Dialyzer Reuse in the Modern Era
Main Article Content
Abstract
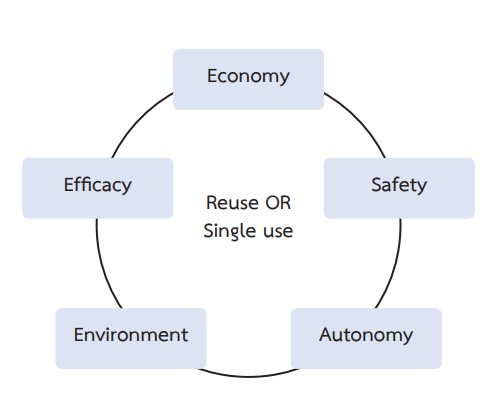
The use of reprocessed dialyzers has been practiced for over 5 decades. In resource-poor countries, dialyzer reuse can help save up to 30% of the cost resulting in more patients gaining access to hemodialysis. Previous studies have confirmed the safety of dialyzer reprocessing if performed under the recommended standard. Patient survival is also comparable with the use of single-use dialyzer. Today modern dialyzers are less costly and provide better biocompatibility and clearance of uremic toxins with less chemical contamination. These factors have made single-use dialyzers increasingly popular. Moreover, the current methods used to determine the efficiency of dialyzer reprocessing are based on studies published 30 years ago which focused only on the clearance of small molecules. Modern hemodialysis and dialyzers are able to provide better clearance of the middle molecules which is associated with better outcomes. The number of studies on the reprocessing of super high flux and middle cut-off dialyzers are also limited. Therefore, there is an urgent need for studies on the reprocessing and reuse of modern dialyzers, especially in the resource-poor countries in order to provide the most effective and economical hemodialysis to the patients.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Twardowski ZJ. Dialyzer reuse-Part I: Historical perspective. Semin Dial. 2006;19(1):41-53.
Finelli L, Miller JT, Tokars JI, Alter MJ, Arduino MJ. National surveillance of dialysis-associated diseases in the United States, 2002. Semin Dial. 2005;18(1):52-61.
Baris E, McGregor M. The reuse of hemodialyzers: an assessment of safety and potential savings. CMAJ. 1993;148(2):175-83.
Qureshi R, Dhrolia MF, Nasir K, Imtiaz S, Ahmad A. Comparison of total direct cost of conventional single use and mechanical reuse of dialyzers in patients of end-stage renal disease on maintenance hemodialysis: A single center study. Saudi J Kidney Dis Transpl. 2016;27(4):774-80.
Upadhyay A, Sosa MA, Jaber BL. Single-use versus reusable dialyzers: the known unknowns. Clin J Am Soc Nephrol. 2007;2(5):1079-86.
Dhrolia MF, Nasir K, Imtiaz S, Ahmad A. Dialyzer reuse: justified cost saving for south Asian region. J Coll Physicians Surg Pak. 2014;24(8):591-6.
Salem M, Ivanovich PT, Ing TS, Daugirdas JT. Adverse effects of dialyzers manifesting during the dialysis session. Nephrol Dial Transplant. 1994;9 Suppl 2:127-37.
Craddock PR, Fehr J, Dalmasso AP, Brighan KL, Jacob HS. Hemodialysis leukopenia. Pulmonary vascular leukostasis resulting from complement activation by dialyzer cellophane membranes. J Clin Invest. 1977;59(5):879-88.
Twardowski ZJ. Dialyzer reuse--part II: advantages and disadvantages. Semin Dial. 2006;19(3):217-26.
Stragier A, Wenderickx D, Jadoul M. Rinsing time and disinfectant release of reused dialyzers: comparison of formaldehyde, hypochlorite, warexin, and renalin. Am J Kidney Dis. 1995;26(3):549-53.
Edens C, Wong J, Lyman M, Rizzo K, Nguyen D, Blain M, et al. Hemodialyzer Reuse and Gram-Negative Bloodstream Infections. Am J Kidney Dis. 2017;69(6):726-33.
Flaherty JP, Garcia-Houchins S, Chudy R, Arnow PM. An outbreak of gram-negative bacteremia traced to contaminated O-rings in reprocessed dialyzers. Ann Intern Med. 1993;119(11):1072-8.
Oyong K, Marquez P, Terashita D, English L, Rivas H, Deak E, et al. Outbreak of bloodstream infections associated with multiuse dialyzers containing O-rings. Infect Control Hosp Epidemiol. 2014;35(1):89-91.
Galvao TF, Silva MT, Araujo ME, Bulbol WS, Cardoso AL. Dialyzer reuse and mortality risk in patients with endstage renal disease: a systematic review. Am J Nephrol. 2012;35(3):249-58.
Owen WF, Jr., Lew NL, Liu Y, Lowrie EG, Lazarus JM. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med. 1993;329(14):1001-6.
Kalantar-Zadeh K, Ficociello LH, Bazzanella J, Mullon C, Anger MS. Slipping Through the Pores: Hypoalbuminemia and Albumin Loss During Hemodialysis. Int J Nephrol Renovasc Dis. 2021;14:11-21.
Cho NJ, Park S, Islam MI, Song HY, Lee EY, Gil HW. Long-term effect of medium cut-off dialyzer on middle uremic toxins and cell-free hemoglobin. PLoS One. 2019;14(7):e0220448.
Thammathiwat T, Tiranathanagul K, Limjariyakul M, Chariyavilaskul P, Takkavatakarn K, Susantitaphong P, et al. Super high-flux hemodialysis provides comparable effectiveness with high-volume postdilution online hemodiafiltration in removing protein-bound and middle-molecule uremic toxins: A prospective cross-over randomized controlled trial. Ther Apher Dial. 2021;25(1):73-81.
Kaplan AA, Halley SE, Lapkin RA, Graeber CW. Dialysate protein losses with bleach processed polysulphone dialyzers. Kidney Int. 1995;47(2):573-8.
Murthy BV, Sundaram S, Jaber BL, Perrella C, Meyer KB, Pereira BJ. Effect of formaldehyde/bleach reprocessing on in vivo performances of high-efficiency cellulose and high-flux polysulfone dialyzers. J Am Soc Nephrol. 1998;9(3):464-72.
Leypoldt JK, Cheung AK, Deeter RB. Effect of hemodialyzer reuse: dissociation between clearances of small and large solutes. Am J Kidney Dis. 1998;32(2):295-301.
Rosner MH, Reis T, Husain-Syed F, Vanholder R, Hutchison C, Stenvinkel P, et al. Classification of Uremic Toxins and Their Role in Kidney Failure. Clin J Am Soc Nephrol. 2021;16(12):1918-28.
Gotch FA. Mass transport in reused dialyzers. Proc Clin Dial Transplant Forum. 1980;10:81-5.
Hemodialysis Adequacy Work G. Clinical practice guidelines for hemodialysis adequacy, update 2006. Am J Kidney Dis. 2006;48 Suppl 1:S2-90.
Ward RA, Ouseph R. Impact of bleach cleaning on the performance of dialyzers with polysulfone membranes processed for reuse using peracetic Acid. Artif Organs. 2003;27(11):1029-34.
Ouseph R, Smith BP, Ward RA. Maintaining blood compartment volume in dialyzers reprocessed with peracetic acid maintains Kt/V but not beta2-microglobulin removal. Am J Kidney Dis. 1997;30(4):501-6.
Tonelli M, Dymond C, Gourishankar S, Jindal KK. Extended reuse of polysulfone hemodialysis membranes using citric acid and heat. ASAIO J. 2004;50(1):98-101.
Piccoli GB, Nazha M, Ferraresi M, Vigotti FN, Pereno A, Barbero S. Eco-dialysis: the financial and ecological costs of dialysis waste products: is a ‘cradle-to-cradle’ model feasible for planet-friendly haemodialysis waste management? Nephrol Dial Transplant. 2015;30(6):1018-27.
Piccoli GB, Cupisti A, Aucella F, Regolisti G, Lomonte C, Ferraresi M, et al. Green nephrology and eco-dialysis: a position statement by the Italian Society of Nephrology. J Nephrol. 2020;33(4):681-98.
Zebrowski P, Zawierucha J, Prystacki T, Marcinkowski W, Malyszko J. Medical waste management - how industry can help us to protect environment and money? Ren Fail. 2020;42(1):547-9.