EFFECTS OF THE INTEGRATED SMOKING CESSATION SERVICE SYSTEM IN PRIMARY HEALTHCARE SERVICE ON SMOKING STATUS
Keywords:
integration, smoking cessation, primary health servicesAbstract
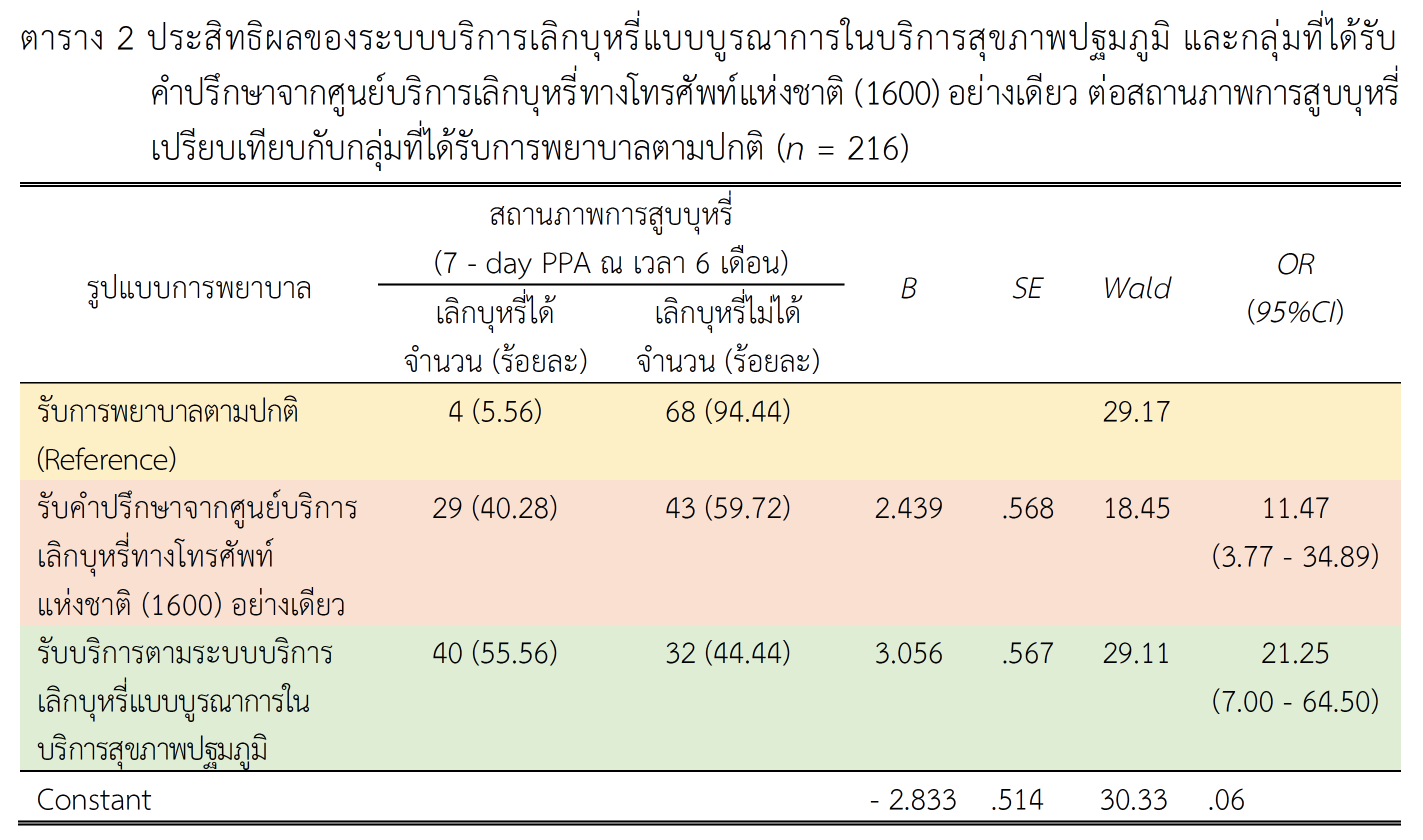
This quasi - experimental research aimed 1) to compare the smoking status of smokers after receiving services from the integrated smoking cessation program in primary healthcare services with a group that receives standard nursing care, and 2) to compare the smoking status of smokers after receiving counseling from the national telephone smoking cessation service with a group that receives standard nursing care. The sample of the study consisted of smokers aged 18 to 75 who smoked either cigarettes or roll-your-own cigarettes in Nakhon Pathom province. Participants were stratified into three groups, each comprising 72 individuals: 1) those receiving the integrated smoking cessation service system in primary health services, 2) those undergoing counseling from the Thailand National Quitline (TNQ) counselor, and 3) those receiving standard nursing care. Matching was performed based on age and nicotine addiction levels. The research utilized the Integrated Smoking Cessation Service System in Primary Health Services as the experimental tool, and data collection involved a questionnaire assessing smoking cessation prevalence at the 6-month mark. Descriptive statistics and bivariate logistic regression analysis were employed for data analysis.
The research revealed successful smoking cessation rates as follows: 55.56% for the group receiving the integrated smoking cessation service system, 40.28% for the TNQ counseling group, and 5.56% for the standard nursing care group. Comparing the smoking status of each group, individuals in the integrated smoking cessation service system group exhibited a 21.25 times higher likelihood of successful quitting compared to those receiving usual care (OR = 21.25, 95%CI = 7.00 - 64.50). Similarly, the group receiving counseling only from the TNQ had an 11.47 times higher chance of successful quitting compared to the standard nursing care group (OR = 11.47, 95%CI = 3.77 - 34.89). Therefore, the implementation of an integrated smoking cessation service system in primary healthcare facilities is recommended to enhance smoking cessation efforts in the community.
Downloads
References
Bright, T., & Burdett, T. (2019). Smoking cessation and the health promotion role of community nurses. The Journal of Community Nursing, 33, 56-60.
Bureau of Tobacco Control Department of Disease Control. (2022). The third national strategic plan for tobacco control. Nonthaburi: Ministry of Public Health.
Cahill, K., Lancaster, T., & Green, N. (2010). Stage-based interventions for smoking cessation. Cochrane Database of Systematic Reviews, 11.
Chu, S., Feng, L., Zuo, Y., Jing, H., Zhang, D., Tong, Z., . . . Liang, L. (2023). Evaluation of an innovative mHealth-based integrated modality for smoking cessation in Chinese smokers: Protocol for a randomized controlled trial. BMC Public Health, 23(1), 1-13.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd). New York, NY: Routledge.
Cope, G. F. (2023). Managing smoking cessation in primary care. Journal of Prescribing Practice, 5(4), 152-156.
Delle, S., Kraus, L., Maspero, S., Pogarell, O., Hoch, E., & Lochbühler, K. (2022). Effectiveness of the national German Quitline for smoking cessation: Study protocol of a randomized controlled trial. BMC Public Health, 22(1), 1-9.
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W., & Robinson, J. (1989). Measuring the Heaviness of Smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction, 84(7), 791-799.
McLeroy, K. R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351-377.
National Statistical Office. (2021). The 2021 health behavior of population survey. Bangkok: Pimdeekarnpim.
Papadakis, S., Pipe, A. L., Reid, R. D., Tulloch, H., Mullen, K. - A., Assi, R., . . . Wells, G. (2015). Effectiveness of performance coaching for enhancing rates of smoking cessation treatment delivery by primary care providers: Study protocol for a cluster randomized controlled trial. Contemporary Clinical Trials, 45(Part B), 184-190.
Park, E. R., Gareen, I. F., Japuntich, S., Lennes, I., Hyland, K., DeMello, S., . . . Rigotti, N. A. (2015). Primary care provider-delivered smoking cessation interventions and smoking cessation among participants in the national lung screening trial. JAMA Internal Medicine, 175(9), 1509-1516.
Piñeiro, B., Wetter, D. W., Vidrine, D. J., Hoover, D. S., Frank - Pearce, S. G., Nguyen, N., . . . Vidrine, J. I. (2019). Quitline treatment dose predicts cessation outcomes among safety net patients linked with treatment via ask-advise-connect. Preventive Medicine Reports, 13, 262-267.
Piper, M. E., Cook, J. W., Schlam, T. R., Jorenby, D. E., Smith, S. S., Collins, L. M., . . . Baker, T. B. (2018). A randomized controlled trial of an optimized smoking treatment delivered in primary care. Annals of Behavioral Medicine, 52(10), 854-864.
Prochaska, J., & Diclemente, C. (1983). Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390-395.
Prochaska, J. O., & DiClemente, C. C. (1982). Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, research & practice, 19(3), 276.
Prochaska, J. O., Norcross, J. C., & DiClemente, C. C. (2013). Applying the stages of change. Psychotherapy in Australia, 19(2), 10-15.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38-48.
Scheffers-van Schayck, T. S., Otten, R., Engels, R. C., & Kleinjan, M. (2019). Proactive telephone smoking cessation counseling tailored to parents: Results of a randomized controlled effectiveness trial. International Journal of Environmental Research and Public Health, 16(15), 2730.
Siewchaisakul, P., Luh, D-L., Chiu, S. Y., Yen, A. M., Chen, C-D., & Chen, H-H. (2020). Smoking cessation advice from healthcare professionals helps those in the contemplation and preparation stage: An application with transtheoretical model underpinning in a community-based program. Tobacco Induced Diseases, 18.
Thanomsat, K., & Yunibhand, J. (2019). Effective behavioral interventions for smoking cessation in the primary care setting: A meta-analysis. Interdisciplinary Research, 14(6), 1-6.
Thanomsat, K., Yunibhand, J., & Preechawong, S. (2022). An integrated smoking cessation intervention in the primary care service system: An intervention mapping. The Open Public Health Journal, 15(1).
Tobacco Control Research and Knowledge Management Center. (2017). Assessment of the framework convention on tobacco control: Implementation Thailand, 2016. Bangkok: Jareonkarnmunkong.
Torre, G. L. (2015). Smoking prevention and cessation. New York, NY: Springer.
Úbeda, J. F. S-V., Rodríguez-Vázquez, S., Barranco, J. A. O., Caldera, G. V., Alvárez, P. P. P., Buitrago, F., . . . Pérez Alvárez, P. P. (2019). Effectiveness of individual and group multicomponent interventions for smoking cessation in primary care: A quasi-experimental study. Family practice, 36(5), 627-633.
Velicer, W. F., Prochaska, J. O., Rossi, J. S., & Snow, M. G. (1992). Assessing outcome in smoking cessation studies. Psychological bulletin, 111(1), 23.
World Health Organization (WHO). (2022). Tobacco. Geneva: WHO.
World Health Organization (WHO). (2010). WHO guidelines for implementation of article 14 of the WHO framework convention on tobacco control. Geneva: WHO.
Yunibhand, J. (2015). Smoking cessation booklet, life without smoking, and preparation for new life. Bangkok: Pre-One.
Zhou, S., Levinson, A. H., Zhang, X., Portz, J. D., Moore, S. L., Gore, M. O., Ford, K. L., Li, Q., & Bull, S. (2021). A pilot study and ecological model of smoking cues to inform mobile health strategies for quitting among low-income smokers. Health Promotion Practice, 22(6), 850-862.
Zhou, X., Nonnemaker, J., Sherrill, B., Gilsenan, A. W., Coste, F., & West, R. (2009). Attempts to quit smoking and relapse: Factors associated with success or failure from the ATTEMPT cohort study. Addictive Behaviors, 34(4), 365-373.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 JOURNAL OF THE POLICE NURSES

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ