The Effect of Sodium-Glucose Co-transporter 2 Inhibitors on Renal Function Among Patients with Diabetic Kidney Disease
Main Article Content
Abstract
Background: Diabetic kidney disease (DKD) is the leading cause of chronic kidney diseases worldwide. Sodium-Glucose Co-Transporter 2 Inhibitors (SGLT2i) is a new class of antidiabetic agent that has renoprotective action beyond glycemic control. However, the efficacy of SGLT2i on renal function in DKD varies in different regions of the world. There has never been any study on the effect of SGLT2i on renal function in Thai population.
Methods: This is a retrospective matched-pair case control study of patients with DKD between 1 January 2015 to 31 December 2020 . Patients who were treated with SGLT2i were matched to those who were not according to age, kidney function, albuminuria and renin-angiotensin-aldosterone system inhibitors (RAASi) usage. The primary outcome was the difference in estimated glomerular filtration rate (eGFR) at 96 weeks. The secondary outcome was the change in eGFR, albuminuria and adverse effects.
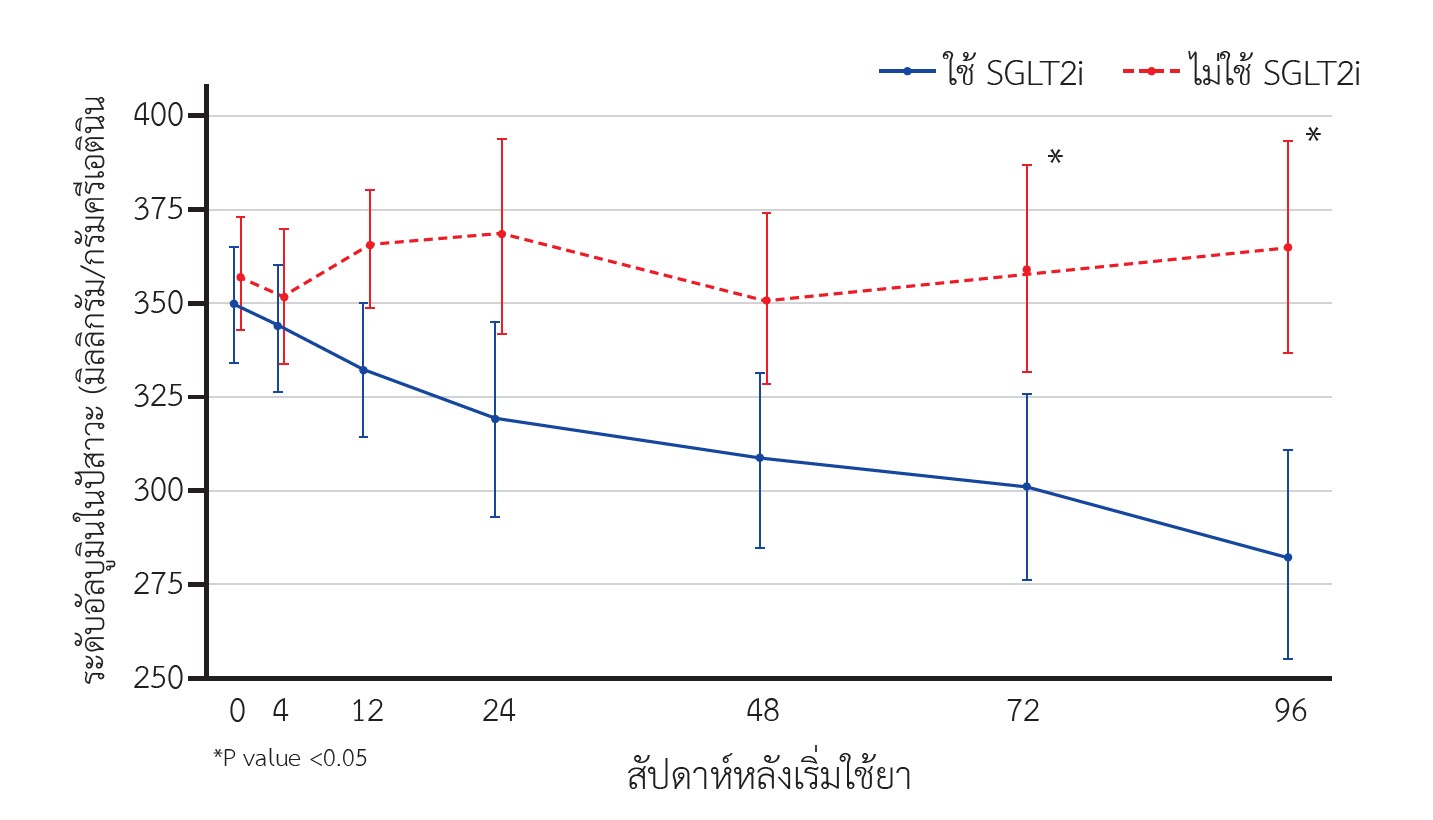
Results: A total of 180 matched pairs were included in the analysis. They were equivalent in age, sex, the number of RAASi usage, baseline eGFR and albuminuria. Estimated glomerular filtration rate at 96 weeks was significantly higher among SGLT2i-users compared to non-users (72.31 vs. 65.37 ml/min/1.73 m2, p = 0.031). The decline in eGFR over 96 weeks was observed in both groups but to a lesser degree among SGLT2i-users (-4.76 vs. -8.46 ml/min/1.73 m2, p = 0.001). Albuminuria at 72 and 96 weeks was also significantly lower among SGLT2i users compared to non-users. Subgroup analysis revealed the higher eGFR among SGLT2i users at 96 weeks was significant only in subgroup of patients with baseline eGFR ≥90 ml/min/1.73 m2. SGLT2i users had higher incidence of urinary tract infection. No serious adverse effects were observed in either group.
Conclusion: The use of SGLT2i was associated with slower decline in eGFR and attenuation of albuminuria among patients with DKD. The use of SGLT2i was associated with increased incidence of urinary tract infection. Serious adverse events were not observed in either group.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, et al. Prevalence and management of diabetes and metabolic risk factors in Thai adults: the Thai National Health Examination Survey IV, 2009: The Thai national health examination survey IV, 2009. Diabetes Care. 2011;34(9):1980–5.
Dall TM, Yang W, Gillespie K, Mocarski M, Byrne E, Cintina I, et al. The economic burden of elevated blood glucose levels in 2017: Diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care. 2019;42(9):1661–8.
Cao Z, Cooper ME. Pathogenesis of diabetic nephropathy: Pathogenesis of diabetic nephropathy. J Diabetes Investig. 2011;2(4):243–7.
Karalliedde J, Gnudi L. Endothelial factors and diabetic nephropathy. Diabetes Care. 2011;34:S291-6.
KDOQI. KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am J Kidney Dis. 2007;49(2 Suppl 2):S12-154.
Molitch ME, Adler AI, Flyvbjerg A, Nelson RG, So W-Y, Wanner C, et al. Diabetic kidney disease: a clinical update from Kidney Disease: Improving Global Outcomes. Kidney Int. 2015;87(1):20–30.
Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR, et al. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63(1):225–32.
Bretzel RG. Prevention and slowing down the progression of the diabetic nephropathy through antihypertensive therapy. J Diabetes Complications. 1997;11(2):112–22.
Parving HH. Diabetic nephropathy: prevention and treatment. Kidney Int. 2001;60(5):2041–55.
Dasgupta I. Cost of treating diabetic kidney disease. Indian J Nephrol. 2014;24(3):139–40.
Strippoli GFM, Bonifati C, Craig M, Navaneethan SD, Craig JC. Angiotensin converting enzyme inhibitors and angiotensin II receptor antagonists for preventing the progression of diabetic kidney disease. Cochrane Database Syst Rev. 2006;(4):CD006257.
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329(20):1456–62.
Deerochanawong C, Kornthong P, Phongwiratchai S, Serirat S. Effects on urinary albumin excretion and renal function changes by delapril and manidipine in normotensive type 2 diabetic patients with microalbuminuria. J Med Assoc Thai. 2001;84(2):234–41.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Novikov A, Vallon V. Sodium glucose cotransporter 2 inhibition in the diabetic kidney: an update: An update. CurrOpin Nephrol Hypertens. 2016;25(1):50–8.
Schork A, Saynisch J, Vosseler A, Jaghutriz BA, Heyne N, Peter A, et al. Effect of SGLT2 inhibitors on body composition, fluid status and renin-angiotensin-aldosterone system in type 2 diabetes: a prospective study using bioimpedance spectroscopy. Cardiovasc Diabetol. 2019;18(1):46.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Zhang X-L, Zhu Q-Q, Chen Y-H, Li X-L, Chen F, Huang J-A, et al. Cardiovascular safety, long-term noncardiovascular safety, and efficacy of sodium-glucose cotransporter 2 inhibitors in patients with type 2 diabetes mellitus: A systemic review and meta-analysis with trial sequential analysis. J Am Heart Assoc. 2018;7(2).
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Perkovic V, Jardine M, Vijapurkar U, Meininger G. Renal effects of canagliflozin in type 2 diabetes mellitus. Curr Med Res Opin. 2015;31(12):2219–31.
Hsia DS, Grove O, Cefalu WT. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. CurrOpin Endocrinol Diabetes Obes. 2017;24(1):73–9.
Khouri C, Cracowski J-L, Roustit M. SGLT-2 inhibitors and the risk of lower-limb amputation: Is this a class effect? Diabetes ObesMetab. 2018;20(6):1531–4.
Bersoff-Matcha SJ, Chamberlain C, Cao C, Kortepeter C, Chong WH. Fournier gangrene associated with sodium-glucose cotransporter-2 inhibitors: A review of spontaneous postmarketing cases. Ann Intern Med. 2019;170(11):764–9.
Heerspink HJL, Karasik A, Thuresson M, Melzer-Cohen C, Chodick G, Khunti K, et al. Kidney outcomes associated with use of SGLT2 inhibitors in real-world clinical practice (CVD-REAL 3): a multinational observational cohort study. Lancet Diabetes Endocrinol. 2020;8(1):27–35.
Kohan DE, Fioretto P, Tang W, List JF. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int. 2014;85(4):962–71.
Cherney DZI, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
Rossing P, Caramori ML, Chan JCN, Heerspink HJL, Hurst C, Khunti K, et al. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022;102(5):S1–127.