Drug-Induced Acute Interstitial Nephritis
Main Article Content
Abstract
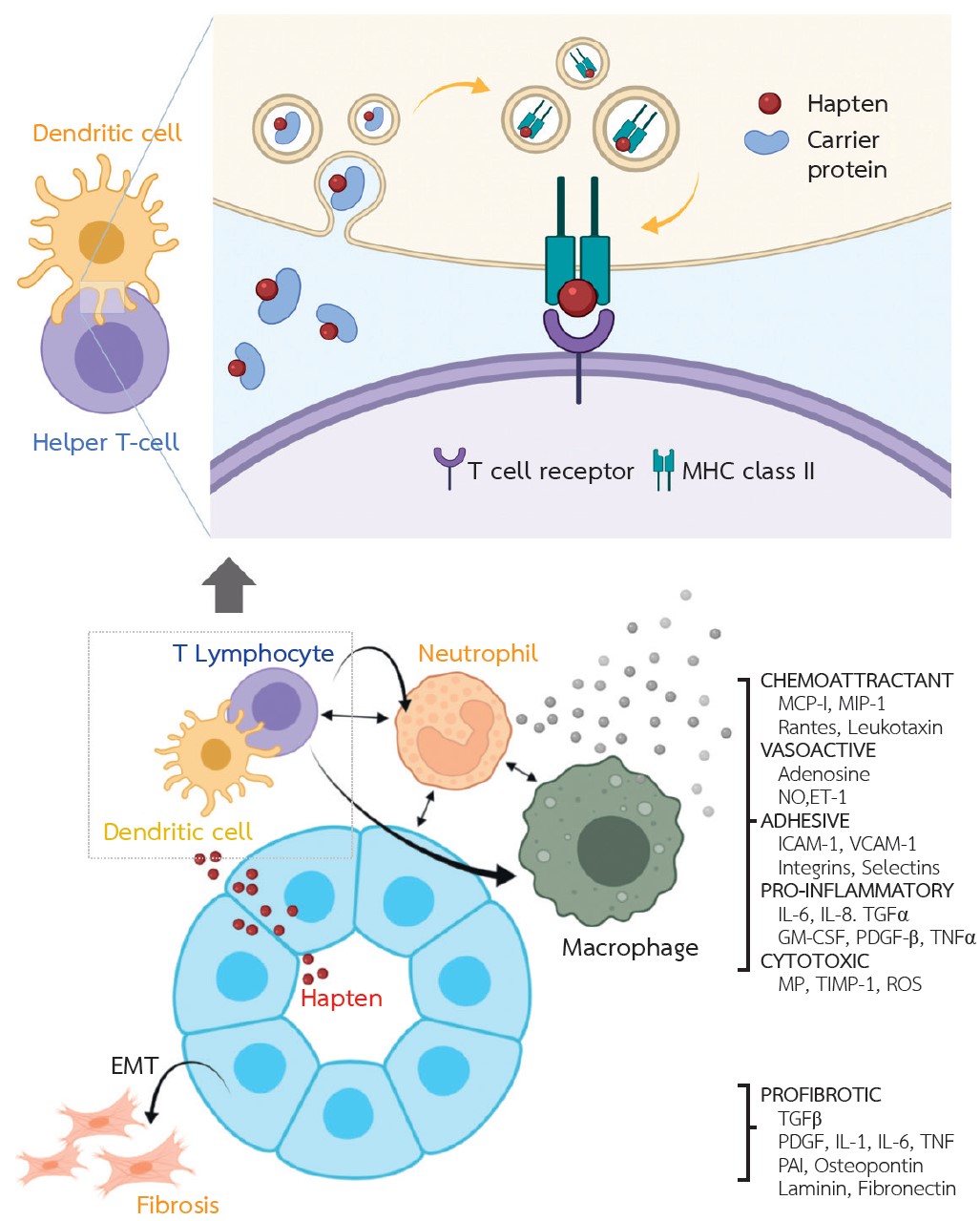
Acute interstitial nephritis (AIN) is an important cause of acute kidney injury. Antibiotics, proton-pump inhibitors, and non-steroidal anti-inflammatory drugs (NSAIDs) are relatively common causes of drug-induced AIN. The pathogenesis of drug-induced AIN involves an allergic response resulting in drug hypersensitivity. The typical triad of symptoms, i.e., rash, fever, and eosinophilia, is only found in 10% of the patients. AIN develops weeks or months after the initiation of the medications. Therefore, drug-induced AIN should be considered in patients with unexplained acute kidney injury and subsequent tissue diagnosis is required. The principles of treatment include the rapid removal of culprit medications and considering for initiation of immunosuppression to reduce chronic kidney disease progression. To date, the efficacy of corticosteroids for treatment of drug-induced AIN has been evaluated in only observational studies. High-dose corticosteroids should be considered in patients with high-probability of
responses including the history of recent uses of the responsible drugs, and mild to moderate interstitial fibrosis from kidney biopsies. Corticosteroids should be discontinued if no meaningful improvement in renal function after 8 weeks because they may potentiate adverse reactions without adding more benefits.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Perazella MA, Rosner MH. Tubulointerstitial diseases. In: YU ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, editors. Brenner & Rector’s the kidney. 11 ed. Philadelphia: Elsevier; 2019. p. 1196-222.
Muriithi AK, Leung N, Valeri AM, Cornell LD, Sethi S, Fidler ME, et al. Biopsy-proven acute interstitial nephritis, 1993-2011: a case series. Am J Kidney Dis 2014;64(4):558-66.
Moledina DG, Perazella MA. Treatment of drug-induced acute tubulointerstitial nephritis: the search for better evidence. Clin J Am Soc Nephrol 2018;13(12):1785-7.
Thong BYH, Tan T-C. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol 2011;71(5):684-700.
Raghavan R, Shawar S. Mechanisms of drug-induced interstitial nephritis. Adv Chronic Kidney Dis 2017;24(2):64-71.
Border WA, Lehman DH, Egan JD, Sass HJ, Glode JE, Wilson CB. Antitubular basement-membrane antibodies in methicillin-associated interstitial nephritis. N Engl J Med 1974;291(8):381-4.
Wuillemin N, Adam J, Fontana S, Krähenbühl S, Pichler WJ, Yerly D. HLA haplotype determines hapten or p-i T cell reactivity to flucloxacillin. J Immunol 2013;190(10): 4956-64.
Ko TM, Chung WH, Wei CY, Shih HY, Chen JK, Lin CH, et al. Shared and restricted T-cell receptor use is crucial for carbamazepine-induced Stevens-Johnson syndrome. J Allergy Clin Immunol 2011;128(6):1266-76.e11.
González E, Gutiérrez E, Galeano C, Chevia C, de Sequera P, Bernis C, et al. Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int 2008;73(8):940-6.
Perazella MA, Markowitz GS. Drug-induced acute interstitial nephritis. Nat Rev Nephrol 2010;6(8):461-70.
Clarkson MR, Giblin L, O’Connell FP, O’Kelly P, Walshe JJ, Conlon P, et al. Acute interstitial nephritis: clinical features and response to corticosteroid therapy. Nephrol Dial Transplant 2004;19(11):2778-83.
Rossert J. Drug-induced acute interstitial nephritis. Kidney Int 2001;60(2):804-17.
Mills RM. Severe hypersensitivity reactions associated with allopurinol. JAMA 1971;216(5):799-802.
Corwin HL, Korbet SM, Schwartz MM. Clinical correlates of eosinophiluria. Arch Intern Med 1985;145(6):1097-9.
Nolan CR, Anger MS, Kelleher SP. Eosinophiluria--a new method of detection and definition of the clinical spectrum. N Engl J Med 1986;315(24):1516-9.
Corwin HL, Bray RA, Haber MH. The detection and interpretation of urinary eosinophils. Arch Pathol Lab Med 1989;113(11):1256-8.
Ruffing KA, Hoppes P, Blend D, Cugino A, Jarjoura D, Whittier FC. Eosinophils in urine revisited. Clin Nephrol 1994; 41(3):163-6.
D’Agati VD, Theise ND, Pirani CL, Knowles DM, Appel GB. Interstitial nephritis related to nonsteroidal anti-inflammatory agents and beta-lactam antibiotics: a comparative study of the interstitial infiltrates using monoclonal antibodies. Mod Pathol 1989;2(4):390-6.
Baker RJ, Pusey CD. The changing profile of acute tubulointerstitial nephritis. Nephrol Dial Transplant 2004;19(1):8-11.
Raza MN, Hadid M, Keen CE, Bingham C, Salmon AH. Acute tubulointerstitial nephritis, treatment with steroid and impact on renal outcomes. Nephrology (Carlton) 2012;17(8): 748-53.
Valluri A, Hetherington L, McQuarrie E, Fleming S, Kipgen D, Geddes CC, et al. Acute tubulointerstitial nephritis in Scotland. QJM 2015;108(7):527-32.
Prendecki M, Tanna A, Salama AD, Tam FW, Cairns T, Taube D, et al. Long-term outcome in biopsy-proven acute interstitial nephritis treated with steroids. Clin Kidney J. 2017; 10(2):233-9.
Fernandez-Juarez G, Perez JV, Caravaca-Fontán F, Quintana L, Shabaka A, Rodriguez E, et al. Duration of treatment with corticosteroids and recovery of kidney function in acute interstitial nephritis. Clin J Am Soc Nephrol 2018;13(12):1851-8.
Preddie DC, Markowitz GS, Radhakrishnan J, Nickolas TL, D’Agati VD, Schwimmer JA, et al. Mycophenolate mofetil for the treatment of interstitial nephritis. Clin J Am Soc Nephrol 2006;1(4):718-22.