PROMOTING HEALTH-RELATED QUALITY OF LIFE IN PATIENTS WITH METASTATIC COLORECTAL CANCER
Keywords:
health-related quality of life, colorectal cancerAbstract
Promoting health-related quality of life for patients with metastatic colorectal cancer is important. The objective of this article to present the way of promoting quality of life relate health, it is consisted of 4 domains which are 1) physical health, 2) mental and emotional health, 3) family and social, and 4) physical activities. The health care provider team has participated in promoting the quality of life, monitoring, following, evaluating the treatment, and managing the effective disease progression. The symptoms associated with metastatic colorectal cancer, both from the disease and side effects or complications from treatment, include abnormalities of the gastrointestinal tract, pain, and fatigue that affected on the nutritional status, mental health, and activities of the patients.
Downloads
References
Aminisani, N., Fatemi, M., Sarbakhsh, P., Nikanfar, A., Eftekharsadat, A., & Jafari, E. (2017). Health-related quality of life and its correlates among rectal cancer survivors, Northwest of Iran. Journal of Cancer Metastasis and Treatment, 3, 209-216. doi:10.20517/2394-4722.2017.47
Atthaphinan, C., & Lueboonthavatchai, P. (2017). Quality of life and associated factors in colorectal cancer patients with colostomy at King Chulalongkorn Memorial Hospital. Chulalongkorn Medical Journal, 61(3), 387-400.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer Journal for Clinicians, 68(6), 394-424.
Chaichompoo, R., Namvongprom, A., Pakdevong, N., Preechakoon, B., & Ounlam, T. (2019). Relationship between symptom severity and distress in patients with advanced cancer. Journal of Nursing and Health Sciences, 13(4), 1-13.
Chinda, M., Jaturapatporn, D., Kirshen, A. J., & Udomsubpayakul, U. (2011). Reliability and validity of a Thai version of the Edmonton Symptom Assessment Scale (ESAS-Thai). Journal of Pain and Symptom Management, 42(6), 954-960. doi:10.1016/j.jpainsymman.2011.02.020
Chiorean, E. G., Nandakumar, G., Fadelu, T., Temin, S., Alarcon-Rozas, A. E., Bejarano, S. &, Chamberlin, M. D. (2020). Treatment of patients with late-stage colorectal cancer: ASCO resource-stratified guideline. JCO Global Oncology, 6, 414-438. doi:10.1200/JGO.19.00367
Decha, W., & Navicharern, R. (2016). Predicting factors of quality of life among colorectal cancer patients with colostomy receiving chemotherapy. Kuakarun Journal of Nursing, 23(1), 133-147.
Esin, E., & Yalcin, S. (2016). Maintenance strategy in metastatic colorectal cancer: A systematic review. Cancer Treatment Reviews, 42, 82-90. doi:10.1016/j.ctrv.2015.10.012
Feo, L., Polcino, M., & Nash, G. M. (2017). Resection of the primary tumor in stage IV colorectal cancer: when is it necessary? The Surgical clinics of North America, 97(3), 657-669. doi:10.1016/j.suc.2017.01.012
Kaewrat, P., Chaiaroon, W., & Wisestrith, W. (2017). Life experiences of ongoing chemotherapy for colorectal cancer patients. EAU Heritage Journal Science and Technology, 11(1), 224-234.
Kimura, C. A., Kamada, I., de Jesus C. A. C., & Guilhem, D. (2014). Quality of life of colorectal cancer patients with intestinal stomas. Journal of Carcinogenesis & Mutagenesis, S10, 007. doi:10.4172/2157-2518.S10-007
Imsamran, W., Pattatang, A., Supattagorn, P., Chiawiriyabunya, I., Namthaisong, K., Wongsena, M., . . . Buasom, R. (2018). Cancer in Thailand Vol. IX, 2013-2015. Bangkok: National Cancer Institute, Thailand.
McMullen, C., Liu, L., Bulkley, J.E., Hornbrook, M.C., Wendel, C., Grant, M., . . . Herrinton, L., (2016). Participation in activities associated with quality of life for long-term survivors of rectal cancer. The Permanente Journal, 21, 48-54. https://doi.org/10.7812/TPP/16-011
Mols, F., Schoormans, D., de Hingh, I., Oerlemans, S., & Husson, O. (2018). Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES registry: Prevalence, predictors, and impact on quality of life. Cancer, 124(12), 2621–2628. doi:10.1002/cncr.31369.
National Cancer Institute. (2015). Guidelines for screening, diagnosis and treatment of colorectal cancer. Bangkok: Kosit Press Company Limited.
O'Gorman, C., Stack, J., O'Ceilleachair, A., Denieffe, S., Gooney, M., McKnight, M., & Sharp, L. (2018). Colorectal cancer survivors: An investigation of symptom burden and influencing factors. BioMed Central cancer, 18(1), 1022. doi:10.1186/s12885-018-4923-3.
Peng, Y. N., Huang, M. L., & Kao, C. H. (2019). Prevalence of depression and anxiety in colorectal cancer patients: A literature review. International journal of environmental research and public health, 16(3), 411. doi:10.3390/ijerph16030411.
Ratanatharathorn, V., Sirilerttrakul, S., Jirajarus, M., Silpakit, C., Maneechavakajorn, J., Sailamai, P., & Sirisinha, T. (2001). Quality of life, functional assessment of cancer therapy-general. Journal of the Medical Association of Thailand, 84(10), 1430-1442.
Rawla, P., Sunkara, T., & Barsouk A. (2019). Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterology Review-przeglad Gastroenterologiczny, 14(2), 89-103. doi:10.5114/pg.2018.81072.
Riihimäki, M., Hemminki, A., Sundquist, J., & Hemminki, K. (2016). Patterns of metastasis in colon and rectal cancer. Scientific Reports, 6, 29765. doi:10.1038/srep29765.
Satianpongprapa, J., Srimoragot, P., & Danaidutsadeekul, S. (2016). Factors affecting the nutritional status in postoperative colorectal cancer patients in hospital. Songklanagarind Journal of Nursing, 36(1), 143-161.
Silpakit, C., Sirilerttrakul, S., Jirajarus, M., Sirisinha, T., Sirachainan, E., & Ratanatharathorn, V. (2006). The European organization for research and treatment of cancer quality of life questionnaire (EORTC QLQ-C30): Validation study of the Thai version. Quality of Life Research, 15, 167–172. doi;10.1007/s11136-005-0449.
Srilertakoon, S., Jirajarus, M., Ratanatharathorn, V., Hanucharurnkul, S., Sirichainan, E., & Nilchaikovit, T. (2005). The reliability item total correlation and discrimination of the functional assessment of cancer therapy (FACT) scale in breast cancer patients, colorectal cancer and lung cancer patient in Thai Version. Thai Journal of Nursing Research, 11(3), 61-77.
Sun, L. M., Liang, J. A., Lin, C. L., Sun, S., & Kao, C. H. (2017). Risk of mood disorders in patients with colorectal cancer. Journal of Affective Disorders, 218, 59–65. doi:10.1016/j.jad.2017.04.050
Thanasilp, S., Suwannapong, K., & Long, N. H. (2018). Validation of the Thai version of the functional assessment cancer therapy- general (FACT-G) for persons with terminal cancer. Journal of Pain and Symptom management, 56(6), e137–e138. doi:10.1016/j.jpainsymman.2018.10.437
van der Geest, L. G., Lam-Boer, J., Koopman, M., Verhoef, C., Elferink, M. A., & de Wilt, J. H. (2015). Nationwide trends in incidence, treatment and survival of colorectal cancer patients with synchronous metastases. Clinical & experimental metastasis, 32(5), 457–465. doi:10.1007/s10585-015-9719-0
Vardy, J. L., Dhillon, H. M., Pond, G. R., Renton, C., Dodd, A., Zhang, H., . . . Tannock, I. F. (2016). Fatigue in people with localized colorectal cancer who do and do not receive chemotherapy: A longitudinal prospective study. Annals of Oncology, 27(9), 1761–1767. doi:10.1093/annonc/mdw252.
Vera, R., González-Flores, E., Rubio, C., Urbano, J., Camps, M. V., Ciampi-Dopazo, J. J., . . . Suarez-Artacho, G. (2020). Multidisciplinary management of liver metastases in patients with colorectal cancer: A consensus of SEOM, AEC, SEOR, SERVEI, and SEMNIM. Clinical Translational Oncology, 22(5), 647–662. doi:10.1007/s12094-019-02182-z
Wilson, I. B., & Cleary, P. D. (1995). Linking clinical variables with health-related quality of life-a conceptual model of patient outcomes. Journal of the American Medical Association, 273(1), 59-65.
Downloads
Published
How to Cite
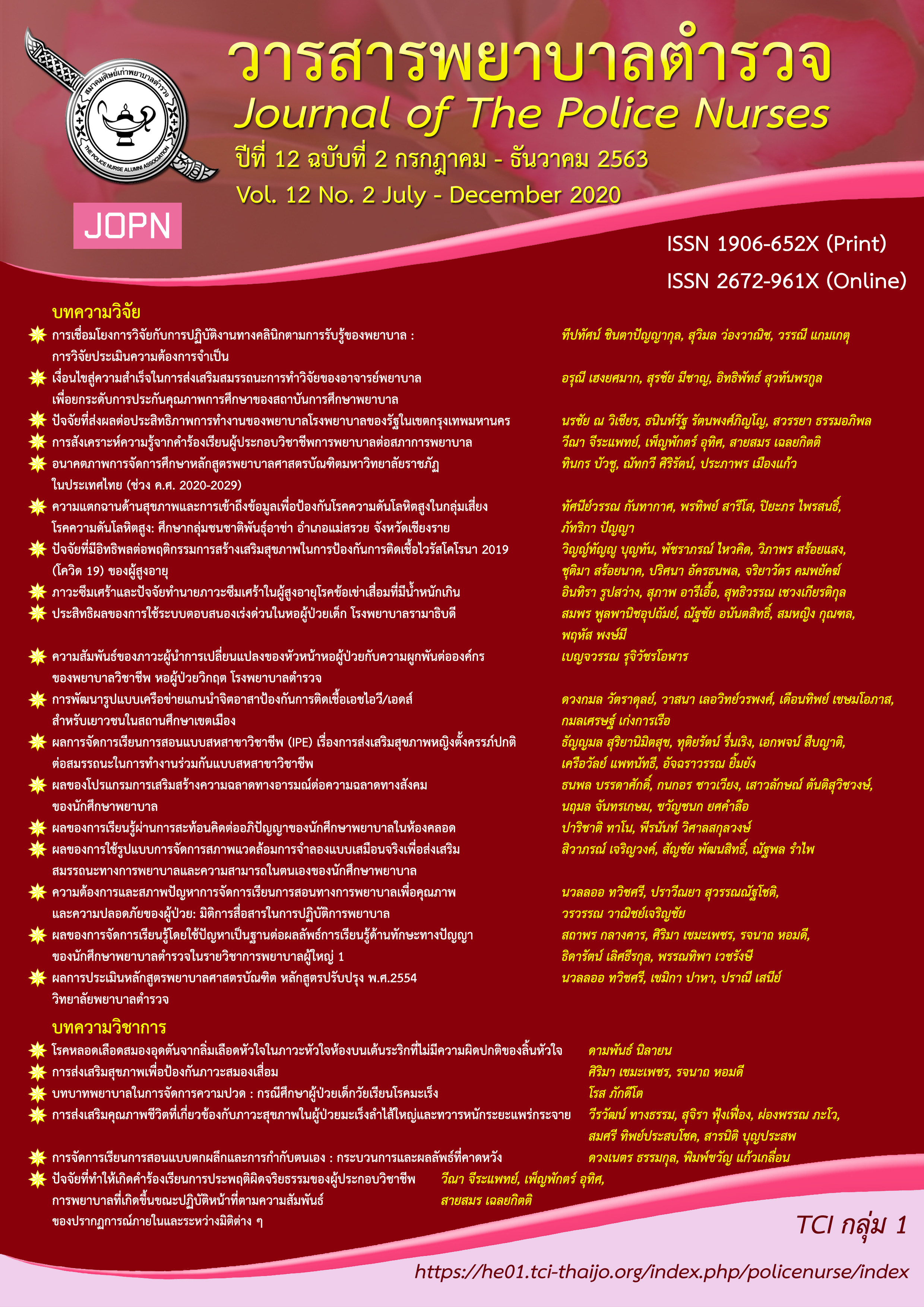
Issue
Section
License
ผลงานที่ได้ตีพิมพ์แล้วจะเป็นลิขสิทธิ์ของวารสารพยาบาลตำรวจ