Immediate effects of percussive massage treatment on thoracolumbar fascia thickness: a quasi-experimental design in healthy individuals
Main Article Content
Abstract
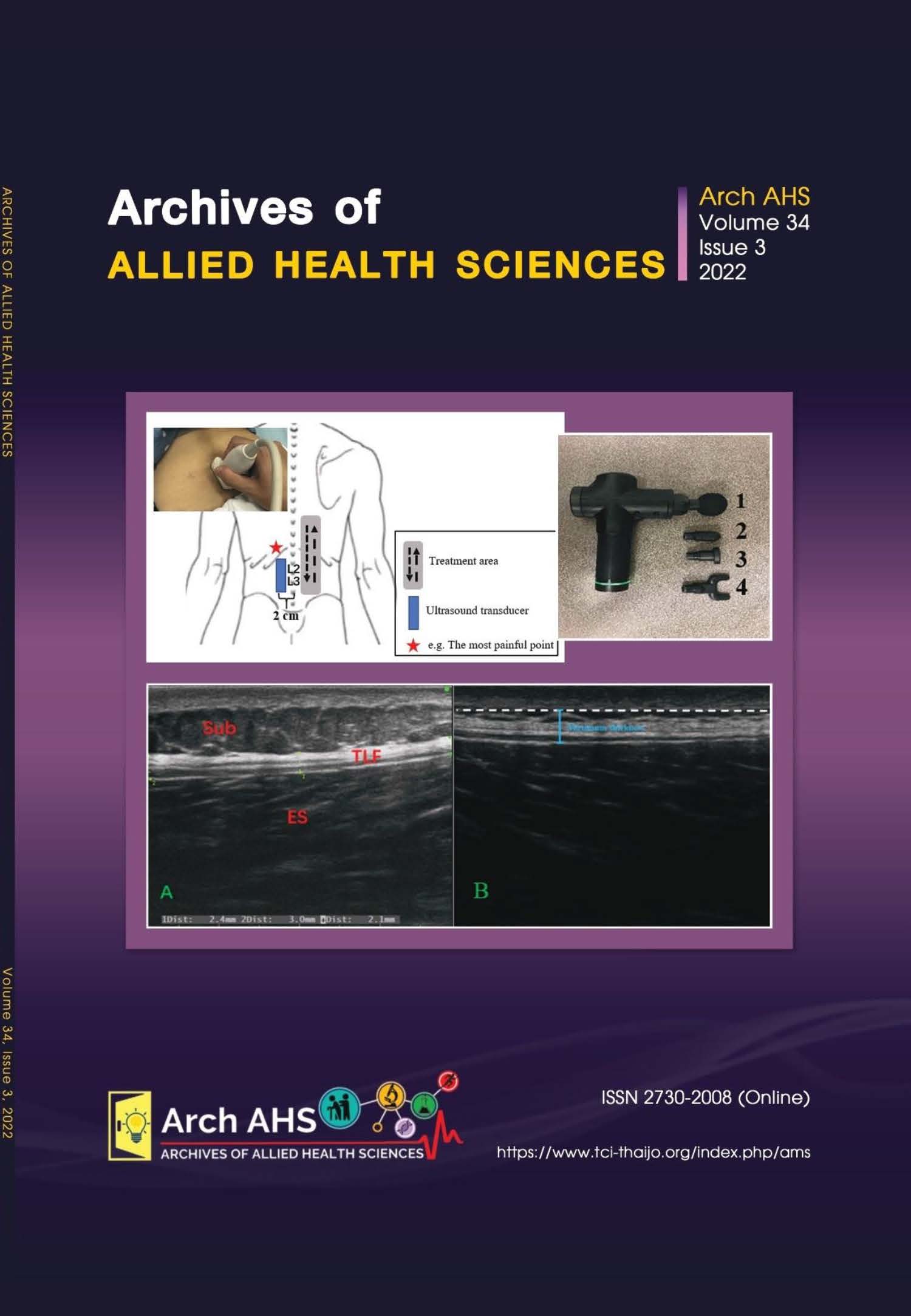
In recent years, numerous studies have pointed to the integral role of fascial tissue in developing lower back pain. Percussion massage therapy could stretch muscles and connective tissues by generating muscle waves, which may improve the fascial structures and muscle functions and provide new ideas for preventing and treating lower back pain. However, no studies have been conducted to investigate the effects of percussion massage therapy on fascial structure, skin and muscular responses, and lumbar flexibility. This pilot study aimed to preliminarily investigate the effects of percussive massage therapy on thoracolumbar fascia (TLF) thickness, skin temperature, muscle stiffness and pain, and lumbar mobility. A quasi-experimental before-and-after design was obtained in 12 healthy participants aged 20-40. A 15-minute percussion massage was performed on the participants’ TLF in the lower back region. All parameters were measured before and immediately after the intervention. The results showed that the maximum thickness value of the TLF decreased significantly after the intervention (p-value < 0.05), whereas the mean thickness value did not change. Shortly after the intervention, skin temperature increased (p-value < 0.05), perceived stiffness decreased (p-value < 0.05), visual analog scale (VAS) and press pain threshold (PPT) decreased (p-value < 0.05), and perceived stiffness decreased (p-value < 0.05). No change in lumbar flexibility was observed (p-value > 0.05). The results indicated that percussive massage therapy may reduce the maximum thickness value of TLF and improve tissue hardness, skin temperature, and pain intensity. A randomized controlled study with a large sample size is suggested to verify these effects.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001; 344(5): 363-70.
Allegri M, Montella S, Salici F, Valente A, Marchesini M, Compagnone C, et al. Mechanisms of low back pain : a guide for diagnosis and therapy. F1000Res 2016; 5: 1-11.
Wilke J, Schleip R, Klingler W, Stecco C. The lumbodorsal fascia as a potential source of low back pain: A Narrative Review. Biomed Res Int 2017; 2017: 1-6.
Pavan PG, Stecco A, Stern R, Stecco C. Painful connections: Densification versus fibrosis of fascia. Curr Pain Headache Rep 2014; 18(8): 1-8.
Langevin HM, Stevens-Tuttle D, Fox JR, Badger GJ, Bouffard NA, Krag MH, et al. Ultrasound evidence of altered lumbar connective tissue structure in human subjects with chronic low back pain. BMC Musculoskelet Disord 2009; 10(1): 1-9.
Langevin HM, Fox JR, Koptiuch C, Badger GJ, Greenan- Naumann AC, Bouffard NA, et al. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskelet Disord 2011; 12(203): 1-11.
Almaz J, Daniel L, Romero-morales C, Bravo-aguilar M, Calvo-lobo C. Quantitative ultrasound imaging differences in multifidus and thoracolumbar fasciae between athletes with and without chronic lumbopelvic pain: a case-control study. J Clin Med 2020; 9(8): 1-20.
Di Matteo A, Filippucci E, Cipolletta E, Martire V, Jesus D, Musca A, et al. How normal is the enthesis by ultrasound in healthy subjects? Clin Exp Rheumatol 2020; 38(3): 472-8.
Wilke J, Macchi V, De Caro R, Stecco C. Fascia thickness, aging and flexibility: is there an association? J Anat 2019; 234(1): 43-9.
Stecco A, Meneghini A, Stern R, Stecco C, Imamura M. Ultrasonography in myofascial neck pain: Randomized clinical trial for diagnosis and follow-up. Surg Radiol Anat 2014; 36(3): 243-53.
Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull 2004; 130(1): 3-18.
García-Sillero M, Benítez-Porres J, GarcíaRomero J, Bonilla DA, Petro JL, Vargas-Molina S. Comparison of interventional strategies to improve recovery after eccentric exerciseinduced muscle fatigue. Int J Environ Res Public Health 2021; 18(2): 1-11.
Konrad A, Glashüttner C, Reiner MM, Bernsteiner D, Tilp M. The acute effects of a percussive massage treatment with a hypervolt device on plantar flexor muscles’ range of motion and performance. J Sport Sci Med 2020; 19(4): 690-4.
Guang H, Ji L, Shi Y. Focal vibration stretches muscle fibers by producing muscle waves. IEEE Trans Neural Syst Rehabil Eng 2018; 26(4): 839-46.
Comeaux Z. Dynamic fascial release and the role of mechanical/vibrational assist devices in manual therapies. J Bodyw Mov Ther 2011; 15(1): 35-41.
Chatchawan U, Jarasrungsichol K, Yamauchi J. Immediate effects of self-thai foot massage on skin blood flow, skin temperature, and range of motion of the foot and ankle in type 2 diabetic patients. J Altern Complement Med 2020; 26(6): 491-500.
Zheng Z, Wang J, Gao Q, Hou J, Ma L, Jiang C, et al. Therapeutic evaluation of lumbar tender point deep massage for chronic non-specific low back pain. J Tradit Chinese Med 2012; 32(4): 534-7.
Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis 1978; 37(4): 378-81.
De Coninck K, Hambly K, Dickinson JW, Passfield L. Measuring the morphological characteristics of thoracolumbar fascia in ultrasound images: An inter-rater reliability study. BMC Musculoskelet Disord 2018; 19(1): 1-6.
Siegmund LA, Barkley JE, Knapp D, Peer KS. Acute effects of local vibration with biomechanical muscle stimulation on low-back flexibility and perceived stiffness. Athl Train Sport Heal Care 2014; 6(1): 1-9.
Wright V. The measurement of back movement. Rheumatology 1983; 22(4): 193-6.
Rezvani A, Ergin O, Karacan I, Oncu M. Validity and reliability of the metric measurements in the assessment of lumbar spine motion in patients with ankylosing spondylitis. Spine (Phila Pa 1976) 2012; 37(19): 1189-96.
Tadmor R, Chen N, Israelachvili JN. Thin film rheology and lubricity of hyaluronic acid solutions at a normal physiological concentration. J Biomed Mater Res 2002; 61(4): 514-23.
Caliandro P, Celletti C, Padua L, Minciotti I, Russo G, Granata G, et al. Focal muscle vibration in the treatment of upper limb spasticity: a pilot randomized controlled trial in patients with chronic stroke. Arch Phys Med Rehabil 2012; 93(9): 1656-61.
Xiong Y, Berrueta L, Urso K, Olenich S, Muskaj I, Badger GJ, et al. Stretching reduces skin thickness and improves subcutaneous tissue mobility in a murine model of systemic sclerosis. Front Immunol 2017; 8(124): 1-11.
Matteini P, Dei L, Carretti E, Volpi N, Goti A, Pini R. Structural behavior of highly concentrated hyaluronan. Biomacromolecules 2009; 10(6): 1516-22.
Schilder A, Magerl W, Hoheisel U, Klein T, Treede RD. Electrical high-frequency stimulation of the human thoracolumbar fascia evokes long-term potentiation-like pain amplification. Pain 2016; 157(10): 2309-17.
Romero-Moraleda B, González-García J, Cuéllar-Rayo Á, Balsalobre-Fernández C, Muñoz-García D, Morencos E. Effects of vibration and non-vibration foam rolling on recovery after exercise with induced muscle damage. J Sport Sci Med 2019; 18(1): 172-80.
Melzack R, Wall PD. Gate Control-Pain mechanisms - a new theory. Science 1965; 150: 971-9.
Guieu R, Tardy-Gervet MF, Giraud P. Substance P-like Immunoreactivity and Analgesic Effects of Vibratory Stimulation on Patients Suffering From Chronic Pain. Can J Neurol Sci 1993; 20(2): 138-41.
Lu X, Wang Y, Lu J, You Y, Zhang L, Zhu D, et al. Does vibration benefit delayed-onset muscle soreness?: a meta-analysis and systematic review. J Int Med Res 2019; 47(1): 3-18.