ผลของการใช้รูปแบบการผดุงครรภ์แบบต่อเนื่องร่วมกับการใช้โปรแกรมประยุกต์บนสมาร์ทโฟนในการดูแลสตรีที่มีภาวะเบาหวานร่วมกับการตั้งครรภ์ในเขตเมือง
คำสำคัญ:
การผดุงครรภ์ต่อเนื่อง, ภาวะเบาหวานร่วมกับการตั้งครรภ์, แอปพลิเคชันบนสมาร์ทโฟน, พื้นที่เขตเมืองบทคัดย่อ
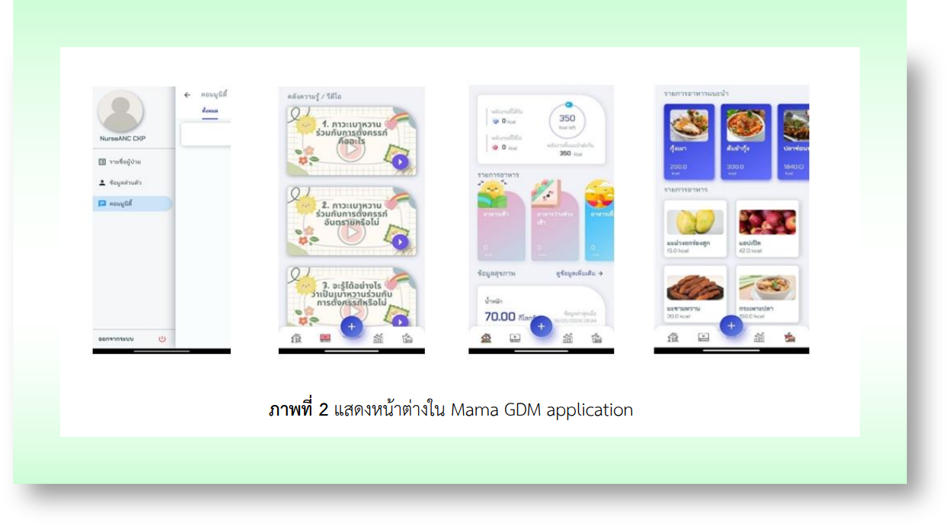
การวิจัยนี้เป็นการวิจัยแบบผสานวิธี เพื่อศึกษาผลของการใช้รูปแบบการผดุงครรภ์ต่อเนื่อง ร่วมกับการใช้โปรแกรมประยุกต์บนสมาร์ทโฟน (Mama GDM application) ในการดูแลสตรีที่มีภาวะเบาหวานร่วมกับการตั้งครรภ์ในกรุงเทพมหานคร กลุ่มตัวอย่าง คือ สตรีที่มีภาวะเบาหวานร่วมกับการตั้งครรภ์ จำนวน 60 ราย และพยาบาลผดุงครรภ์ จำนวน 9 ราย เครื่องมือในการวิจัยผ่านการตรวจสอบความตรงเชิงเนื้อหา และความเชื่อมั่น วิเคราะห์ข้อมูลโดยใช้สถิติ Independent t-test และข้อมูลเชิงคุณภาพใช้การวิเคราะห์แก่นสาระ
ผลการวิจัย พบว่า คะแนนพฤติกรรมการดูแลตนเอง และการรับรู้ของสตรีตั้งครรภ์ภายหลังได้รับรูปแบบการผดุงครรภ์ต่อเนื่องร่วมกับการใช้ Mama GDM application สูงกว่ากลุ่มควบคุม (t = 3.42; p-value < .05 และ t = 3.57; p-value < .05 ตามลำดับ) พยาบาลผดุงครรภ์สะท้อนถึงรูปแบบการผดุงครรภ์ต่อเนื่องร่วมกับการใช้ Mama GDM application 3 ประเด็น ได้แก่ 1) ส่งเสริมให้เกิดการเรียนรู้ และตระหนักในการดูแลตนเอง 2) ดูแลต่อเนื่องติดตาม และให้ข้อมูล และ 3) เข้าถึงสตรีตั้งครรภ์ในเขตเมืองได้ง่าย สตรีตั้งครรภ์สะท้อนใน 3 ประเด็น ได้แก่ 1) ความเครียดต่อสุขภาพทารกในครรภ์ 2) โอกาสในการดูแลตนเอง และ 3) ฟังก์ชันสวยงาม และง่ายต่อการเข้าถึง การใช้รูปแบบการผดุงครรภ์ต่อเนื่องร่วมกับการใช้ Mama GDM application ส่งเสริมให้สตรีสามารถดูแลตนเอง และมีความมั่นใจเพื่อให้เกิดความปลอดภัยทั้งต่อสตรีและทารกในครรภ์
เอกสารอ้างอิง
Sirirat S, Ruangvutilert P, Yapan P, Boriboonhirunsarn D. Prevalence of gestational diabetes mellitus among women with lower risk for gestational diabetes in Siriraj hospital. Thai Journal of Obstetrics and Gynaecology 2022;30(5):313-20. (in Thai)
Netimetee S, Boobpamala S. Nursing care for pregnant women with gestational diabestes mellitus during pregnancy. Journal of Health and Nursing Education 2022;28(1):e256658.
Fakier A, Petro G, Fawcus S. Mid-upper arm circumference: a surrogate for body mass index in pregnant women. South African Medical Journal 2017;107(7):606-10. doi: 10.7196/SAMJ.2017.v107i7.12255.
Msollo SS, Martin HD, Mwanri AW, Petrucka P. Prevalence of hyperglycemia in pregnancy and influence of body fat on development of hyperglycemia in pregnancy among pregnant women in urban areas of Arusha region, Tanzania. BioMed Central Pregnancy and Childbirth 2019;19:315. doi: 10.1186/s12884-019-2463-8.
Shi P, Liu A, Yin X. Association between gestational weight gain in women with gestational diabetes mellitus and adverse pregnancy outcomes: a retrospective cohort study. BioMed Central Pregnancy and Childbirth 2021;21:508. doi: 10.1186/s12884-021-03982-4.
Nasreen S, Wilk P, Mullowney T, Karp I. The effect of gestational diabetes mellitus on the risk of asthma in offspring. Annals of Epidemiology 2021;57:7-13. doi: 10.1016/j.annepidem.2021.02.003.
Pathirana MM, Lassi ZS, Ali A, Arstall MA, Roberts CT, Andraweera PH. Association between metabolic syndrome and gestational diabetes mellitus in women and their children: a systematic review and meta-analysis. Endocrine 2021;71(2):310-20. doi: 10.1007/s12020-020-02492-1.
Mistry SK, Gupta RD, Alam S, Kaur K, Shamim AA, Puthussery S. Gestational diabetes mellitus (GDM) and adverse pregnancy outcome in South Asia: a systematic review. Endocrinology, Diabetes and Metabolism 2021;4(4):e00285. doi: 10.1002/edm2.285.
Wang M, Hu RY, Gong WW, Pan J, Fei FR, Wang H, et al. Trends in prevalence of gestational diabetes mellitus in Zhejiang province, China, 2016-2018. Nutrition and Metabolism 2021;18(1):12. doi: 10.1186/s12986-020-00539-8.
Gagné-Ouellet V, Breton E, Thibeault K, Fortin CA, Cardenas A, Guérin R, et al. Mediation analysis supports a causal relationship between maternal hyperglycemia and placental DNA methylation variations at the leptin gene locus and cord blood leptin levels. International Journal of Molecular Sciences 2020;21(1):329. doi: 10.3390/ijms21010329.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. 2016 [cited 2021 Oct 11]. Available from: https://www.who.int/publications/i/item/9789241549912
Homer C, Brodie P, Leap N, Sandall J. Midwifery continuity of care: a practical guide. 2nd ed. New South Wales: Elsevier Australia; 2019.
Taylor BI. Diabetic continuity of care and A1c outcomes: evaluating single vs. multiple provider continuity of care of type II diabetics in a rural community medical home [Dissertation]. Pennsylvania: Carlow University; 2018.
Turienzo CF, Silverio SA, Coxon K, Brigante L, Seed PT, Shennan AH, et al. Experiences of maternity care among women at increased risk of preterm birth receiving midwifery continuity of care compared to women receiving standard care: results from the POPPIE pilot trial. PloS one 2021;16(4):e0248588. doi: 10.1371/journal.pone.0248588.
Thailand Nursing and Midwifery Council. Announcement of the nursing and midwifery council on the nursing and midwifery council’s statement during the COVID-19 outbreak situation [Internet]. 2016 [cited 2021 Oct 11]. Available from: https://www.ratchakitcha.soc.go.th/DATA/PDF/2564/E/033/T_0049.PDF (in Thai)
Eberle C, Stichling S. Telemedical approaches to managing gestational diabetes mellitus during COVID-19: systematic review. JMIR Pediatrics and Parenting 2021;4(3):e28630. doi: 10.2196/28630.
Gandhi K, Ives R. The efficacy of mHealth interventions in treatment of gestational diabetes mellitus: a research protocol. Undergraduate Research in Natural and Clinical Science and Technology Journal 2021;5(3):1-6. doi: 10.26685/urncst.220.
Immanuel J, Simmons D. Apps and the woman with gestational diabetes mellitus. Diabetes Care 2021;44(2):313-5. doi: 10.2337/dci20-0068.
Guo H, Zhang Y, Li P, Zhou P, Chen LM, Li SY. Evaluating the effects of mobile health intervention on weight management, glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus. Journal of Endocrinological Investigation 2019;42(6):709-14. doi: 10.1007/s40618-018-0975-0.
Yew TW, Chi C, Chan SY, van Dam RM, Whitton C, Lim CS, et al. A randomized controlled trial to evaluate the effects of a smartphone application-based lifestyle coaching program on gestational weight gain, glycemic control, and maternal and neonatal outcomes in women with gestational diabetes mellitus: the SMART-GDM study. Diabetes Care 2021;44(2):456-63. doi: 10.2337/dc20-1216.
Creswell JW, Clark VLP. Designing and conducting mixed methods research. Los Angeles: SAGE; 2017.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 9th ed. Philadelphia: Lippincott, Williams and Wilkins; 2012.
Prasan S, Siriarunrat S, Tachasuksri T. Effects of continuous labor support programme on fear of childbirth and childbirth outcomes among primiparous women. Nursing Journal of the Ministry of Public Health 2021;31(1):148-60. (in Thai)
Coates D, Foureur M. The role and competence of midwives in supporting women with mental health concerns during the perinatal period: a scoping review. Health and Social Care in the Community 2019;27(4):e389-405. doi: 10.1111/hsc.12740.
Panmuang S, Sutthiprapa A, Phuakphan W. The development of self-care program for pregnant women with gestational diabetes mellitus. Journal of Health Research and Development, Nakhon Ratchasima Provincial Public Health Office 2023;9(1):130-44. (in Thai)
Viveiros CJ, Darling EK. Barriers and facilitators of accessing perinatal mental health services: the perspectives of women receiving continuity of care midwifery. Midwifery 2018;65:8-15. doi: 10.1016/j.midw.2018.06.018.
Forster DA, McLachlan HL, Davey MA, Biro MA, Farrell T, Gold L, et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BioMed Central Pregnancy and Childbirth 2016;16:28. doi: 10.1186/s12884-016-0798-y.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2025 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















