Prevalence and Associated Factors of Contrast-Associated Acute Kidney Injury in Kidney Disease: A Retrospective Cohort Study
Main Article Content
Abstract
Background: Research indicates that the intravascular administration of contrast agents during computed tomography (CT) procedures may lead to Contrast-Associated Acute Kidney Injury (CA-AKI). The prevalence and associated risk factors for CA-AKI vary among different populations, particularly in individuals with pre-existing kidney disease.
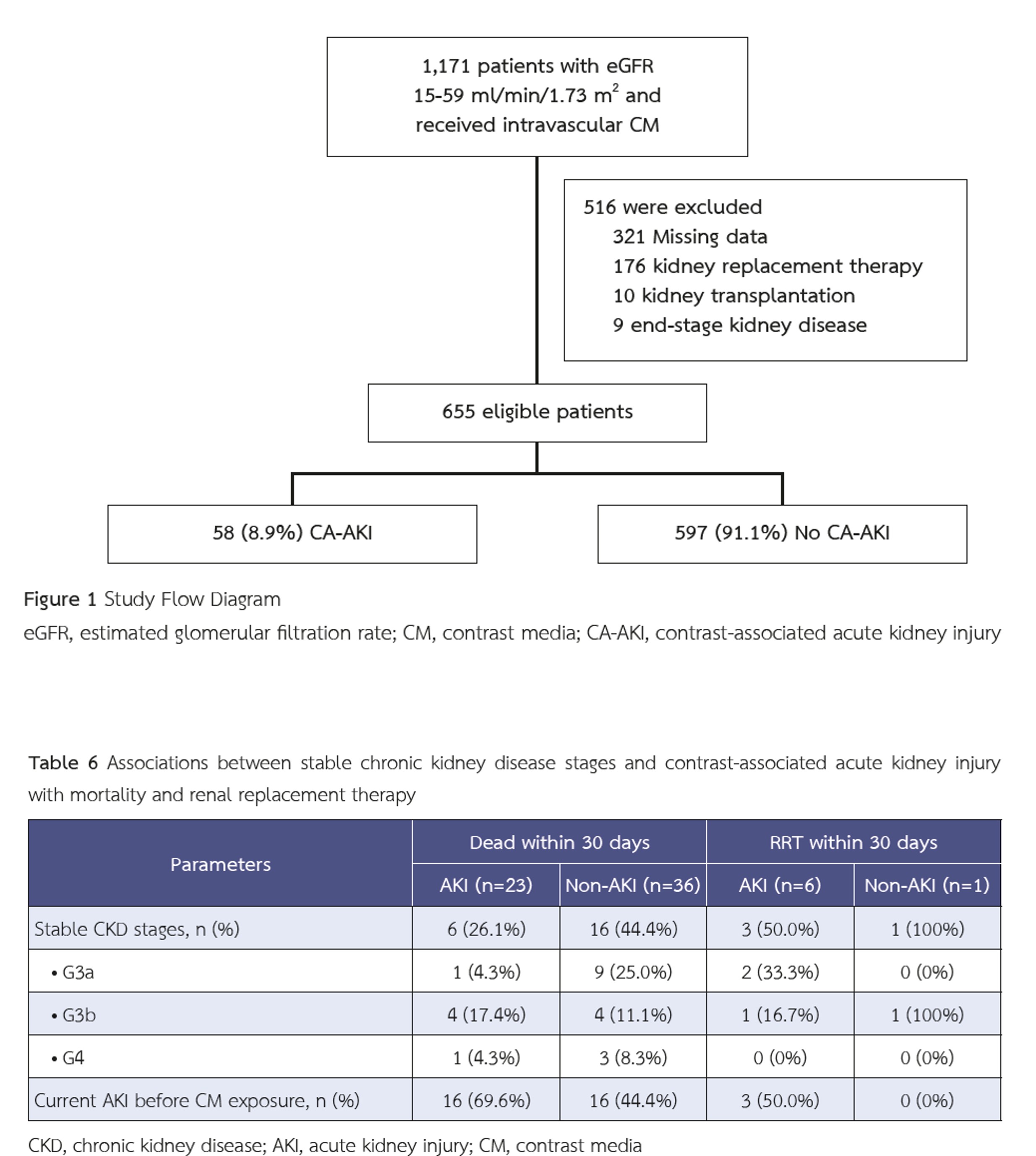
Methods: This retrospective cohort study included patients with an estimated glomerular filtration rate (eGFR) between 15 and 59 mL/min/1.73 m² who received intravenous contrast medium (CM) for CT between October 2021 and September 2024. The prevalence of CA-AKI in patients with kidney disease was evaluated, and associated risk factors were analyzed.
Results: A total of 655 patients met the inclusion criteria. Among them, 58 patients (8.58%) developed CA-AKI. Baseline demographic characteristics were not significantly different between the CA-AKI and non-CA-AKI groups. However, the CA-AKI group had significantly higher proportions of patients with chronic kidney disease (CKD) stage G3b and G4, current use of diuretics and vasopressors, multiple exposures to CM within 72 hours, and concurrent acute kidney injury (AKI). Multivariate analysis identified CKD stage G3b (odds ratio [OR] 2.75; 95% confidence interval [CI], 1.26–6.00; p = 0.011) and current AKI (OR 3.99; 95% CI, 1.89–8.42; p < 0.001) as significant factors associated with the development of CA-AKI.
Conclusions: CKD stage G3b and current AKI were significantly associated with an increased risk of CA-AKI. Therefore, caution is warranted when administering CM to patients with these conditions.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 2012;120(4):c179–84. doi: 10.1159/000339789.American college of radiology. ACR manual on contrast media. ACR. 2023:40-6.
American college of radiology. ACR manual on contrast media. ACR. 2023:40-6.
Rachoin JS, Wolfe Y, Patel S, Cerceo E. Contrast associated nephropathy after intravenous administration: what is the magnitude of the problem? Ren Fail 2021;43(1):1311–21. doi: 10.1080/0886022X.2021.1978490.
European society of urogenital radiology. ESUR guidelines on contrast agents. ESUR. 2018:18-20.
Davenport MS, Perazella MA, Yee J, Dillman JR, Fine D, McDonald RJ, et al. Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation. Radiology 2020;294(3):660–8. doi: 10.1148/radiol.2019192094.
Isaka Y, Hayashi H, Aonuma K, Horio M, Terada Y, Doi K, et al. Guideline on the use of iodinated contrast media in patients with kidney disease 2018. Clin Exp Nephrol 2020;24(1):1–44. doi: 10.1007/s10157-019-01750-5.
Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH. Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology 2013;268(3):719–28. doi: 10.1148/radiol.13122276.
Dekkers IA, van der Molen AJ. Propensity Score Matching as a Substitute for Randomized Controlled Trials on Acute Kidney Injury After Contrast Media Administration: A Systematic Review. AJR Am J Roentgenol 2018;211(4):822–6. doi: 10.2214/AJR.17.19499.
McDonald JS, McDonald RJ, Lieske JC, Carter RE, Katzberg RW, Williamson EE, et al. Risk of Acute Kidney Injury, Dialysis, and Mortality in Patients With Chronic Kidney Disease After Intravenous Contrast Material Exposure. Mayo Clin Proc 2015;90(8):1046–53. doi: 10.1016/j.mayocp.2015.05.016.
Kidoh M, Nakaura T, Awai K, Matsunaga Y, Tanoue K, Harada K, et al. Low-contrast dose protection protocol for diagnostic computed tomography in patients at high-risk for contrastinduced nephropathy. J Comput Assist Tomogr 2013;37(2):289–96. doi: 10.1097/RCT.0b013e318279bd20.
Enderlein G. Daniel, Wayne W.: Biostatistics — A Foundations for Analysis in the Health Sciences. Wiley & Sons, New York—Chichester—Brisbane—Toronto—Singapore, 6th ed. 1995, 780 S.,£58.—, ISBN 0–471–58852-0 (cloth). Biometrical Journal 2007;37(6):744–. doi: 10.1002/bimj.4710370610.
McDonald JS, McDonald RJ, Williamson EE, Kallmes DF, Kashani K. Post-contrast acute kidney injury in intensive care unit patients: a propensity score-adjusted study. Intensive Care Med 2017;43(6):774–84. doi: 10.1007/s00134-017-4699-y.
Stacul F, Bertolotto M, Thomsen HS, Pozzato G, Ugolini D, Bellin MF, et al. Iodine-based contrast media, multiple myeloma and monoclonal gammopathies: literature review and ESUR Contrast Media Safety Committee guidelines. Eur Radiol 2018;28(2):683–91. doi: 10.1007/s00330-017-5023-5.
Crowley MP, Prabhakaran VN, Gilligan OM. Incidence of Contrast-Induced Nephropathy in Patients with Multiple Myeloma Undergoing Contrast-Enhanced Procedures. Pathol Oncol Res 2018;24(4):915–9. doi: 10.1007/s12253-017-0300-9.