ปัจจัยทำนายพฤติกรรมสุขภาพของผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019
คำสำคัญ:
แบบแผนความเชื่อด้านสุขภาพ, ผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019, พฤติกรรมสุขภาพบทคัดย่อ
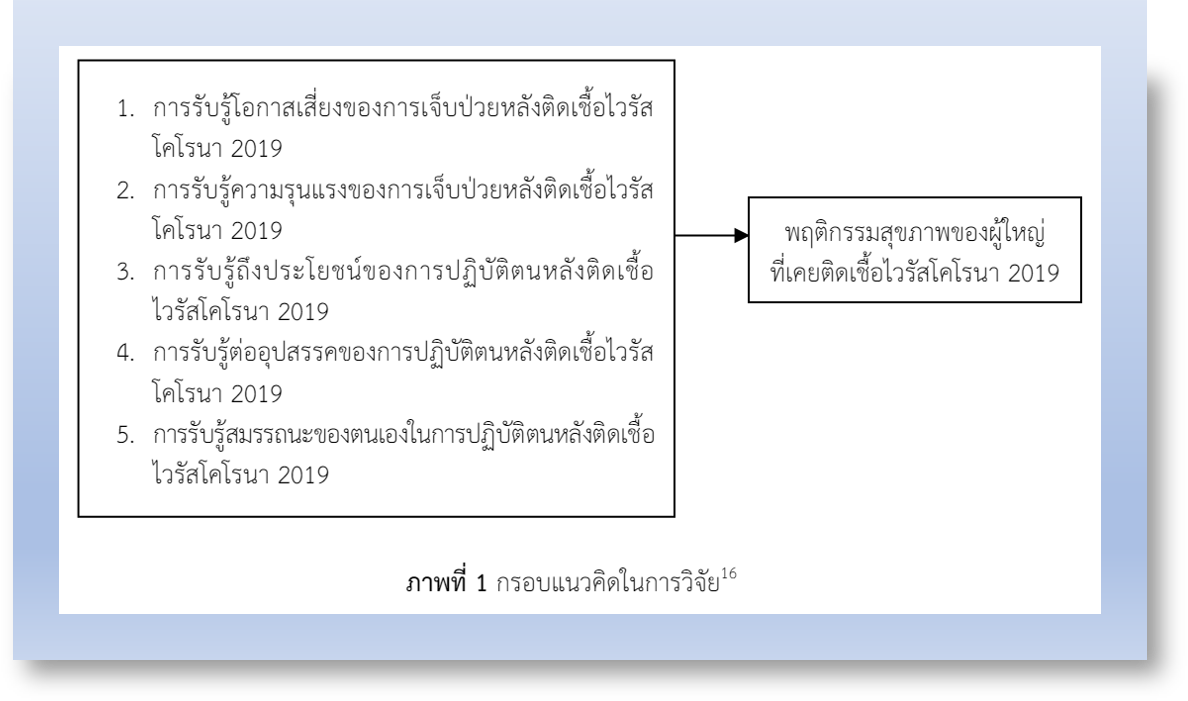
การวิจัยแบบหาความสัมพันธ์เชิงทำนายนี้ เพื่อศึกษาปัจจัยทำนายพฤติกรรมสุขภาพของผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019 กลุ่มตัวอย่าง คือ ผู้ใหญ่อายุ 18 - 59 ปี มีประวัติเคยติดเชื้อไวรัสโคโรนา 2019 ตั้งแต่ 1 ปีขึ้นไป ที่มารับบริการในแผนกผู้ป่วยนอกโรงพยาบาลจุฬาลงกรณ์ สภากาชาดไทย จำนวน 131 ราย เครื่องมือเก็บรวบรวมข้อมูล ประกอบด้วย แบบบันทึกข้อมูลทั่วไป แบบบันทึกข้อมูลสุขภาพ แบบประเมินพฤติกรรมสุขภาพ และแบบประเมินการรับรู้ภาวะสุขภาพ ค่าดัชนีความตรงเชิงเนื้อหาของแบบประเมินพฤติกรรมสุขภาพ และแบบประเมินการรับรู้ภาวะสุขภาพ เท่ากับ .99 ค่าสัมประสิทธิ์แอลฟาของครอนบาค เท่ากับ .82 และ .81 ตามลำดับ วิเคราะห์ข้อมูลโดยใช้สถิติสหสัมพันธ์เพียร์สัน และสถิติการวิเคราะห์ถดถอยพหุคูณแบบเป็นขั้นตอน
ผลการวิจัย พบว่า ผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019 มีพฤติกรรมสุขภาพในระดับดีมาก คะแนนอยู่ในช่วง 128 - 167 คะแนน (Mean = 153.32, SD = 6.71) ปัจจัยการรับรู้ถึงประโยชน์ของการปฏิบัติตน และปัจจัยการรับรู้สมรรถนะของตนเองในการปฏิบัติตน สามารถร่วมกันทำนายพฤติกรรมสุขภาพของผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019 ได้ร้อยละ 16.30 (R2 = .163) อย่างมีนัยสำคัญทางสถิติที่ระดับ .05 ข้อเสนอแนะจากผลการวิจัย พยาบาลควรมีแนวทางส่งเสริมพฤติกรรมสุขภาพสำหรับผู้ใหญ่ที่เคยติดเชื้อไวรัสโคโรนา 2019 ทั้งนี้ เพื่อคงไว้ซึ่งพฤติกรรมสุขภาพที่ดีอย่างต่อเนื่อง
เอกสารอ้างอิง
World Health Organization. Coronavirus disease (COVID-19) [Internet]. 2023 [cited 2024 Mar 1]. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_1
Department of Disease Control. Surveillance management of coronavirus disease 2019 (COVID-19) [Internet]. 2021 [cited 2024 Mar 1]. Available from: https://ddc.moph.go.th/viralpneumonia/file/g_srrt/g_srrt_090364.pdf (in Thai)
World Health Organization. Number of COVID-19 cases reported to WHO [Internet]. 2024 [cited 2024 Mar 1]. Available from: https://data.who.int/dashboards/covid19/cases?n=c
Department of Disease Control. COVID-19 patient situation updated daily [Internet]. 2023 [cited 2024 Mar 1]. Available from: https://public.tableau.com/views/SATCOVIDDashboard/1-dash-tiles?:showVizHome=no (in Thai)
Ahmed GK, Khedr EM, Hamad DA, Meshref TS, Hashem MM, Aly MM. Long term impact of Covid-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Research 2021;305:114243. doi: 10.1016/j.psychres.2021.114243.
Gavriatopoulou M, Korompoki E, Fotiou D, Ntanasis-Stathopoulos I, Psaltopoulou T, Kastritis E, et al. Organ-specific manifestations of COVID-19 infection. Clinical and Experimental Medicine 2020;20(4):493-506. doi: 10.1007/s10238-020-00648-x.
Zhang P, Li J, Liu H, Han N, Ju J, Kou Y, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Research 2020;8:8. doi: 10.1038/s41413-020-0084-5.
Zhou F, Tao M, Shang L, Liu Y, Pan G, Jin Y, et al. Assessment of sequelae of COVID-19 nearly 1 year after diagnosis. Frontiers in Medicine 2021;8:717194. doi: 10.3389/fmed.2021.717194.
McBride E, Arden MA, Chater A, Chilcot J. The impact of COVID-19 on health behaviour, well-being, and long-term physical health. British Journal of Health Psychology 2021;26(2):259-70. doi: 10.1111/bjhp.12520.
Health Education Division. Assessment of public health literacy and health behavior to prevent important infectious and non-infectious diseases of people of working age in the village, change health behavior in 2023 [Internet]. 2023 [cited 2024 Mar 1]. Available from: https://hed.go.th/wp-content/uploads/2024/05/คู่มือการเฝ้าระวังและเตือนภัยพฤติกรรมสุขภาพในชุมชน.pdf (in Thai)
Clemente-Suarez VJ, Ramos-Campo DJ, Mielgo-Ayuso J, Dalamitros AA, Nikolaidis PA, Hormeno-Holgado A, et al. Nutrition in the actual COVID-19 pandemic. A narrative review. Nutrients 2021;13(6):1924. doi: 10.3390/nu13061924.
Weaver RH, Jackson A, Lanigan J, Power TG, Anderson A, Cox AE, et al. Health behaviors at the onset of the COVID-19 pandemic. American Journal of Health Behavior 2021;45(1):44-61. doi: 10.5993/AJHB.45.1.4.
Veljkovic M, Pavlovic DR, Stojanovic NM, Dzopalic T, Dragonjic LP. Behavioral and dietary habits that could influence both COVID-19 and non-communicable civilization disease prevention-what have we learned up to now?. Medicina 2022;58(11):1686. doi: 10.3390/medicina58111686.
Garcia-Esquinas E, Ortola R, Gine-Vazquez I, Carnicero JA, Manas A, Lara E, et al. Changes in health behaviors, mental and physical health among older adults under severe lockdown restrictions during the COVID-19 pandemic in Spain. International Journal of Environmental Research and Public Health 2021;18(13):7067. doi: 10.3390/ijerph18137067.
Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. Journal of Epidemiology and Community Health 2021;75(3):224-31. doi: 10.1136/jech-2020-215060.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly 1988;15(2):175-83. doi: 10.1177/109019818801500203.
Zewdie A, Mose A, Sahle T, Bedewi J, Gashu M, Kebede N, et al. The health belief model’s ability to predict COVID-19 preventive behavior: a systematic review. SAGE Open Medicine 2022;10:20503121221113668. doi: 10.1177/20503121221113668.
Yanti N, Wiangpati T. Self care behaviors during the corona virus disease (COVID-19) outbreak in Khlong Nueng sub-district, Khlong Luang district, Pathumthani province. VRU Research and Development Journal Science and Technology 2022;17(1):57-70. (in Thai)
Hongpanich P. Factors Influencing COVID -19 prevention behaviors of the peoples in Pathumthani province. The Journal of Pacific Institute of Management Science 2021;7(3):174-85. (in Thai)
Klunduang S. Health literacy and preventative behaviors for coronavirus disease-2019 (COVID-19) of the people who received the Vaccines against COVID-19 service at the service point of Khon Kaen Hospital. Journal of Regional Health Promotion Centre 7 KhonKaen 2022;14(1):79-96. (in Thai)
Chuenchom J, Tuntong T, Chuenchom P, Somboon L, Thanakumma O. Factors predicting health promoting behaviors among persons with chronic obstructive pulmonary disease in Wiang Chiang Rung hospital Chiang Rai province. Nursing Journal CMU 2015;42(4):86-97. (in Thai)
Alagili DE, Bamashmous M. The health belief model as an explanatory framework for COVID-19 prevention practices. Journal of Infection and Public Health 2021;14(10):1398-403. doi: 10.1016/j.jiph.2021.08.024.
Kim S, Kim S. Analysis of the impact of health beliefs and resource factors on preventive behaviors against the COVID-19 pandemic. International Journal of Environmental Research and Public Health 2020;17(22):8666. doi: 10.3390/ijerph17228666.
Yildirim M, Guler A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Studies 2022;46(4):979-86. doi: 10.1080/07481187.2020.1793434.
Chu H, Liu S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Education and Counseling 2021;104(8):1878-86. doi: 10.1016/j.pec.2021.02.031.
Kor-issaranuphab N, Samrannet W, Arsa P. Factors related to self-protective behaviors for coronavirus disease 2019 infection among type 2 diabetic patients. Journal of Sakon Nakhon Hospital 2022;25(1):43-55. (in Thai)
Tam CC, Li X, Li X, Wang Y, Lin D. Adherence to preventive behaviors among college students during COVID-19 pandemic in China: the role of health beliefs and COVID-19 stressors. Current Psychology 2021;9(1):1-11. doi: 10.1007/s12144-021-01942-x.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2024 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















