ปัจจัยคัดสรรที่มีความสัมพันธ์กับระยะเวลามารับการรักษาของผู้สูงอายุที่มีภาวะพิษเหตุติดเชื้อ
คำสำคัญ:
ระยะเวลามารับการรักษา, ผู้สูงอายุ, พิษเหตุติดเชื้อบทคัดย่อ
การวิจัยความสัมพันธ์นี้มีวัตถุประสงค์เพื่อศึกษาปัจจัยที่มีความสัมพันธ์กับระยะเวลามารับการรักษาของผู้สูงอายุที่มีภาวะพิษเหตุติดเชื้อ ที่เข้ารับการรักษาในหอผู้ป่วยอายุรกรรมของโรงพยาบาลระดับตติยภูมิ 2 แห่ง เขตกรุงเทพมหานคร ระหว่างเดือนกรกฎาคมถึงเดือนตุลาคม พ.ศ. 2564 คัดเลือกตัวอย่างแบบเฉพาะเจาะจง จำนวน 87 ราย เครื่องมือที่ใช้ในการวิจัย ประกอบด้วย แบบสอบถามความรู้สึกหลากหลายมิติเกี่ยวกับความช่วยเหลือ
ทางสังคม แบบสอบถามการรับรู้ความเจ็บป่วย และแบบวัดความรู้เกี่ยวกับภาวะติดเชื้อในกระแสเลือด ผ่านการตรวจสอบความตรงเชิงเนื้อโดยผู้ทรงคุณวุฒิ 5 ท่าน มีค่าความเที่ยงเท่ากับ .828, .827, และ .718 ตามลำดับ วิเคราะห์ข้อมูลโดยใช้สถิติเชิงพรรณา สัมประสิทธิ์สหสัมพันธ์พอยท์ไบซีเรียล และสัมประสิทธิ์สหสัมพันธ์สเปียร์แมน
ผลการวิจัย พบว่า ผู้สูงอายุที่มีภาวะพิษเหตุติดเชื้อมีค่ามัธยฐานระยะเวลามารับการรักษาเท่ากับ 62.20 ชั่วโมง (IQR= 62.5) ผลการวิเคราะห์ความสัมพันธ์ พบว่า ปัจจัยความรู้เกี่ยวกับภาวะพิษเหตุติดเชื้อ การรับรู้ด้านลักษณะของความเจ็บป่วย การตอบสนองต่อความเจ็บป่วยด้านอารมณ์ การสนับสนุนทางสังคม และประสบการณ์เกี่ยวกับภาวะพิษเหตุติดเชื้อมีความสัมพันธ์กับระยะเวลามารับการรักษาอย่างมีนัยสำคัญทางสถิติที่ระดับ .05 (rs= -.446, rs= -.371, rs= -.342, rs= -.276, และ rpb= -.239 ตามลำดับ) ดังนั้น พยาบาลและทีมสุขภาพควรตระหนักถึงการให้ความรู้และส่งเสริมการรับรู้เกี่ยวกับภาวะพิษเหตุติดเชื้อที่ถูกต้อง โดยเฉพาะด้านลักษณะอาการแก่ผู้ป่วยและครอบครัว ตลอดจนส่งเสริมการจัดการอารมณ์ขณะเผชิญกับอาการอย่างเหมาะสม เพื่อช่วยให้ผู้สูงอายุที่มีภาวะพิษเหตุติดเชื้อมารับการรักษารวดเร็วยิ่งขึ้น
Downloads
เอกสารอ้างอิง
Borson, S., Scanlan, J., Brush, M., Vitaliano, P., & Dokmak, A. (2000). The Mini-Cog: A cognitive vital signs measure for dementia screening in multi-lingual elderly. International Journal of Geriatric Psychiatry, 15(11), 1021-1027.
Broadbent, E., Petrie, K. J., Main, J., & Weinman, J. (2006). The brief illness perception questionnaire. Journal of Psychosomatic Research, 60(6), 631-637.
Bunyaphatkun, P. (2015). The effectiveness of emergency health care system on clinical signs in patients with sepsis (Doctor degree of philosophy, nursing). Faculty of Graduate Studies, Mahidol University, Bangkok.
Chattaris, T., & Muangpaisan, W. (2018). Cognitive change in normal aging. In W. Muangpaisan (Ed.), Challenges and solutions for healthy aging (pp. 291-323). Bangkok: Thai Society of Gerontology and Geriatric Medicine.
Cheranakhon, C. (2018). Rapid detection of sepsis. In D. Staworn, K. Piyavechviratana, & S. Poonyathawon (Eds.), ICU everywhere (pp. 115-127). Bangkok: The Thai Society of Critical Care Medicine.
Doungsuriya, P., Chanruangvanich, W., Chayaput, P., & Thosingha, O. (2021). Factors predicting severity of physiological deterioration among sepsis patients in emergency department. Journal of Thailand Nursing and Midwifery Council, 36(3), 134-150.
Eitze, S., Fleischmann-Struzek, C., Betsch, C., & Reinhart, K., & the vaccination60+study group (2018). Determinants of sepsis knowledge: A representative survey of the elderly population in Germany. Critical Care, 22(1), 273-273.
Falaha, T., Worku, A., Meskele, M., & Facha, W. (2016). Health care seeking behaviour of elderly people in rural part of Wolaita zone, Southern Ethiopia. Health Science Journal, 10(4), 12-17.
Hancock, R. D. (2018). Qualitative analysis of older adult’ experiences with sepsis (Doctor degree of philosophy, nursing). The School of Nursing, Indiana University.
Health Data Center, Ministry of Public Health. (2021). Mortality rate in severe community-acquired sepsis patients. Retrieved from https://hdcservice.moph.go.th/hdc/reports/report_kpi.php?flag_kpi_level=1&flag_kpi_year=2021&source=pformated/format1.php&id=00366a85bd3c2b6932a228df29137252#
Hwang, S. Y., & Jeong, M. H. (2012). Cognitive factors that influence delayed decision to seek treatment among older patients with acute myocardial infarction in Korea. European Journal of Cardiovascular Nursing, 11(2), 154-159.
Kang, H. (2021). Sample size determination and power analysis using the G*Power software. Journal of Educational Evaluation for Health Professions, 18, 17-28. http://dx.doi.org/10.3352/jeehp.2021.18.17
Leventhal, H., Brissette, I., & Leventhal, E. A. (2003). The common-sense model of self-regulation of health and illness. In L. D. Cameron & H. Leventhal (Eds.), The self-regulation of health and illness behaviour (pp. 42-65). New York, NY: Routledge.
Liang, S. Y. (2016). Sepsis and other infectious disease emergencies in the elderly. Emergency Medicine Clinics of North America, 34(3), 501-522.
Liu, V. X., Fielding-Singh, V., Greene, J. D., Baker, J. M., Iwashyna, T. J., Bhattacharya, J., . . . Escobar, G. J. (2017). The timing of early antibiotics and hospital mortality in sepsis. American Journal of Respiratory and Critical Care Medicine, 196(7), 856-863.
Makam, R. P., Erskine, N., Yarzebski, J., Lessard, D., Lau, J., Allison, J., . . . Goldberg, R. J. (2016). Decade long trends (2001-2011) in duration of pre-hospital delay among elderly patients hospitalized for an acute myocardial infarction. Journal of the American Heart Association, 5(4), e002664.
National Statistical Office of Thailand. (2021). Statistic yearbook Thailand 2021. Retrieved from https://shorturl.asia/tk3TX
Otto, G. P., Sossdorf, M., Claus, R. A., Rödel, J., Menge, K., Reinhart, K., . . . Riedemann, N. C. (2011). The late phase of sepsis is characterized by an increased microbiological burden and death rate. Critical Care, 15(4), R183.
Permpikul, C. (2018). Sepsis and septic shock. Bangkok: Beyond Enterprise.
Pinphat, S., Puwarawuttipanit, W., Sriprasong, S., & Rongrungruang, Y. (2022). Factors influencing time-to-hospital decision in patients with sepsis. Nursing Science Journal of Thailand, 40(1), 99-111.
Polit, D. F., & Beck, C. T. (2018). Essentials of nursing research: Appraising evidence for nursing practice (9th ed.). Philadelphia, PA: Wolters Kluwer.
Pornsirirat, T. (2015). Nursing care for septic shock patients. In S. Naowapanich & W. Pinyopasakul (Eds.), Critical care: Medical nursing (pp. 291-323). Faculty of Medicine Siriraj Hospital, Mahidol University.
Prescott, H. C., & Angus, D. C. (2018). Enhancing recovery from sepsis: A review. Journal of the American Medical Association, 319(1), 62-75.
Rudd, K. E., Johnson, S. C., Agesa, K. M., Shackelford, K. A., Tsoi, D., Kievlan, D. R., . . . Naghavi, M. (2020). Global, regional, and national sepsis incidence and mortality, 1990-2017: Analysis for the global burden of disease study. The Lancet, 395(10219), 200-211.
Samoraphop, B., Channarong, P., & Lach, H. W. (2020). Factors related to a delay in seeking treatment for acute myocardial infarction in older adults: An integrative review. Pacific Rim International Journal of Nursing Research, 24(4), 553-568.
Sasat, S. (2021). Gerontological nursing: Common problems and caring guideline (5th ed.). Chulalongkorn University Printing House.
Seymour, C. W., Kahn, J., Martin-Gill, C., Callaway, C. W., Yealy, D. M., Scales, D., . . . Angus, D. C. (2017). Delays from first medical contact to antibiotic administration for sepsis. Critical Care Medicine, 45(5), 759-765.
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., . . . Angus, D. C. (2016). The third international consensus definitions for sepsis and septic shock (Sepsis-3). Journal of the American Medical Association, 315(8), 801-810.
Sri-on, J. (2017). Geriatric emergency medicine. In J. Sri-on, R. Rojsaengruang, & C. Sawawiboon (Eds.), Geriatric emergency (pp. 3-16). Bangkok: Faculty of Medicine Vajira Hospital, Navamindradhiraj University.
Strategy and Planning Division, Ministry of Public Health. (2019). Public health statistics A.D.2019. Retrieved from https://bps.moph.go.th/new_bps/node/232
Tanner, D. (2012). The examination of factors that Influence treatment seeking delay among older adults diagnosed with acute myocardial infarction (Doctor degree of philosophy, nursing). Byrdine F. Lewis School of Nursing and Health Professions, Georgia State University, Georgia, Atlanta.
Thepphawan, P. (2010). Cognitive representation, emotional responses and hospitalization experience in predicting decision making for receiving treatment among patients with acute coronary syndrome (Master degree of nursing science, adult nursing). Faculty of Nursing, Mahidol University, Bangkok.
Thongcharoen, V. (2015). Science and art of gerontological nursing (2nd ed.). Bangkok: Faculty of nursing, Mahidol University.
Trongsakul, S., Lambert, R., Clark, A., Wongpakaran, N., & Cross, J. (2015). Development of the Thai version of Mini-Cog, a brief cognitive screening test. Geriatrics and Gerontology International, 15(5), 594-600.
Wongpakaran, N., & Wongpakaran, T. (2012). A revised Thai multi-dimensional scale of perceived social support. The Spanish Journal of Psychology, 15(3), 1503-1509.
Wongpakaran, T., Wongpakaran, N., & Ruktrakul, R. (2011). Reliability and validity of the multidimensional scale of perceived social support (MSPSS): Thai version. Clinical Practice & Epidemiology in Mental Health, 7, 161-166.
Yanagida, T., Fujimoto, S., Inoue, T., & Suzuki, S. (2014). Causes of prehospital delay in stroke patients in an urban aging society. Journal of Clinical Gerontology and Geriatrics, 5(3), 77-81.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30-41.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
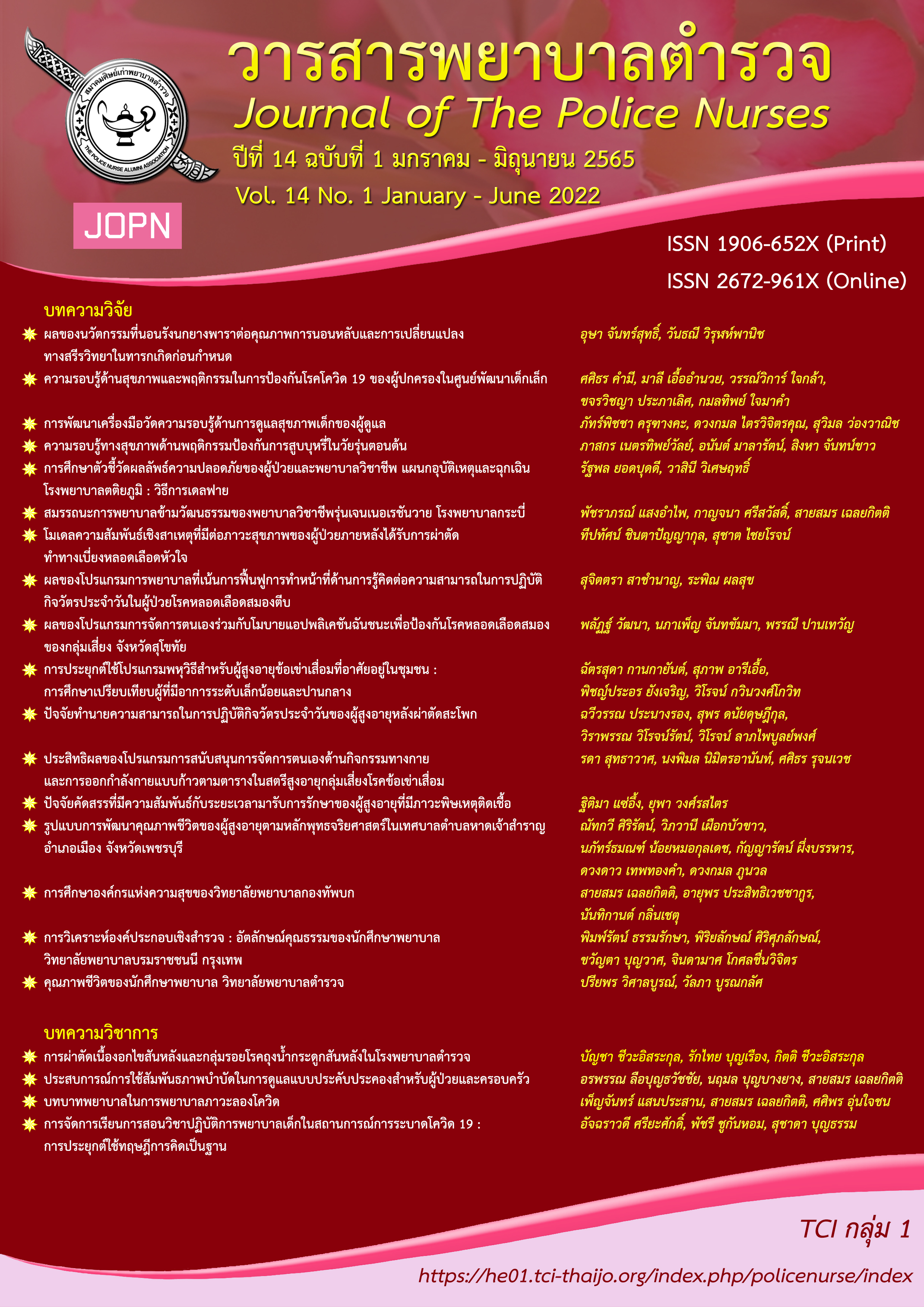
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2022 วารสารพยาบาลตำรวจ

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ