Comparative Anatomy of the Right and Left Internal Jugular Veins: Implications for Optimal Central Venous Catheter Placement
Main Article Content
Abstract
Background: Central venous catheters are essential for dialysis, with the internal jugular vein (IJV) being the preferred access site. Recognizing anatomical variations of the IJV is crucial to avoid accidental arterial puncture. This study aims to describe anatomical variations of the right and left IJVs.
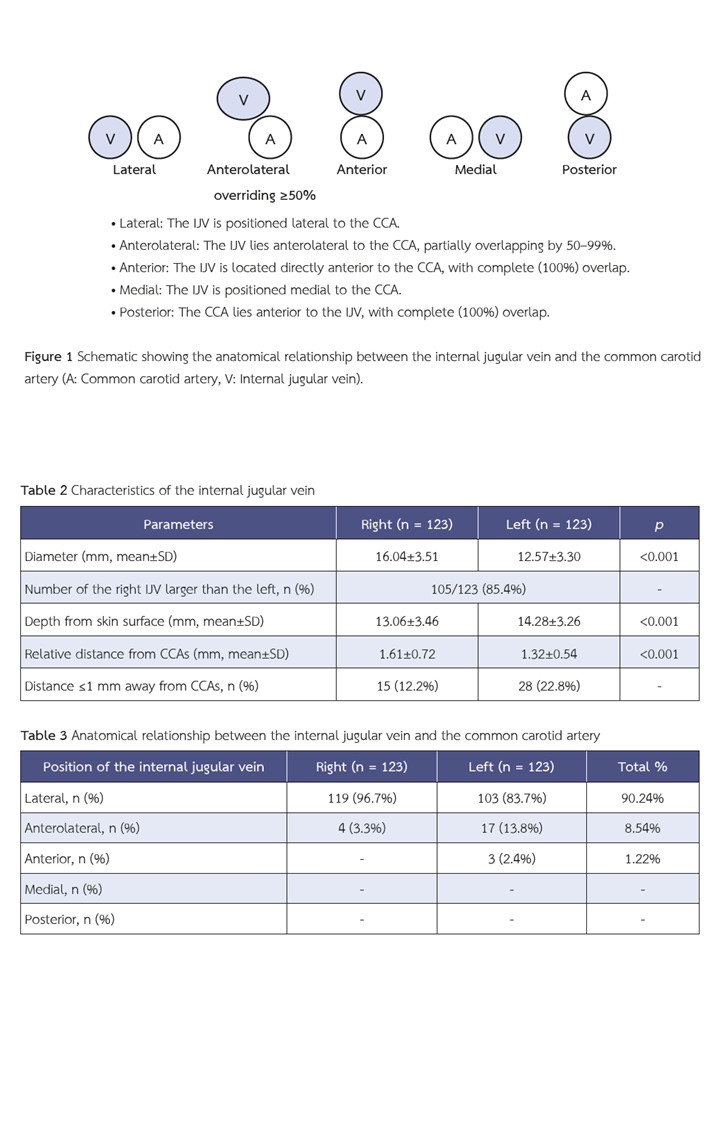
Methods: We retrospectively reviewed neck CT scans from 123 patients who underwent imaging at our hospital between January 1, 2015, and December 31, 2019. We recorded the bilateral IJV diameter, depth from the skin, distance to the common carotid artery (CCA), and the IJV’s positional relationship to the CCA. The IJV’s position relative to the CCA was classified as lateral, anterior, anterolateral, medial, or posterior, based on its location at the level of the cricoid cartilage.
Results: Most IJVs (90.24%) were positioned lateral to the CCA, with the left side demonstrating greater anatomical variation. The left IJV overlapped the CCA more frequently than the right in the anterolateral position, and only left IJVs were found in the anterior position. Right IJVs were larger in 85.4% of patients, with a significantly greater mean diameter (16.04±3.51 mm vs. 12.57±3.30 mm, p<0.001) and were more superficial (13.06±3.46 mm vs.14.28±3.26 mm, p <0.001) compared to the left.
Conclusions: Due to less anatomical variability and a more favorable puncture site, the right IJV is generally more suitable for vascular access than the left.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011) 2022;12(1):7–11. doi: 10.1016/j.kisu.2021.11.003.
Kidney Disease: Improving Global Outcomes CKDWG. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int 2024;105(4S):S117–S314. doi: 10.1016/j.kint.2023.10.018.
Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis 2020;75(4 Suppl 2):S1–S164. doi: 10.1053/j.ajkd.2019.12.001.
McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003;348(12):1123–33. doi: 10.1056/NEJMra011883.
Vats HS. Complications of catheters: tunneled and nontunneled. Adv Chronic Kidney Dis 2012;19(3):188–94. doi: 10.1053/j.ackd.2012.04.004.
Schillinger F, Schillinger D, Montagnac R, Milcent T. Post catheterisation vein stenosis in haemodialysis: comparative angiographic study of 50 subclavian and 50 internal jugular accesses. Nephrol Dial Transplant 1991;6(10):722–4. doi: 10.1093/ndt/6.10.722.
Bowdle A. Vascular complications of central venous catheter placement: evidence-based methods for prevention and treatment. J Cardiothorac Vasc Anesth 2014;28(2):358–68. doi: 10.1053/j.jvca.2013.02.027.
Safety Committee of Japanese Society of A. Practical guide for safe central venous catheterization and management 2017. J Anesth 2020;34(2):167–86. doi: 10.1007/s00540-019-02702-9.
Lim CL, Keshava SN, Lea M. Anatomical variations of the internal jugular veins and their relationship to the carotid arteries: a CT evaluation. Australas Radiol 2006;50(4):314–8. doi: 10.1111/j.1440-1673.2006.01589.x.
Maneenai N, Arjhansiri K. CT evaluation of anatomical variations of the internal jugular veins in Thai adults. Asian Biomedicine 2013;7(6):803–11. doi: 10.5372/1905-7415.0706.243.
Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. Int J Crit Illn Inj Sci 2015;5(3):170–8. doi: 10.4103/2229-5151.164940.
Jin Lee J, Sook Gwak M, Yang M, Soo Kim G. A new method of internal jugular vein catheterization using the cricoid cartilage and the external jugular vein as a landmark. Am J Emerg Med 2006;24(6):697–701. doi: 10.1016/j.ajem.2006.03.005.
Buch K, Groller R, Nadgir RN, Fujita A, Qureshi MM, Sakai O. Variability in the Cross-Sectional Area and Narrowing of the Internal Jugular Vein in Patients Without Multiple Sclerosis. AJR Am J Roentgenol 2016;206(5):1082–6. doi: 10.2214/AJR.15.14689.
Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy 2011;4:27–39. doi: 10.2147/RMHP.S10383.
Ayres A, van Tonder DJ, van Schoor A-N. Anatomical analysis of Sedillot’s triangle as a reliable landmark for insertion of central venous catheters in neonates using a central approach. Translational Research in Anatomy 2023;33:100264. doi: 10.1016/j.tria.2023.100264.
Troianos CA, Kuwik RJ, Pasqual JR, Lim AJ, Odasso DP. Internal jugular vein and carotid artery anatomic relation as determined by ultrasonography. Anesthesiology 1996;85(1):43–8. doi: 10.1097/00000542-199607000-00007.
Lin BS, Kong CW, Tarng DC, Huang TP, Tang GJ. Anatomical variation of the internal jugular vein and its impact on temporary haemodialysis vascular access: an ultrasonographic survey in uraemic patients. Nephrol Dial Transplant 1998;13(1):134–8. doi: 10.1093/ndt/13.1.134.
Saugel B, Scheeren TWL, Teboul JL. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Crit Care 2017;21(1):225. doi: 10.1186/s13054-017-1814-y.
Sulek CA, Blas ML, Lobato EB. A randomized study of left versus right internal jugular vein cannulation in adults. J Clin Anesth 2000;12(2):142–5. doi: 10.1016/s0952-8180(00)00129-x.
Asouhidou I, Natsis K, Asteri T, Sountoulides P, Vlasis K, Tsikaras P. Anatomical variation of left internal jugular vein: clinical significance for an anaesthesiologist. Eur J Anaesthesiol 2008;25(4):314–8. doi: 10.1017/S0265021508003700.
Saiki K, Tsurumoto T, Okamoto K, Wakebe T. Relation between bilateral differences in internal jugular vein caliber and flow patterns of dural venous sinuses. Anat Sci Int 2013;88(3):141–50. doi: 10.1007/s12565-013-0176-z.
Kosnik N, Kowalski T, Lorenz L, Valacer M, Sakthi-Velavan S. Anatomical review of internal jugular vein cannulation. Folia Morphol (Warsz) 2024;83(1):1–19. doi: 10.5603/FM.a2023.0008.
Lorchirachoonkul T, Ti LK, Manohara S, Lye ST, Tan SA, Shen L, et al. Anatomical variations of the internal jugular vein: implications for successful cannulation and risk of carotid artery puncture. Singapore Med J 2012;53(5):325–8.
Patel AR, Patel AR, Singh S, Singh S, Khawaja I. Central Line Catheters and Associated Complications: A Review. Cureus 2019;11(5):e4717. doi: 10.7759/cureus.4717.
Kwon SS, Falk A, Mitty HA. Thoracic duct injury associated with left internal jugular vein catheterization: anatomic considerations. J Vasc Interv Radiol 2002;13(3):337–9. doi: 10.1016/s1051-0443(07)61730-8.
Merritt RL, Hachadorian ME, Michaels K, Zevallos E, Mhayamaguru KM, Closser Z, et al. The Effect of Head Rotation on the Relative Vascular Anatomy of the Neck: Implications for Central Venous Access. J Emerg Trauma Shock 2018;11(3):193–6. doi: 10.4103/JETS.JETS_5_18.