Sodium-Glucose Cotransporter 2 Inhibitors in Acute Kidney Injury
Main Article Content
Abstract
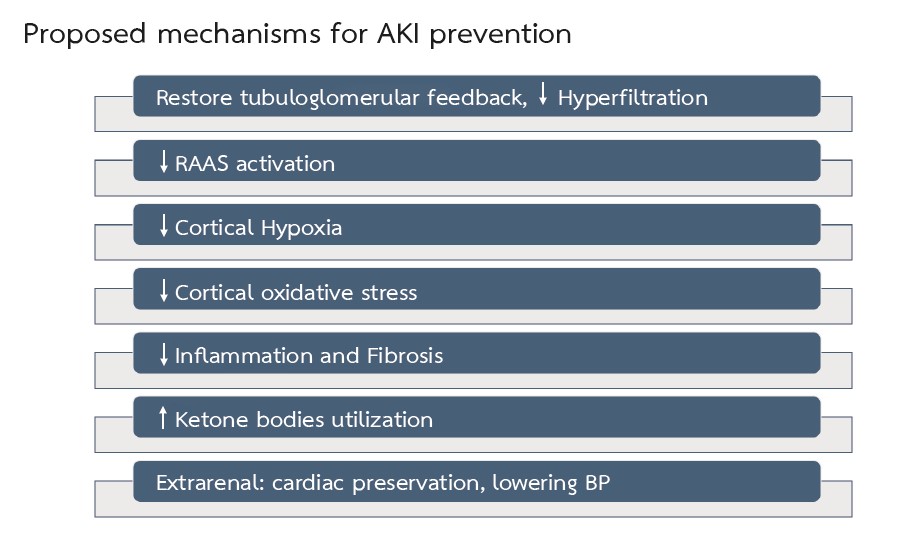
Acute kidney injury (AKI) is a common complication in hospitalized patients and is associated with an increase in morbidity and mortality. Moreover, patients with a history of AKI have an increased risk for congestive heart failure, rehospitalization, recurrence of AKI, progression to chronic kidney disease, and end-stage kidney disease. Currently, there is no specific treatment for post-AKI survivors. Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors, a new and promising drug class, have now been widely used to control blood sugar, delay chronic kidney disease progression, and improve cardiovascular outcomes. By blocking the SGLT2 cotransporter at the proximal tubules, SGLT2 inhibitors result in glucosuria and natriuresis. In addition to lowering blood glucose levels, the drugs enhance the diuretic effect, minimize intravascular and interstitial volume overload, and reduce sympathetic activity. In the heart, SGLT2 inhibitors reduce oxidative stress and inflammation, which are protective against cardiac injury. The inhibition of Na+/H+ exchanger in cardiomyocytes can also reduce congestive heart failure. In the kidneys, SGLT2 inhibitors can reduce oxygen consumption in the renal cortex. There is currently no direct evidence regarding the protective effect of SGLT2 inhibitors in AKI. However, these promising mechanisms and other indirect evidence suggest that SGLT2 inhibitors may help improve long-term outcomes in patients with AKI.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Carlos AC, Eva R, Sheila B, Adriana S, Carla B, Clara B, et al. Short- and long-term outcomes after non-severe acute kidney injury. Clin Exp Nephrol. 2018;22(1):61-7.
Gayat E, Hollinger A, Cariou A. Deye N, Vieillard-Baron A, Jaber S, et al. Impact of angiotensin-converting enzyme inhibitors or receptor blockers in post-ICU discharge outcome in patients with acute kidney injury. Intensive Care Med. 2018;44(5):598-605.
Brar S, Ye F, James MT, Hemmelgarn B, Klarenbach S, Pannu N. Association of angiotensin-converting enzyme inhibitors or receptor blocker use with outcomes after acute kidney injury. JAMA Intern Med. 2018;178(12):1681-90.
Harel Z, Wald R, Bargman JM, Mamdani M, Etchells E, Garg AX, et al. Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int. 2013;83(5):901-8.
Thanapongsatorn P, Chaikomon K, Lumlertgul N, Yimsangyad K, Leewongwarasingh, Kulvichit W, et al. Comprehensive versus standard care in post-severe acute kidney injury survivors, a randomized controlled trial. Crit Care. 2021;25(1):322.
Kashani K, Rosner MH, Haase M, Lewington AJP, O’Donoghue DJ, Wilson FP, et al. Quality Improvement Goals for Acute Kidney Injury. Clin J Am Soc Nephrol. 2019;14(6):941-53.
Cowie MR, Fisher M. SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycemic control. Nat Rev Cardiol. 2020;17(12):761-72.
Tahrani AA, Barnett AH, Bailey CJ. SGLT inhibitors in management of diabetes. Lancet Diabetes Endocrinol. 2013;1(2):140-51.
Griffin M, Rao VS, Ivey-Miranda J, Fleming J, Mahoney D, Maulion C, et al. Empagliflozin in heart failure: diuretic and cardiorenal effects. Circulation. 2020;142(11):1028-39.
Hallow KM, Helmlinger G, Greasley PJ, McMurray JJV, Boulton DW. Why do SGLT2 inhibitors reduce heart failure hospitalization? A differential volume regulation hypothesis. Diabetes Obes Metab. 2018;20(3):479-87.
Hiromi K, Jun S, Kazuki T, Tomoko O, Yu T, Hikaru T, et al. Effects of SGLT2 Inhibition on eGFR and Glomerular and Tubular Damage Markers in Japanese Patients with Type 2 Diabetes. J Endocrinol Metab. 2018;8(5):106-12
Foresto-Neto O, Albino AH, Arias SCA, Faustino VD, Zambom FFF, Cenedeze MA, et al. NF-κB system is chronically activated and promotes glomerular injury in experimental type 1 diabetic kidney disease. Front Physiol. 2020;11:84.
Bessho R, Takiyama Y, Takiyama T, Kitsunai H, Takeda Y, Sakagami H, et al. Hypoxia-inducible factor-1α is the therapeutic target of the SGLT2 inhibitors for diabetic nephropathy. Sci Rep. 2019;9(1):14754.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, Cardiovascular Outcomes and Mortality in Type 2 diabetes. N Engl J Med. 2015;373(22):2117-28.
Swedberg K, Young JB, Anand IS, Cheng S, Desai AS, Diaz R, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med. 2013;368(13):1210-9.
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995-2008.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306
Cooper S, Teoh H, Campeau MA, Verma S, Leask RL. Empagliflozin restores the integrity of the endothelial glycocalyx in vitro. Mol Cell Biochem. 2019;459(1-2):121-30.
Herat LY, Magno AL, Rudnicka C, Hricova J, Carnagarin R, Ward NC et al. SGLT2 inhibitor–induced Sympathoinhibition a novel mechanism for cardiorenal protection. JACC Basic Transl Sci. 2020;5(2):169-79.
Zaccardi F, Webb DR, Htike ZZ, Youssef D, Khunti K, Davies MJ. Efficacy and safety of sodium-glucose cotransporter-2 inhibitors in type 2 diabetes mellitus: systematic review and network meta-analysis. Diabetes Obes Metab. 2016;18(8):783-94.
Chilton R, Tikkanen L, Hehnke U, Woerle HJ, Johansen OE. Impact of empagliflozin on blood pressure in dipper and non-dipper patients with type 2 diabetes mellitus and hypertension. Diabetes Obes Metab. 2017;19(11):1620-4.
Matthews V, Elliot R, Rudnicka C, Hricova J, Herat L, Schlaich M. Role of the sympathetic nervous systemin regulation of the sodium glucose co-transporter 2. J Hypertens. 2017;35(10):2059-68.
Baartscheer A, Schumacher CA, Wust RCI, Fioloet JW, Steinen GJM, Coronel R, et al. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia. 2017;60(3):568-73.
Uthman L, Baartscheer A, Bleijlevens B, Schumacher CA, Fiolet JWT, Koeman A, et al. Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na+/H+ exchanger, lowering of cytosolic Na+ and vasodilation. Diabetologia. 2018;61(3):722-6.
Kolhaas M, Liu T, Knopp A, Zeller T, Ong MF, Böhm M, et al. Elevated cytosolic Na+ increase mitochondrial formation of reactive oxygen species in failing cardiac myocytes. Circulation. 2010;121(14):1606-13.
Ojima A, Matsui T, Nishino Y, Nakamura N, Yamagishi S. Empagliflozin, an inhibitor of sodium glucose cotransporter 2 exerts anti-inflammatory and antifibrotic effects on experimental diabetic nephropathy partly by suppressing AGEs-receptor axis. Horm Metab Res. 2015;47(9):686-92.
Kosiborod MN, Esterline RHM, Furtado R, Oscarsson J, Gasparyan SB, Koch GG, et al. Dapagliflozin in patients with cardiometabolic risk factors hospitalized with COVID-19 (DARE-19): a randomized double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2021;9(9):586-94.
Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, Emberson JR, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388(2):117-27.
Gallagher M. Prevention with SGLT2 inhibition of acute kidney injury in intensive care (PREVENTS-AKI). (online). 2023. Source: https://clinicaltrials.gov/ct2/show/NCT05468203 (16th January 2023)