The study of association between duration of diagnosis to treatments and mortality among advanced stage non-small cell lung cancer in Saraburi hospital
Keywords:
Non-small cell lung cancer, Advanced stage CA lung, duration of diagnosis and treatment, mortality rateAbstract
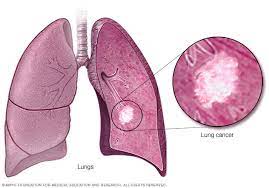
Lung cancer accounts for high mortality rate. The study aims to investigate the association between duration of diagnosis to treatments, other factors, and mortality among 255 patients diagnosed with advanced stage non-small cell lung cancer (NSCLC) from 1st January 2014 to 31st December 2019. This is a retrospective cohort study. Risks of dying from lung cancer were assess using Cox with time varying covariates. Patient data was obtained from electronic medical records and the National Cancer Registry of Thailand. The mortality rate of lung cancer in Saraburi province was 1.5 per 100 person-month and 1-year, 3-year, and 5-year mortality was 58.8%, 91.3% and 95% respectively. In univariate analysis, mortality of lung cancer is associated with longer waiting period for any services. The mortality rate is almost 3 times higher if the waiting time between the 1st visit and the diagnosis is more than 4 weeks, compared to shorter waiting time [HR 2.81 (95%CI 1.95-4.04)]. Longer waiting period for tissue diagnosis more than 2 weeks is also associated with higher mortality [HR 2.79 (95%CI 1.85-4.21)]. Furthermore, the waiting period between the diagnosis and the 1st treatment for more than 4 weeks and the waiting period between the 1st visit and the 1st treatment for more than 6 weeks are associated with higher mortality rate [HR 1.50 (95%CI 1.11-2.02) and HR 2.63 (95%CI 1.70-4.08) respectively]. In multivariate analysis, these timing factors do not reach statistical significance but patients who did not receive any systemic treatments demonstrate the strongest mortality rate [adjusted HR 4.10 (95%CI 2.32-7.24)]. Among 172 patients receiving treatments for lung cancer, those receiving external beam radiation therapy has higher mortality rate than others [HR 3.00 (95%CI 1.12-8.02)]. In conclusion, longer waiting period in any process show trends to impact mortality rate although did not reach statistical significance in multivariate analysis. The other cell types apart from adenocarcinoma and squamous cell carcinoma associate with higher mortality. Patients who did not receive systemic therapy have higher mortality rate than those who received.
References
P. W Imsamran, A Pattatang, P Supattagorn, I Chiawiriyabunya K. Namthaisong M. Wongsena P., Cancer in Thailand Vol.IX, Cancer สถาบันมะเร็งแห่งชาติ, ทะเบียนมะเร็งระดับโรงพยาบาล พ.ศ. 2561, สถาบันมะเร็งแห่งชาติ กรมการแพทย์ กระทรวงสาธารณสุข, 2562. http://www.nci.go.th/th/File_download/Nci Cancer Registry/Hospital Based_2018.pdf.
C.F. Mountain, The international system for staging lung cancer, Seminars in Surgical Oncology. 18 (2000) 106. https://doi.org/10.1002/(sici)1098-2388(200003)18:2<106::aid-ssu4>3.3.co;2-g.
F. Venuta, D. Diso, I. Onorati, M. Anile, S. Mantovani, E.A. Rendina, Lung cancer in elderly patients, Journal of Thoracic Disease. 8 (2016) S908–S914. https://doi.org/10.21037/jtd.2016.05.20.
F. Tas, R. Ciftci, L. Kilic, S. Karabulut, Age is a prognostic factor affecting survival in lung cancer patients, Oncology Letters. 6 (2013) 1507–1513. https://doi.org/10.3892/ol.2013.1566.
S.H. Feng, S.T. Yang, The new 8th tnm staging system of lung cancer and its potential imaging interpretation pitfalls and limitations with ct image demonstrations, Diagnostic and Interventional Radiology. 25 (2019) 270–279. https://doi.org/10.5152/dir.2019.18458.
S.M. Lichtman, H. Wildiers, E. Chatelut, C. Steer, D. Budman, V.A. Morrison, B. Tranchand, I. Shapira, M. Aapro, International society of geriatric oncology chemotherapy taskforce: Evaluation of chemotherapy in older patients - An analysis of the medical literature, Journal of Clinical Oncology. 25 (2007) 1832–1843. https://doi.org/10.1200/JCO.2007.10.6583.
Y. Ito, Y. Ohno, B. Rachet, M.P. Coleman, H. Tsukuma, A. Oshima, Cancer survival trends in Osaka, Japan: The influence of age and stage at diagnosis, Japanese Journal of Clinical Oncology. 37 (2007) 452–458. https://doi.org/10.1093/jjco/hym047.
C.M. Tammemagi, C. Neslund-Dudas, M. Simoff, P. Kvale, Smoking and Lung Cancer Survival: The Role of Comorbidity and Treatment, Chest. 125 (2004) 27–37. https://doi.org/10.1378/chest.125.1.27.
I. Yoshino, D. Kawano, T. Oba, K. Yamazaki, T. Kometani, Y. Maehara, Smoking status as a prognostic factor in patients with stage I pulmonary adenocarcinoma, Annals of Thoracic Surgery. 81 (2006) 1189–1193. https://doi.org/10.1016/j.athoracsur.2005.09.028.
R. Mäkitaro, P. Pääkko, E. Huhti, R. Bloigu, V.L. Kinnula, Prospective population-based study on the survival of patients with lung cancer, European Respiratory Journal. 19 (2002) 1087–1092. https://doi.org/10.1183/09031936.02.00048302.
A. Joshi, R. Mishra, S. Desai, P. Chandrani, H. Kore, R. Sunder, S. Hait, P. Iyer, V. Trivedi, A. Choughule, V. Noronha, A. Joshi, V. Patil, N. Menon, R. Kumar, K. Prabhash, A. Dutt, Molecular characterization of lung squamous cell carcinoma tumors reveals therapeutically relevant alterations, Oncotarget. 12 (2021) 578–588. https://doi.org/10.18632/ONCOTARGET.27905.
A.K. Vaid, A. Gupta, G. Momi, Overall survival in stage IV EGFR mutation-positive NSCLC: Comparing first-, second- And third-generation EGFR-TKIs (Review), International Journal of Oncology. 58 (2021) 171–184. https://doi.org/10.3892/ijo.2021.5168.
R. Salloum, Survival among Non-Small Cell Lung Cancer Patients with Poor Performance Status after First Line Chemotherapy, Lung Cancer. 77 (2012) 1–12. https://doi.org/10.1016/j.lungcan.2012.04.019.
C. Owusuaa, S.A. Dijkland, D. Nieboer, A. van der Heide, C.C.D. van der Rijt, Predictors of Mortality in Patients with Advanced Cancer—A Systematic Review and Meta-Analysis, Cancers. 14 (2022) 1–20. https://doi.org/10.3390/cancers14020328.
A.C. Obenauf, J. Massagué, Surviving at a Distance: Organ-Specific Metastasis, Trends in Cancer. 1 (2015) 76–91. https://doi.org/10.1016/j.trecan.2015.07.009.
O.H. Gómez, A.M. Paul, A.L.O. Granados, S.R. Martínez, D.P. Parente, P.R. Gracia, L.S. Cuervo-Arango, L. Vilà, “High Tumor Burden” in Metastatic Non-Small Cell Lung Cancer: Defining the Concept, Cancer Management and Research. 13 (2021) 4665–4670. https://doi.org/10.2147/CMAR.S302928.
D.R. Gomez, K.P. Liao, S.G. Swisher, G.R. Blumenschein, J.J. Erasmus, T.A. Buchholz, S.H. Giordano, B.D. Smith, Time to treatment as a quality metric in lung cancer: Staging studies, time to treatment, and patient survival, Radiotherapy and Oncology. 115 (2015) 257–263. https://doi.org/10.1016/j.radonc.2015.04.010.
V. Vichapat, Prognostic Factors and Overall Survival of Advanced Stage NSCLC Patients in Saraburi Hospital, J Dept Med Ser. 46 (2021) D. Ha, A.L. Ries, P. Montgrain, F. Vaida, S. Sheinkman, M.M. Fuster, Time to treatment and survival in veterans with lung cancer eligible for curative intent therapy, Respiratory Medicine. 141 (2018) 172–179. https://doi.org/10.1016/j.rmed.2018.07.005.
H. Bozcuk, C. Martin, Does treatment delay affect survival in non-small cell lung cancer? A retrospective analysis from a single UK centre, Lung Cancer. 34 (2001) 243–252. https://doi.org/10.1016/S0169-5002(01)00247-1.
TCB Report Online, Thai population cancer database, National Cancer Institute. (2020). http://tcb.nci.go.th/CWEB/cwebBase.do?mode=initialApplication (accessed April 9, 2020).
P. Goldstraw, K. Chansky, J. Crowley, The IASLC lung cancer staging project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM Classification for lung cancer, Journal of Thoracic Oncology. 11 (2016) 39–51. https://doi.org/10.1016/j.jtho.2015.09.009.
C. Ruhe, Estimating survival functions after stcox with time-varying coefficients, Stata Journal. 16 (2016) 867–879. https://doi.org/10.1177/1536867x1601600404.
StataCorp, Stata Statistical Software: Release 14, (2015).
S.Y. Brule, K. Al-Baimani, H. Jonker, T. Zhang, G. Nicholas, G. Goss, S.A. Laurie, P. Wheatley-Price, Palliative systemic therapy for advanced non-small cell lung cancer: Investigating disparities between patients who are treated versus those who are not, Lung Cancer. 97 (2016) 15–21. https://doi.org/10.1016/j.lungcan.2016.04.007.
T.Y.D. Cheng, S.M. Cramb, P.D. Baade, D.R. Youlden, C. Nwogu, M.E. Reid, The international epidemiology of lung cancer: Latest trends, disparities, and tumor characteristics, Journal of Thoracic Oncology. 11 (2016) 1653–1671. https://doi.org/10.1016/j.jtho.2016.05.021.
Visbal AL, Williams BA, Nichols FC 3rd, Marks RS, Jett JR, Aubry MC, Edell ES, Wampfler JA, Molina JR, Yang P. Gender differences in non-small-cell lung cancer survival: an analysis of 4,618 patients diagnosed between 1997 and 2002. Ann Thorac Surg. 2004 Jul;78(1):209-15; discussion 215. https://doi.org/10.1016/j.athoracsur.2003.11.021.
Islam KM, Jiang X, Anggondowati T, Lin G, Ganti AK. Comorbidity and Survival in Lung Cancer Patients. Cancer Epidemiol Biomarkers Prev. 2015 Jul;24(7):1079-85. https://doi.org/10.1158/1055-9965.EPI-15-0036.
Travis WD, Brambilla E, Geisinger KR. Histological grading in lung cancer: one system for all or separate systems for each histological type? Eur Respir J. 2016 Mar;47(3):720-3. https://doi.org/10.1183/13993003.00035-2016.
Fukuoka M, Wu YL, Thongprasert S, Sunpaweravong P, Leong SS, Sriuranpong V, Chao TY, Nakagawa K, Chu DT, Saijo N, Duffield EL, Rukazenkov Y, Speake G, Jiang H, Armour AA, To KF, Yang JC, Mok TS. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol. 2011 Jul 20;29(21):2866-74. https://doi.org/10.1200/JCO.2010.33.4235.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, Zhang S, Wang J, Zhou S, Ren S, Lu S, Zhang L, Hu C, Hu C, Luo Y, Chen L, Ye M, Huang J, Zhi X, Zhang Y, Xiu Q, Ma J, Zhang L, You C. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011 Aug;12(8):735-42. https://doi.org/10.1016/S1470-2045(11)70184-X.
S.K. Vinod, A. Chandra, A. Berthelsen, J. Descallar, Does timeliness of care in Non-Small Cell Lung Cancer impact on survival?, Lung Cancer. 112 (2017) 16–24. https://doi.org/10.1016/j.lungcan.2017.07.032.
C. Labbé, M. Anderson, S. Simard Msc, L. Tremblay, F. Laberge, R. Vaillancourt, Y. Lacasse, Wait times for diagnosis and treatment of lung cancer: A single-centre experience, Current Oncology. 24 (2017) 367–373. https://doi.org/10.3747/co.24.3655.
C.H. Tsai, P.T. Kung, W.Y. Kuo, W.C. Tsai, Effect of time interval from diagnosis to treatment for non-small cell lung cancer on survival: A national cohort study in Taiwan, BMJ Open. 10 (2020) 1–10. https://doi.org/10.1136/bmjopen-2019-034351.
S. Peters, C. Bexelius, V. Munk, N. Leighl, The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer, Cancer Treatment Reviews. 45 (2016) 139–162. https://doi.org/10.1016/j.ctrv.2016.03.009.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Journal of TCI is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) licence, unless otherwise stated. Please read our Policies page for more information.





