การพัฒนาต้นแบบอุปกรณ์ยึดและป้องกันการกัดท่อช่วยหายใจ
คำสำคัญ:
อุปกรณ์ยึดท่อช่วยหายใจ, การยึดท่อช่วยหายใจ, อุปกรณ์ป้องกันการกัดท่อช่วยหายใจ, การเลื่อนหลุดของท่อช่วยหายใจบทคัดย่อ
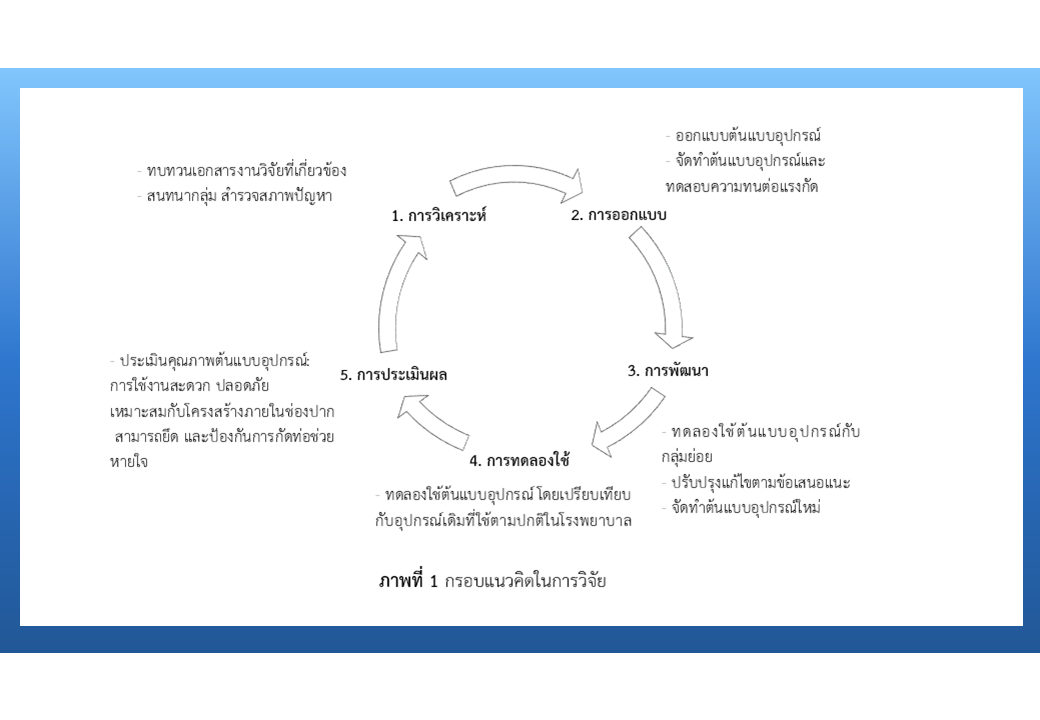
งานวิจัยนี้มีวัตถุประสงค์เพื่อพัฒนา และประเมินคุณภาพต้นแบบอุปกรณ์ยึด และป้องกันการกัดท่อช่วยหายใจ กลุ่มตัวอย่างเป็นพยาบาลวิชาชีพ จำนวน 36 คน เครื่องมือที่ใช้ ได้แก่ แบบสัมภาษณ์แบบกึ่งโครงสร้าง แบบบันทึกเวลา แบบประเมินคุณภาพอุปกรณ์ อุปกรณ์ยึดและป้องกันการกัดท่อช่วยหายใจ และหุ่นจำลองมนุษย์ ตรวจสอบคุณภาพเครื่องมือโดยหาค่าความตรงเชิงเนื้อหามีค่า .50 - 1.00 วิเคราะห์ค่าสัมประสิทธิ์แอลฟาครอนบราคมีค่า .82 วิเคราะห์ข้อมูลด้วยสถิติเชิงพรรณนา และวิเคราะห์ความแปรปรวนทางเดียวแบบวัดซ้ำ
ผลการศึกษา พบว่า การใช้ผ้าหรือพลาสเตอร์ยึดท่อช่วยหายใจใช้งานไม่สะดวก ทำให้เกิดการระคายเคือง และแผลกดทับ การใส่ oropharyngeal airway ทำให้เสี่ยงต่อการสำลัก ผู้วิจัยจึงพัฒนาต้นแบบอุปกรณ์ที่ทำจากพลาสติกที่ใช้งานสะดวก และปลอดภัย นำไปทดลองใช้ พบว่า คุณภาพโดยรวมอยู่ในระดับดี ด้านที่มีคะแนนเฉลี่ยสูงที่สุด คือ ความสะดวกในการดูแลความสะอาดในช่องปาก (Mean = 3.20, SD = .62) ออกแบบเหมาะสมกับโครงสร้างภายในช่องปาก (Mean = 3.10, SD = .55) และใช้งานสะดวก (Mean = 3.10, SD = .62) นอกจากนี้ พบว่า ใช้เวลาในการเปลี่ยนอุปกรณ์น้อยกว่าการใช้ผ้า และพลาสเตอร์ (F = 217.386, p-value = .000) ผลจากการศึกษานี้ สรุปได้ว่าต้นแบบอุปกรณ์มีคุณสมบัติเหมาะสมในการยึด และป้องกันการกัดท่อช่วยหายใจ
เอกสารอ้างอิง
Sukkul A, Sriwantha S, Phatharapreeyakul L. The effect of utilizing clinical nursing practice guideline for prevention incidence of unplanned extubation in critically ill patients. Journal of Nursing Division 2020;47(3):122-41. (in Thai)
Cosentino C, Fama M, Foà C, Bromuri G, Giannini S, Saraceno M, et al. Unplanned extubations in intensive care unit. evidences for risk factors: a literature review. Acta Biomedica 2017;88(5S):55-65. doi: 10.23750/abm.v88i5-S.6869.
Salakkham P, Pokathip S, Jareunsee P, Wasombut O, Pumthong P, Saythong S. Situation of unplanned extubation in Sappasitthiprasong hospital. Sanpasitthiprasong Medical Journal 2019;40(1-3):51-60. (in Thai)
Nakrit B, Namvongprom A, Pakdevong N. Unplanned extubation and duration of mechanical ventilation in critically ill patients on evidenced based nursing practice. Kuakarun Journal of Nursing 2015;22(1):129-43. (in Thai)
Kwon E, Choi K. Case-control study on risk factors of unplanned extubation based on patient safety model in critically ill patients with mechanical ventilation. Asian Nursing Research 2017;11(1):74-8.
Suttason M, Kaewkullay K, Naiyapatana W. Effects of utilizing clinical nursing practice guideline on the incidence of unplanned extubation in critically ill patients. Journal of Nursing and Education 2017;10(2):58-70. (in Thai)
Kim CH, Kim MS, Kang MJ, Kim HH, Park NJ, Jung HK. Oral mucosa pressure ulcers in intensive care unit patients: a preliminary observational study of incidence and risk factors. Journal of Tissue Viability 2019;28(1):27-34.
Kumar A, Mullick P, Prakash S. Guedel airway: not a bite block!. British Journal of Anaesthesia 2015;115. doi: 10.1093/bja/el_12771.
Knowledge management division. Faculty of medicine Siriraj hospital, Mahidol university. method for securing the endotracheal tube with the clove hitch knot [internet]. 2016 [cited 2023 Sep 6]. Available from: https://www2.si.mahidol.ac.th/km/cop/cop
Landsperger JS, Byram JM, Lloyd BD, Rice TW. The effect of adhesive tape versus endotracheal tube fastener in critically ill adults: the endotracheal tube securement (ETTS) randomized controlled trial. Critical Care 2019;23(161):1-7. doi: 10.1186/s13054-019-2440-7.
Cheung L. Using the ADDIE model of instructional design to teach chest radiograph interpretation [Internet]. 2016 [cited 2022 Sep 4]. Available from: https://www.hindawi.com/journals/jbe/2016/9502572/12
Žižlavsky O. Past present and future of the innovation process. International Journal of Engineering Business Management 2013;5(47):1-8. doi: 10.5772/56920.
Levartovsky S, Peleg G, Matalon S, Tsesis I, Rosen E. Maximal bite force measured via digital bite force transducer in subjects with or without dental implants - a pilot study. Applied Sciences 2022;12(3):1544.
Suttapanit K, Yuksen C, Aramvanitch K, Meemongkol T, Chandech A, Songkathee B, et al. Comparison of the effectiveness of endotracheal tube holder with the conventional method in a manikin model. Turkish Journal Emergency Medicine 2020;20:175-9.
Phonphotthanamat W. A comparative study of verifying the content validity of a research Instrument with the IOC, CVR and CVI. RSU Library Journal 2022;28(1):169-92. (in Thai)
Meehanpong P, Boonsin S. The development of nursing research instruments. Journal of The Royal Thai Army Nurses 2023;22(1):10-19. (in Thai)
Kucklick TR. “The medical device R&D handbook.” second edition. United Kingdom: CRC Press; 2013.
Isfahani MN, Abootalebi A, Ghaznavi K, Dolatabadi LK. Comparison of the effectiveness of two types of commercial endotracheal tube holders, with the conventional method in a manikin model. Advanced Biomedical Research 2023;12:30. doi: 10.4103/abr.abr_192_21.
Haaland K. Comparison of non-specialized versus specialized ties for endotracheal tube fixation [Dissertation]. Stavanger Norway: University of Stavanger; 2018.
Alatawi M, Aljuhani E, Alsufiany F, Aleid K, Rawah R, Aljanabi S, et al. Barriers of implementing evidence-based practice in nursing profession: a literature review. American Journal of Nursing Science 2020;9(1):35-42. doi: 10.11648/j.ajns.20200901.16.
Pengpala K. Which is the best endotracheal tube fixation method?. Journal of Nursing and Patient Care 2022;7(3):1.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















