ปัจจัยทำนายการเกิดภาวะแทรกซ้อนหลังผ่าตัดในผู้ป่วยหลอดเลือดสมองโป่งพองแตก
คำสำคัญ:
ภาวะแทรกซ้อนหลังผ่าตัด, หลอดเลือดสมองโป่งพองแตก, เม็ดเลือดขาว, ภาวะโรคร่วม, สภาพร่างกายระหว่างผ่าตัดบทคัดย่อ
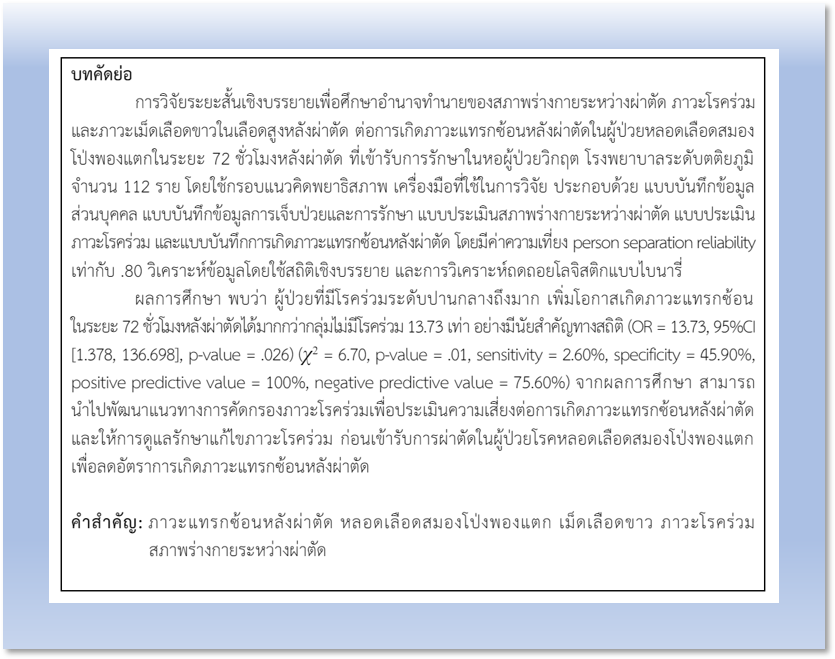
การวิจัยระยะสั้นเชิงบรรยายเพื่อศึกษาอำนาจทำนายของสภาพร่างกายระหว่างผ่าตัด ภาวะโรคร่วม และภาวะเม็ดเลือดขาวในเลือดสูงหลังผ่าตัด ต่อการเกิดภาวะแทรกซ้อนหลังผ่าตัดในผู้ป่วยหลอดเลือดสมองโป่งพองแตกในระยะ 72 ชั่วโมงหลังผ่าตัด ที่เข้ารับการรักษาในหอผู้ป่วยวิกฤต โรงพยาบาลระดับตติยภูมิ จำนวน 112 ราย โดยใช้กรอบแนวคิดพยาธิสภาพ เครื่องมือที่ใช้ในการวิจัย ประกอบด้วย แบบบันทึกข้อมูลส่วนบุคคล แบบบันทึกข้อมูลการเจ็บป่วยและการรักษา แบบประเมินสภาพร่างกายระหว่างผ่าตัด แบบประเมินภาวะโรคร่วม และแบบบันทึกการเกิดภาวะแทรกซ้อนหลังผ่าตัด โดยมีค่าความเที่ยง person separation reliability เท่ากับ .80 วิเคราะห์ข้อมูลโดยใช้สถิติเชิงบรรยาย และการวิเคราะห์ถดถอยโลจิสติกแบบไบนารี่
ผลการศึกษา พบว่า ผู้ป่วยที่มีโรคร่วมระดับปานกลางถึงมาก เพิ่มโอกาสเกิดภาวะแทรกซ้อนในระยะ 72 ชั่วโมงหลังผ่าตัดได้มากกว่ากลุ่มไม่มีโรคร่วม 13.73 เท่า อย่างมีนัยสำคัญทางสถิติ (OR = 13.73, 95%CI [1.378, 136.698], p-value = .026) (χ2 = 6.70, p-value = .01, sensitivity = 2.60%, specificity = 45.90%, positive predictive value = 100%, negative predictive value = 75.60%) จากผลการศึกษา สามารถนำไปพัฒนาแนวทางการคัดกรองภาวะโรคร่วมเพื่อประเมินความเสี่ยงต่อการเกิดภาวะแทรกซ้อนหลังผ่าตัด และให้การดูแลรักษาแก้ไขภาวะโรคร่วม ก่อนเข้ารับการผ่าตัดในผู้ป่วยโรคหลอดเลือดสมองโป่งพองแตก เพื่อลดอัตราการเกิดภาวะแทรกซ้อนหลังผ่าตัด
เอกสารอ้างอิง
Revilla-Pacheco F, Escalante-Seyffert MC, Herrada-Pineda T, Manrique-Guzman S, Perez-Zuniga I, Rangel-Suarez S, et al. Prevalence of incidental clinoid segment saccular aneurysms. World Neurosurgery 2018;115:e244-51. doi: 10.1016/j.wneu.2018.04.027.
Information System Development Group: Department of Medical Services. Mortality of patients with cerebral stroke (Hemorrhagic Stroke: I60-I62) [Internet]. 2024 [cited 4 Feb 2024]. Available from: https://medinfo.dms.go.th/public-health/kpi_reports.php?kpi_year=2566&id=2 (in Thai)
Chung DY, Abdalkader M, Nguyen TN. Aneurysmal subarachnoid hemorrhage. Neurologic Clinics 2021;39(2):419-42. doi: 10.1016/j.ncl.2021.02.006.
Jin J, Duan J, Du L, Xing W, Peng X, Zhao Q. Inflammation and immune cell abnormalities in intracranial aneurysm subarachnoid hemorrhage (SAH): relevant signaling pathways and therapeutic strategies. Frontiers in Immunology 2022;13:1027756. doi: 10.3389/fimmu.2022.1027756.
Pont W, Groeneveld I, Arwert H, Meesters J, Mishre RR, Vlieland TV, et al. Caregiver burden after stroke: changes over time?. Disability and rehabilitation 2020;42(3):360-7. doi: 10.1080/09638288.2018.1499047.
Waiyapat B. Case study: nursing care for patients with cerebral artery aneurysms. Journal of Preventive Medicine Association of Thailand 2016;6(1):71-9. (in Thai)
Dixon KJ. Pathophysiology of traumatic brain injury. Physical Medicine and Rehabilitation Clinics 2017;28(2):215-25. doi: 10.1016/j.pmr.2016.12.001.
Mangat HS. Severe traumatic brain injury. Continuum: Lifelong Learning in Neurology 2012;18(3):532-46. doi: 10.1212/01.CON.0000415426.76524.e1.
Fugate JE. Complications of neurosurgery. Continuum: Lifelong Learning in Neurology 2015;21(5 Neurocritical Care):1425-44. doi: 10.1212/CON.0000000000000227.
Nanda A, Patra DP. Surgical complications in neurosurgery. In: Nanda A, editor. Complications in neurosurgery. London: Elsevier; 2019. p. 17-22.
Narayan V, Kalakoti P, Nanda A. Medical complications in neurosurgery. In: Nanda A, editor. Complications in neurosurgery. London: Elsevier; 2019. p. 13-6.
Kamide T, Burkhardt JK, Tabani H, Safaee M, Lawton MT. Microsurgical clipping techniques and outcomes for paraclinoid internal carotid artery aneurysms. Operative Neurosurgery 2020;18(2):183-92. doi: 10.1093/ons/opz157.
Algattas H, Kimmell KT, Vates GE. Risk of reoperation for hemorrhage in patients after craniotomy. World Neurosurgery 2016;87:531-9. doi: 10.1016/j.wneu.2015.09.020.
Cinotti R, Bruder N, Srairi M, Paugam-Burtz C, Beloeil H, Pottecher J, et al. Prediction score for postoperative neurologic complications after brain tumor craniotomy: a multicenter observational study. Anesthesiology 2018;129(6):1111-20. doi: 10.1097/ALN.0000000000002426.
Lonjaret L, Guyonnet M, Berard E, Vironneau M, Peres F, Sacrista S, et al. Postoperative complications after craniotomy for brain tumor surgery. Anaesthesia, Critical Care and Pain Medicine 2017;36(4):213-8. doi: 10.1016/j.accpm.2016.06.012.
Carli F. Physiologic considerations of enhanced recovery after surgery (ERAS) programs: implications of the stress response. Canadian Journal of Anaesthesia 2015;62(2):110-9. doi: 10.1007/s12630-014-0264-0.
Helander EM, Webb MP, Menard B, Prabhakar A, Helmstetter J, Cornett EM, et al. Metabolic and the surgical stress response considerations to improve postoperative recovery. Current Pain and Headache Reports 2019;23(5):33. doi: 10.1007/s11916-019-0770-4.
Vel R, Udupi BP, Satya Prakash MVS, Adinarayanan S, Mishra S, Babu L. Effect of low dose tranexamic acid on intra-operative blood loss in neurosurgical patients. Saudi Journal of Anaesthesia 2015;9(1):42-8. doi: 10.4103/1658-354X.146304.
Kim Y, Han MH, Kim CH, Kim JM, Cheong JH, Ryu JI. Increased short-term mortality in patients with spontaneous intracerebral hemorrhage and its association with admission glucose levels and leukocytosis. World Neurosurgery 2017;98:503-11. doi: 10.1016/j.wneu.2016.11.087.
Yu Z, Zheng J, Guo R, Ma L, You C, Li H. Prognostic impact of leukocytosis in intracerebral hemorrhage: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 2019;98(28):e16281. doi: 10.1097/MD.0000000000016281.
Tao C, Wang J, Hu X, Ma J, Li H, You C. Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocritical Care 2017;26(3):393-401. doi: 10.1007/s12028-016-0332-0.
Ibañez FAL, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, et al. A new classification of complications in neurosurgery. World Neurosurgery 2011;75(5-6):709-15. doi: 10.1016/j.wneu.2010.11.010.
Rock AK, Dincer A, Carr MT, Opalak CF, Workman KG, Broaddus WC. Outcomes after craniotomy for resection of craniopharyngiomas in adults: analysis of the National Surgical Quality Improvement Program (NSQIP). Journal of Neuro-Oncology 2019;144(1):117-25. doi: 10.1007/s11060-019-03209-9.
Charlson ME, Charlson RE, Peterson JC, Marinopoulos SS, Briggs WM, Hollenberg JP. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. Journal of Clinical Epidemiology 2008;61(12):1234-40. doi: 10.1016/j.jclinepi.2008.01.006.
Gawande AA, Kwaan MR, Regenbogen SE, Lipsitz SA, Zinner MJ. An Apgar score for surgery. Journal of the American College of Surgeons 2007;204(2):201-8. doi: 10.1016/j.jamcollsurg.2006.11.011.
Roffman CE, Buchanan J, Allison GT. Charlson comorbidities index. Journal of Physiotherapy 2016;62(3):171. doi: 10.1016/j.jphys.2016.05.008.
Hsu SY, Ou CY, Ho YN, Huang YH. Application of surgical Apgar score in intracranial meningioma surgery. PLoS One 2017;12(4):e0174328. doi: 10.1371/journal.pone.0174328.
Vecchio TG, Corell A, Buvarp D, Rydén I, Smits A, Jakola AS. Classification of adverse events following surgery in patients with diffuse lower-grade gliomas. Frontiers in Oncology 2021;11:792878. doi: 10.3389/fonc.2021.792878.
Johans SJ, Garst JR, Burkett DJ, Grahnke K, Martin B, Ibrahim TF, et al. Identification of preoperative and intraoperative risk factors for complications in the elderly undergoing elective craniotomy. World Neurosurgery 2017;107:216-25. doi: 10.1016/j.wneu.2017.07.177.
Hsu SY, Huang YH. Characterization and prognostic implications of significant blood loss during intracranial meningioma surgery. Translational Cancer Research 2016;5(6):797-804. doi: 10.21037/tcr.2016.11.72.
Ma X, Lan F, Zhang Y. Associations between C-reactive protein and white blood cell count, occurrence of delayed cerebral ischemia and poor outcome following aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Acta Neurologica Belgica 2021;121(5):1311-24. doi: 10.1007/s13760-020-01496-y.
Burzynska M, Uryga A, Wozniak J, Załuski R, Robba C, Gozdzik W. The role of early serum biomarkers and clinical rating scales in the prediction of delayed cerebral ischaemia and short-term outcome after aneurysmal subarachnoid haemorrhage: single centre experience. Journal of Clinical Medicine 2023;12(17):5614. doi: 10.3390/jcm12175614.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2024 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















