Outcomes after pharmacoinvasive strategy versus primary PCI in acute ST elevated myocardial infarction: a retrospective study in Saraburi hospital
Keywords:
STEMI, Primary PCI, Pharmacoinvasive, in-hospital mortalityAbstract
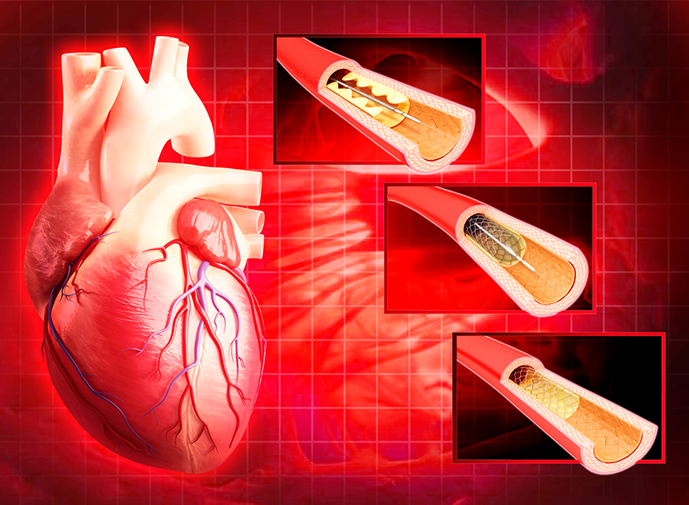
Introduction: ST segment elevation myocardial infarction (STEMI) is a critical cause of sudden cardiac death. Primary percutaneous intervention (PCI) along with balloon angioplasty is the standard recommendation as the first option for treatment. However, there are many limitations to performing PCI such as the lack of hospital readiness for both equipment and personnel. Therefore, a pharmacoinvasive strategy (PI), which refers to administering streptokinase prior to performing PCI, is an alternative option for treating such conditions.
Objective: To compare the in-hospital mortality rate between patients diagnosed with STEMI who underwent primary PCI and those who received PI treatment
Methodology: This is a retrospective cohort study that aimed to collect and analyzed data from electronic medical records of patients diagnosed with and treated for STEMI, either through primary PCI or PI, at Saraburi hospital between 1st January 2021 and 31st December 2022. The study was conducted with the approval of the Ethical review board. Statistical analyses were conducted using both descriptive and analytic methods. Cox-proportional hazard analysis was performed to achieve survival information and hazard ratios using STATA software program.
Results: A total of 249 patients were included in the study. They were divided into a primary PCI group with 79 patients and a PI group with 170 patients. The in-hospital mortality rate was 8.41% with 11 deaths in the primary PCI group and 10 deaths in the PI group. There was no statistically significant difference in mortality rate between these two treatment groups (adjusted HR 0.75, p = 0.74). The primary PCI group had a significantly lower incidence of major bleeding events than the PI group [1.3% vs 4.7%, respectively (HR 0.01, p = 0.01)]. However, the PI group had a shorter duration of total ischemic time, system delay and reperfusion time compared to the primary PCI group (154 vs 219 minutes, p <0.01; 52 vs 105 minutes, p < 0.01; 37 vs 83 minutes, p < 0.01, respectively). The duration of hospital stay did not differ significantly between the two groups (3.9 vs 3 days, p = 0.21).
Conclusion: Patients diagnosed with STEMI who received PI treatment did not have a significantly different in-hospital mortality rate compared to those who underwent primary PCI. Despite providing a shorter duration of total ischemic time and reperfusion time, PI had a higher risk of major bleeding compared to primary PCI.
References
สมาคมแพทย์โรคหัวใจแห่งประเทศไทยในพระบรมราชูปถัมภ์, แนวเวชปฏิบัติการดูแลรักษาผู้ป่วยภาวะหัวใจขาดเลือดเฉียบพลัน พ.ศ.2563, หน้า 7.
Roxana Mehran, Sunil V. Rao, Deepak L. Bhatt, C. Michael Gibson, Adriano Caixeta, John Eikelboom, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consen- sus report from the Bleeding Academic Research Consortium. Circulation. 2011; 123:2736–2747.
Doo Sun Sim, Myung Ho jeong, Youngkeun Ahn, Young Jo Kim, Shung Chull Chae, Taek Jong Hong, et al. Pharmacoinvasive strategy versus primary percutaneous coronary intervention in patients with ST-segment–elevation myocardial infarction: a propensity score–matched analysis. Circulation: Cardiovascular Interventions, 2016;9:e003508.
Paul W. Armstrong, M.D., Anthony H. Gershlick, M.D., Patrick Goldstein, M.D., Robert Wilcox, M.D., Thierry Danays, M.D., Yves Lambert, M.D., et al. Fibrinolysis or Primary PCI in ST-Segment Elevation Myocardial Infarction. N Engl J Med 2013; 368:1379-1387.
Patrick T. O’Gara, Frederick G. Kushner, Deborah D. Ascheim, Donald E. CaseyJr, Mina K. Chung, James A. de Lemos, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127: e362–e425.
Borja Ibanez, Stefan James, Stefan Agewall, Manuel J Antunes, Chiara Bucciarelli-Ducci, Héctor Bueno, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.
Loïc Belle, Guillaume Cayla, Yves Cottin, Pierre Coste, Khalife Khalife, Jean-Noël Labèque, et al. French Registry on Acute ST-elevation and non−ST-elevation Myocardial Infarction 2015 (FAST-MI 2015). Design and baseline data. Archives of Cardiovascular Diseases, 2017 Jun-Jul;110(6-7):366-378.
Brahmajee K Nallamothu, Eric R Bates. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003 Oct 1;92(7):824-6.
Peerawat Jinatongthai, Junporn Kongwatcharapong, Chee Yoong Foo, Arintaya Phrommintikul, Surakit Nathisuwan, Ammarin Thakkinstian, et al. Comparative efficacy and safety of reperfusion therapy with fibrinolytic agents in patients with ST-segment elevation myocardial infarction: a systematic review and network meta-analysis. Lancet. 2017 Aug 19;390(10096):747-759.
Patrick T O'Gara, Frederick G Kushner, Deborah D Ascheim, Donald E Casey Jr, Mina K Chung, James A de Lemos, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Jan 29;61(4): e78-e140.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Rathaphong Lertwichitsilp

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Journal of TCI is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) licence, unless otherwise stated. Please read our Policies page for more information.





