Long Term Renal Outcome in Preeclampsia: Role of sFlt-1 / PlGF and Endoglin
Main Article Content
Abstract
Background: Preeclampsia (PE) is an important complication of pregnancy and can lead to chronic kidney disease by causing endothelial damage and podocyte loss, Soluble forms-like tyrosine kinase-1 (sFlt-1), placental growth factor (PlGF), sFlt1/PlGF ratio and endoglin are the biomarkers for the differential diagnosis of preeclampsia and other diseases. We aim to explore the correlation of these biomarkers with long term renal function, blood pressure and urine albumin creatinine ratio (UACR) in PE patients.
Methods: All patients diagnosed as PE were enrolled. Blood samples for sFlt-1, PlGF, endoglin and urine albumin-creatinine ratio (UACR) were collected. After delivery, the patients were followed to record blood pressure, renal function and UACR at three months and one year.
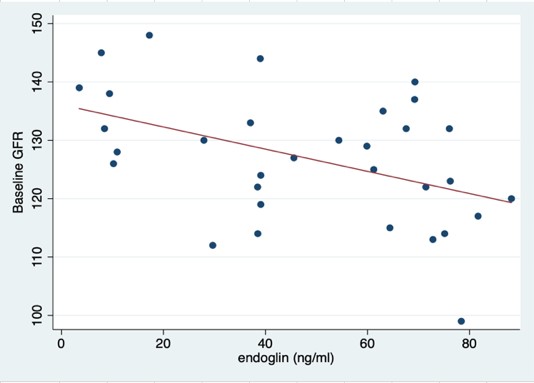
Results: 42 PE patients were included. Estimated glomerular filtration rate (eGFR) decreased significantly within three months and one year after follow-up (128.20 ± 10.34 to 120.75 ± 10.166 mL/min/1.73 m2 (p=0.001) at three months and 126.71 ± 9.948 to 114.29 ± 11.274 mL/min/1.73 m2 (p < 0.001) at one year. The endoglin level correlated significantly with eGFR level during PE but there was no correlation of all the biomarkers with eGFR, blood pressure, urine albumin-creatinine ratio (UACR) at one year.
Conclusion: PE carries an increased risk for the mother to develop renal disease later in life. Only endoglin can help diagnose PE but is not correlated with long term renal function, blood pressure and urine albumin creatinine ratio (UACR).
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Rudra CB, Williams MA. Monthly variation in preeclampsia prevalence: Washington State, 1987-2001, J Matern Fetal Neonatal Med. 2005;18(5):319-24.
Bellamy L, Casas JP, Hingorani AD, Williams DJ. Preeclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. Br Med J. 2007;335(7627):974-7.
Magee LA, von Dadelszen P. Pre-eclampsia and increased cardiovascular risk. Br Med J. 2007 335(7627):945–6.
Airoldi J, Weinstein L. Clinical significance of proteinuria in pregnancy. Obstet Gynecol Surv. 2007;62(2) 117-24.
Drakeley AJ, Le Roux PA, Anthony J, Penny J. Acute renal failure complicating severe preeclampsia requiring admission to an obstetric intensive care unit. Am J Obstet Gynecol. 2002;186(2):253-6.
McDonald SD, Han Z, Walsh MW, Gerstein HC, Devereaux PJ. Kidney disease after preeclampsia: a systematic review and meta-analysis. Am J Kidney Dis. 2010;55(6):1026-39.
Fiaschi E, Naccarato R. The histopathology of the kidney in toxaemia. Serial renal biopsies during pregnancy, puerperium and several years postpartum. Light and electron microscopic and immunofluorescent studies. Virchows Archiv A Pathol Anat. 1968;345(4):299-309.
Murakami S, Saitoh M, Kubo T, Koyama T, Kobayashi M. Renal disease in women with severe preeclampsia or gestational proteinuria. Obstet Gynecol. 2000;96(6):945-9.
National Collaborating Centre for Chronic Conditions. Royal College of Physicians; London: 2008. Chronic Kidney Disease: National Clinical Guideline for Early Identification and Management in Adults in Primary and Secondary Care.
Ayansina D, Black C, Hall SJ, Marks A, Miller C, Prescott GJ, et al. Long term effects of gestational hypertension and pre-eclampsia on kidney function: Record linkage study. Pregnancy Hypertens. 2016;6:344-9.
van Balen VAL, Spaan JJ, Cornelis T, Spaanderman MEA. Prevalence of chronic kidney disease after preeclampsia. J Nephrol. 2017;30(3):403-9.
Pollak VE, Nettles JB. The kidney in toxemia of pregnancy: a clinical and pathologic study based on renal biopsies. Medicine (Baltimore). 1960;39:469-526.
Ballermann BJ. Glomerular endothelial cell differentiation. Kidney Int 2005; 67: 1668-71.
Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003;111(5):707-16.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111(5): 649-58.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672-83.
Roberts WG, Palade GE. Increased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factor. J Cell Sci. 1995;1082369-79.
Kaleta T, Stock A, Panayotopoulos D, Vonend O, Niederacher D, Neumann M, et al. Predictors of Impaired Postpartum Renal Function in Women after Preeclampsia: Results of a Prospective Singer Center Study. Dis Markers. 2016;2016:7861919.
Hirashima C, Ohkuchi A, Arai F, Takahashi K, Suzuki H, Watanabe T, et al. Establishing reference values for both total soluble Fms-like tyrosine kinase 1 and free placental growth factor in pregnant women. Hypertens Res. 2005;28(9):727-32.
Cheifetz S, Bellon T, Cales C, Vera S, Bernabeu C, Massague J, et al. Endoglin is a component of the transforming growth factor-beta receptor system in human endothelial cells. J Biol Chem. 1992;267(27): 9027-30.
.Gougos A, St Jacques S, Greaves A, O’Connell PJ, d’Apice AJ, Buhring HJ, et al. Identification of distinct epitopes of endoglin, an RGD-containing glycoprotein of endothelial cells, leukemic cells, and syncytiotrophoblasts. Int Immunol. 1992;4(1):83-92.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al.Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355(10):992-1005.
Elhawary TM, El-Bendary AS, Demerdash H. Maternal serum endoglin as an early marker of pre-eclampsia in high-risk patients. Int J Womens Health. 2012;4:521-5.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672-83.
Nachtigal P, Vecerova LZ, Rathouska J, Strasky Z. The role of endoglin in atherosclerosis. Atherosclerosis. 2012;224(1): 4-11.