Thai women aged 15 years and above, giving birth to singleton and alive newborns. The samples were also 61 babies with low birth weight (LBW) and 122 babies with normal birth weight. Data were collected using a data recording form created by the researcher and checked for content validity by 3 experts, with a CVI value calculated to be .87. Data were analyzed using descriptive statistics, chi-square test, and binary logistic regression.
The results showed that the prevalence of low birth weight was 9.32%. Maternal risk factors that increased the chance of low birth weight included: weight gain during pregnancy < .50 kg/week increases the chance of LBW .21 times (OR = .21; 95%CI = .09 - .61, p = .000), prenatal care according to quality criteria < 5 times increases the chance of LBW .03 times (OR = .30; 95%CI = .15 - .58,
p = .000), obstetric complications increase the chance of LBW 3.10 times (OR = 3.10; 95%CI = .25 - 79.61, p = .007), and prenatal complications increase the chance of LBW 21 times (OR = 21.00; 95%CI = 2.56 - 171.93, p = .001). Infants with low birth weight had a .10 time increased risk of having Apgar scores < 7 in the 1st and 5th minutes (OR = .10; 95%CI = .02 - .38, p = .001), risk of hypoglycemia increased 7.77 times (OR = 7.77; 95%CI = 2.00 - 29.45, p = .003), risk of severe hypoxia/ventilation with CPAP/ET tube increased 19.35 times (OR = 19.35; 95%CI = 5.46 - 68.52, p = .000), and they would be transferred to the NICU 12.35 times higher (OR = 12.35; 95%CI = 3.95 - 38.55, p = .000) when compared to newborns with normal birth weight.
Health personnel should increase efficiency in caring for pregnant women by assessing risk factors for low birth weight, promoting quality prenatal care, enhancing nutrition during pregnancy, and providing advice on self-care to reduce the chance of low birth weight. This will help reduce complications that cause illness, disability, and death among infants and young children in this region.
Downloads
References
Abubakari, A., Taabia, F. Z., & Ali, Z. (2019). Maternal determinants of low birth weight and neonatal asphyxia in the Upper West region of Ghana. Midwifery, 73, 1–7.
Adu-Bonsaffoh, K., Ntumy, M. Y., Obed, S. A., & Seffah, J. D. (2017). Perinatal outcomes of hypertensive disorders in pregnancy at a tertiary hospital in Ghana. BMC Pregnancy Childbirth, 17(1), 388–394.
Anil, K. C., Basel, P. L., & Singh, S. (2019). Low birth weight and its associated risk factors: Health facility-based case-control study. PLoS ONE, 15(6), e0234907. https://doi.org/10.1371/journal.pone.0234907
Chakreyavanich, R. (2020). Factors related to low birth weight in Health Region 5. Journal of Public Health Nursing, 34(3), 1–17.
Chmielewska, B., Barratt, I., Townsend, R., Kalafat, E., van der Meulen, J., Gurol-Urganci, I., . . . Khalil, A. (2021). Effects of the COVID-19 pandemic on maternal and perinatal outcomes: A systematic review and meta-analysis. Lancet Global Health, 9, e759–e772. https://doi.org/10.1016/S2214-109X(21)00079-6
Coutinho, P. R., Cecatti, J. G., Surita, F. G., Costa, M. L., & Morais, S. S. (2018). Perinatal outcomes associated with low birth weight in a historical cohort. Reproductive Health, 8(1), 18–22. https://doi.org/10.1186/1742-4755-8-18
de Knegt, V. E., Hedley, P. L., Hedermann, G., Wilstrup, C., Bækvad-Hansen, M, Thagaard, I. N., . . . Christiansen, M. (2023). The impact of the COVID-19 lockdown on birthweight among singleton term birth in Denmark. PLoS ONE, 18(4), e0283909. https://doi.org/10.1371/journal.pone.0283909
Department of Health, Ministry of Public Health. (2022). Service plan, mother and child branch. Public Health Administration Division.
Figueiredo, A. C. M. G., Gomes-Filho, I. S., Batista, J. E. T., Orrico, G. S., Porto, E. C. L., Cruz Pimenta, R. M., . . . Pereira, M. G. (2019). Maternal anemia and birth weight: A prospective cohort study. PLoS ONE, 14(3), e0212817. https://doi.org/10.1371/journal.pone.0212817
Fitriana, Y., Indarty, A., Mallongi, A., Mappajanci, M., Seweng, A., Hidayanty, H., Nur, R., & Syam, A. (2021). Risk factors for asphyxia neonatorum in public health centres of nosarara and pantoloan, Palu City. Gaceta Sanitaria, 35(S2), S131–S134. https://doi.org/10.1016/j.gaceta.2021.07.009
Hedley, P. L., Hedermann, G., Hagen, C. M., Bækvad-Hansen, M., Hjalgrim, H., Rostgaard, K., . . . Christiansen, M. (2022). Preterm birth, stillbirth and early neonatal mortality during the Danish COVID-19 lockdown. European Journal of Pediatrics, 181, 1175–1184. https://doi.org/10.1007/s00431-021-04297-4
Kaoian, V. (2020). A study of the maternal risk factors for low-birth-weight infants in Huaiyot hospital, Trang. Region 11 Medical Journal, 34(3), 63–72.
Kelsey, J. L., Whittemore, A. S., Evans, A. S., & Thompson, W. D. (1996). Methods in observational epidemiology. Oxford University Press, Oxford.
Khalil, A., von Dadelszen, P., Kalafat, E., Sebghati, M., Ladhani, S., Ugwumadu, A., . . . PregnaCOVID3 study group. (2021). Change in obstetric attendance and activities during the COVID-19 pandemic. Lancet Infectious Diseases, 21(5), e115. https://doi.org/10.1016/S1473-3099(20)30779-9
Khan, N., Mozumdar, A., & Kaur, S. (2020). Determinants of low birth weight in India: An investigation from the National Family Health Survey. American Journal of Human Biology, 32(3), e23355.
Lee, J. H., Youn, Y., Chang, Y. S., & The Korean Neonatal Network. (2020). Short-and long-term outcomes of very low birth weight infants in Korea: Korean Neonatal Network update in 2019. Clinical and Experimental Pediatrics, 63(8), 284-290. https://doi.org/10.3345/cep.2019.00822
Li, Z-n., Wang, S-r., & Wang, P. (2023). Associations between low birth weight and perinatal asphyxia: A hospital-based study. Medicine, 102(13), e33137.
Mathewson, K. J., Chow, C. H., Dobson, K. G., Pope, E. I., Schmidt, L. A., Van Lieshout, R. J. (2017). Mental health of extremely low birth weight survivors: A systematic review and meta-analysis. Psychological Bulletin, 143(4), 347–383. https://doi.org/10.1037/bul0000091
Muluneh, M. W., Mulugeta, S. S., Belay, A. T., & Moyehodie, Y. A. (2023). Determinants of low birth weight among newborns at Debre Tabor Referral Hospital, Northwest Ethiopia: A cross-sectional study. SAGE Open Nursing, 9, 1–8. https://doi.org/10.1177/23779608231167107
Nazira, K., Ali, S. M., & Firdaus, U. (2022). Morbidity profile and short-term outcomes of low-birth-weight neonates delivered in tertiary care center: A prospective observational study. International Journal of Contemporary Pediatrics, 9(8), 740-745. https://dx.doi.org/10.18203/2349-3291.ijcp20221857
Nur, R., Sese, R. G. C., Patui, N. S., & Fajriah, R. N. (2020). Detection mapping of women with high-risk pregnancy in antenatal care in Kamonji Public Health Center, Palu City, Indonesia. Systematic Reviews in Pharmcy, 11(2), 642–647. https://doi.org/10.5530/srp.2020.2.92
Phayuhasenarak, S. & Purinthapibal, S. (2020). Factors affecting birth of low-birth-weight babies of pregnant women attending antenatal care in Wang Wiset hospital, Trang province. Thailand Journal of Health Science, 29(3), 497–507.
Puisungnoen, N. (2023). Education in the prevalence of low-birth-weight infants after implementing of the new antenatal program for pregnant women at Debaratana Nakorn Ratchasima hospital. Medical Journal of Srisaket, Surin, Burirum Hospitals, 38(1), 143–152.
Ruiz, N. M., Íniguez, J. P. G., Gracia, S. R., & Villagrasa, M. P. S. (2022). Prospective study on influence of perinatal factors on the development of early neonatal hypoglycemia in late preterm and term infants. Anales de Pediatría, 96, 230–241.
Seema, S. (2022). Lockdown measures and COVID-19 disease control in Thailand. Library of Parliament, Office of the Secretariat of the House of Representatives.
Saini, A., Gaur, B. K., & Singh, P. (2018). Hypoglycemia in low birth weight neonates: Frequency, pattern, and likely determinants. International Journal of Contemporary Pediatrics, 5(2), 526-532. http://dx.doi.org/10.18203/2349-3291.ijcp20180548
Sertsu, A., Nigussie, K., Eyeberu, A., Tibebu, A., Negash, A., Getachew, T., . . . Dheresa, M. (2022). Determinants of neonatal hypoglycemia among neonates admitted at Hiwot Fana Comprehensive Specialized University hospital, Eastern Ethiopia: A retrospective cross-sectional study. SAGE Open Medicine, 10, 1–9. https://doi.org/10.1177/20503121221141801
Sharma, D., Shastri, S., & Sharma, P. (2016). Intrauterine growth restriction: Antenatal and postnatal aspects. Clinical Medicine Insights Pediatrics, 10, 67–83.
Shen, Z., Wang, Y., Ma, S., Zhan, Y. L., Wu, S. S., & Feng, Y. H. (2019). Risk factors for preterm birth, low birth weight and small for gestational age: A prospective cohort study. Clinical Journal of Epidemiology, 40(09), 1125-1129. https://doi.org/10.3760/cma.j
Shaohua, Y., Bin, Z., Mei, L., Jingfei, Z., Pingping, Q., Yanping, H., . . . Guoshun, M. (2022). Maternal risk factors and neonatal outcomes associated with low birth weight. Frontier in Genetics, 13, e1019321. https://doi.org/10.3389/fgene.2022.1019321
Talie, A., Taddele, M., & Alemayehu, M. (2017). Magnitude of low birth weight and associated factors among newborns delivered in Dangla Primary hospital, Amhara Regional State, Northwest Ethiopia. Journal of Pregnancy, 3587239. https://doi.org/10.1155/2019/3587239
Thapa, P., Poudyal, A., Poudel, R., Upadhyaya, D. P., Timalsina, A., Bhandari, R., . . . Adhikari, N. (2022). Prevalence of low birth weight and its associated factors: Hospital-based cross-sectional study in Nepal. PLOS Global Public Health, 2(11), e0001220. https://doi.org/10.1371/journal.pgph.0001220
UNICEF-WHO. (2019). UNICEF-WHO Low birthweight estimates: Levels and trends 2000–2015. World Health Organization, Geneva.
Zaveri, A., Paul, P., Saha, J., Barman, B., & Chouhan, P. (2020). Maternal determinants of low birth weight among Indian children: Evidence from the National Family Health Survey-4, 2015-2016. PLoS ONE, 15(12), e0244562. https://doi.org/10.1371/journal.pone.0244562
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 JOURNAL OF THE POLICE NURSES AND HEALTH SCIENCE

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ