Tumor-induced Osteomalacia with Proximal Tubulopathy: A Case Report
Main Article Content
Abstract
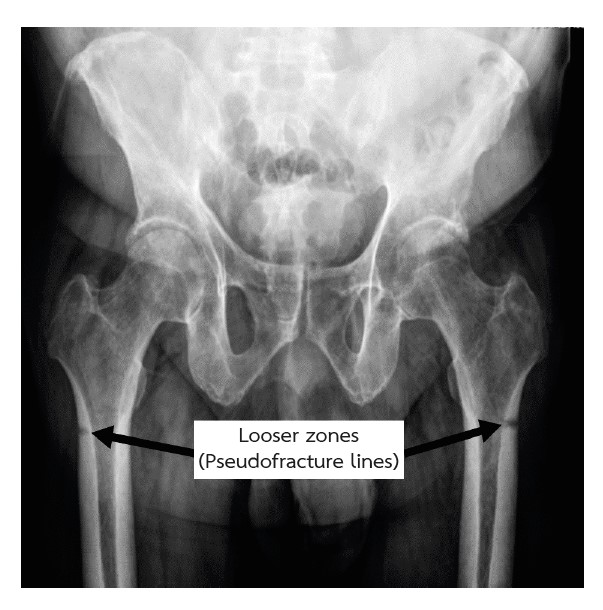
Tumor-induced osteomalacia (TIO) is a rare paraneoplastic syndrome that poses diagnostic challenges. Most patients present with symptoms such as bone pain, fractures, or muscle weakness, which are caused by the tumor’s production of fibroblast growth factor-23 (FGF-23). This phosphaturic hormone decreases the expression of type 2 sodium-phosphate cotransporters (NaPi-2a and NaPi-2c) in the kidney’s proximal tubule, leading to hypophosphatemia due to increased phosphate excretion. Additionally, FGF-23 inhibits the enzyme 1α-hydroxylase (CYP27B1), which converts 25(OH)D to the active form of vitamin D, 1,25(OH)2D, while stimulating the enzyme 24-hydroxylase (CYP24A1), which increases the breakdown of 1,25(OH)2D. This reduction in active vitamin D contributes to the development of osteomalacia. Diagnosing TIO is often delayed due to the small size of the tumor, which is difficult to locate, and the non-specific symptoms. This article reports the case of a 58-year-old man who experienced bilateral thigh pain for three years. Initially diagnosed with osteoporosis, he was treated with pain medication, anti-resorptive therapy, and physical therapy. However, eight months before admission, his thigh pain worsened, and he had difficulty walking. Laboratory tests revealed renal phosphate wasting, hypophosphatemia, and elevated levels of intact FGF-23. Additionally, proteinuria, glucosuria, and elevated urine beta-2 microglobulin indicated proximal tubulopathy. A 99mTc-Hynic-TOC scan with SPECT/CT revealed increased uptake in the right medial thigh. He was diagnosed with TIO and Fanconi syndrome.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Bosman A, Palermo A, Vanderhulst J, De Beur SMJ, Fukumoto S, Minisola S, et al. Tumor-Induced Osteomalacia: A Systematic Clinical Review of 895 Cases. Calcif Tissue Int. 2022;111(4):367-79.
Florenzano P, Gafni RI, Collins MT. Tumor-induced osteomalacia. Bone Rep. 2017;7:90-7.
Yin Z, Du J, Yu F, Xia W. Tumor-induced osteomalacia. Osteoporos Sarcopenia. 2018;4(4):119-27.
Aligail K, Dave JA, Ross IL. Tumor-induced osteomalacia: a case report. J Med Case Rep. 2022;16(1):22.
Agarwal A, Bathla G, Gupta V. Tumor-induced Osteomalacia Secondary to Phosphaturic Mesenchymal Tumor. Radiol Imaging Cancer. 2023;5(2):e220170.
Bacchetta J, Salusky IB. Evaluation of hypophosphatemia: lessons from patients with genetic disorders. Am J Kidney Dis. 2012;59(1):152-9.
Beil FT, Sturznickel J, Rolvien T, Amling M, Oheim R. [Tumor localization and treatment of tumor-induced osteomalacia]. Z Rheumatol. 2022;81(3):182-8.
Minisola S, Peacock M, Fukumoto S, Cipriani C, Pepe J, Tella SH, et al. Tumour-induced osteomalacia. Nat Rev Dis Primers. 2017;3(1):17044.
Cianferotti L. Osteomalacia Is Not a Single Disease. Int J Mol Sci. 2022;23(23).
Tile L, Cheung AM. Atypical femur fractures: current understanding and approach to management. Ther Adv Musculoskelet Dis. 2020;12:1759720X20916983.
Liu L, Li C, Yang P, Zhu J, Gan D, Bu L, et al. Association between alendronate and atypical femur fractures: a meta-analysis. Endocr Connect. 2015;4(1):58-64.
Chong WH, Yavuz S, Patel SM, Chen CC, Collins MT. The importance of whole body imaging in tumor-induced osteomalacia. J Clin Endocrinol Metab. 2011;96(12):3599-600.
Crotti C, Bartoli F, Coletto LA, Manara M, Marini E, Daolio PA, et al. Tumor induced osteomalacia: A single center experience on 17 patients. Bone. 2021;152:116077.
Takeuchi Y, Suzuki H, Ogura S, Imai R, Yamazaki Y, Yamashita T, et al. Venous sampling for fibroblast growth factor-23 confirms preoperative diagnosis of tumor-induced osteomalacia. J Clin Endocrinol Metab. 2004;89(8):3979-82.
David WM, Arthur DM. 27 - Hypophosphatemia. 2018:280-6.e1.
Norden AG, Laing RJ, Rowe P, Unwin RJ, Wrong O, Crisp AJ. Oncogenic osteomalacia, raised FGF-23, and renal Fanconi syndrome. QJM. 2014;107(2):139-41.
Gou M, Ma Z. Osteomalacia, renal Fanconi syndrome, and bone tumor. J Int Med Res. 2018;46(8):3487-90.
Leehey DJ, Ing TS, Daugirdas JT. Fanconi syndrome associated with a non-ossifying fibroma of bone. Am J Med. 1985;78(4):708-10.
Farrow EG, White KE. Tumor-induced osteomalacia. Expert Rev Endocrinol Metab. 2009;4(5):435-42.
Chong WH, Molinolo AA, Chen CC, Collins MT. Tumor-induced osteomalacia. Endocr Relat Cancer. 2011;18(3):R53-77.
Zhang Z, Li J, Zhang Z, Shao Z. Tumor-induced Osteomalacia: A Case Report and Etiological Analysis with Literature Review. Orthop Surg. 2023;15(12):3342-52.
Smith ER, Cai MM, McMahon LP, Holt SG. Biological variability of plasma intact and C-terminal FGF23 measurements. J Clin Endocrinol Metab. 2012;97(9):3357-65.
Koumakis E, Cormier C, Roux C, Briot K. The Causes of Hypo- and Hyperphosphatemia in Humans. Calcif Tissue Int. 2021;108(1):41-73.
Laurent MR, De Schepper J, Trouet D, Godefroid N, Boros E, Heinrichs C, et al. Consensus Recommendations for the Diagnosis and Management of X-Linked Hypophosphatemia in Belgium. Front Endocrinol (Lausanne). 2021;12:641543.
Geerse DA, Bindels AJ, Kuiper MA, Roos AN, Spronk PE, Schultz MJ. Treatment of hypophosphatemia in the intensive care unit: a review. Crit Care. 2010;14(4):R147.
Felsenfeld AJ, Levine BS. Approach to treatment of hypophosphatemia. Am J Kidney Dis. 2012;60(4):655-61.
Minisola S, Fukumoto S, Xia W, Corsi A, Colangelo L, Scillitani A, et al. Tumor-induced Osteomalacia: A Comprehensive Review. Endocr Rev. 2023;44(2):323-53.