ประสิทธิผลของโปรแกรมการจัดการตนเองร่วมกับการฝึกสติในผู้ป่วยโรคเบาหวานที่คุมไม่ได้
คำสำคัญ:
การจัดการตนเอง, การฝึกสติ, ผู้ป่วยโรคเบาหวานที่คุมไม่ได้บทคัดย่อ
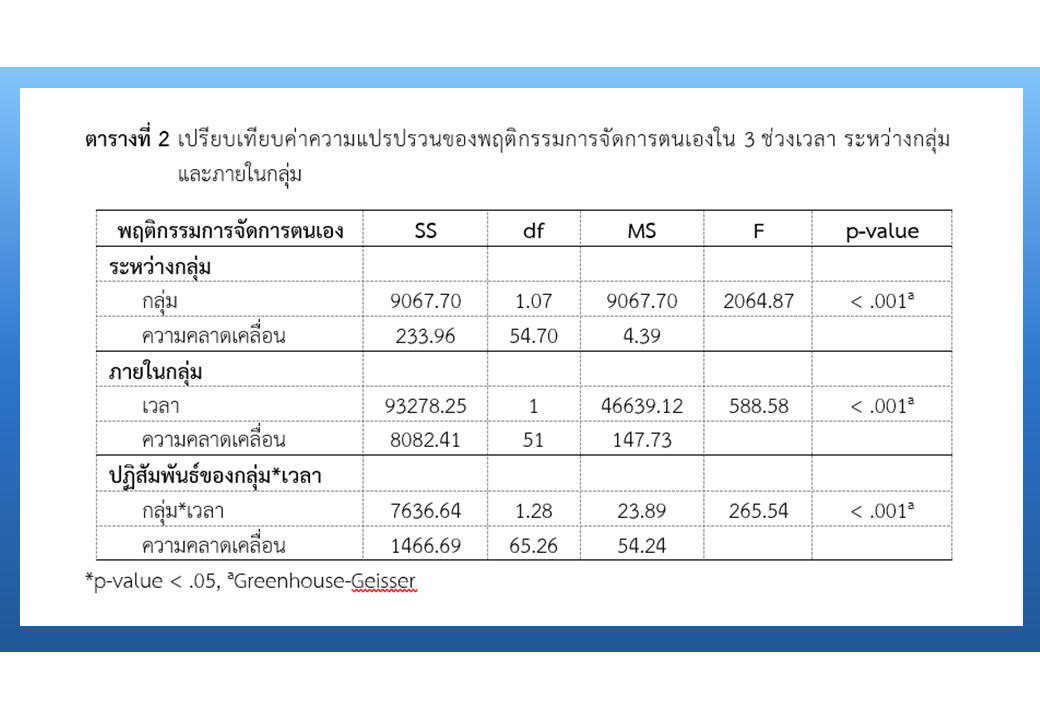
การวิจัยกึ่งทดลองแบบ 2 กลุ่ม วัดก่อน - หลัง และติดตามผลการทดลอง มีวัตถุประสงค์เพื่อศึกษาประสิทธิผลของโปรแกรมการจัดการตนเองร่วมกับการฝึกสติในผู้ป่วยโรคเบาหวานที่คุมไม่ได้ในกลุ่มผู้ใหญ่ อายุ 35 - 60 ปี จำนวน 52 คน แบ่งเป็นกลุ่มทดลอง และกลุ่มเปรียบเทียบ กลุ่มละ 26 คน โดยกลุ่มทดลองได้รับโปรแกรมการจัดการตนเองร่วมกับการฝึกสติ เก็บรวบรวมข้อมูลด้วยแบบสัมภาษณ์ ประกอบด้วยข้อมูลทั่วไปส่วนบุคคล การรับประทานอาหารอย่างมีสติ การรับประทานอาหารที่เหมาะสม การออกกำลังกาย ซึ่งมีค่าความเชื่อมั่น เท่ากับ .80 - .91 วิเคราะห์ข้อมูลด้วยสถิติเชิงพรรณนา และความแปรปรวนทางเดียวแบบวัดซ้ำ
ผลการวิจัย พบว่า หลังการทดลอง และระยะติดตามผล กลุ่มทดลองมีคะแนนเฉลี่ยการรับประทานอาหารอย่างมีสติ การรับประทานอาหารที่เหมาะสม และการออกกำลังกายสูงกว่าก่อนการทดลอง และสูงกว่ากลุ่มเปรียบเทียบอย่างมีนัยสำคัญทางสถิติ (p-value < .05) ส่วนค่าระดับน้ำตาลในเลือดลดลงกว่ากลุ่มเปรียบเทียบอย่างมีนัยสำคัญทางสถิติ (p-value < .05) โปรแกรมการจัดการตนเองร่วมกับการฝึกสตินี้มีส่วนช่วยในการดูแล และจัดการตนเองของผู้ป่วย จึงส่งผลให้ค่าระดับน้ำตาลในเลือดลดลง ดังนั้นการนำโปรแกรมการส่งเสริมการจัดการตนเองร่วมกับการฝึกสติไปประยุกต์ใช้ในสถานบริการพยาบาล จึงมีความจำเป็นเพื่อส่งเสริมให้ผู้ป่วยเบาหวานสามารถจัดการตนเองในการปรับเปลี่ยนพฤติกรรมได้อย่างเหมาะสม
เอกสารอ้างอิง
World Health Organization. WHO mortality database 2023 [Internet]. 2023 [cited 2023 Feb 20]. Available from: https://www.who.int/data/data-collection-tools/who-mortality-database
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Research and Clinical Practice 2022;4(3):311-21. doi: 10.1016/j.diabres.2011.10.029.
Cho NH, Shaw JE, Karuranga S, Huang Y, Da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice 2018;138:271-81. doi: 10.1016/j.diabres.2018.02.023.
Ministry of Public Health. Annual report 2018. Bangkok: Aksorn Graphic and Design Publishing House; 2018. (in Thai)
Division of Non Communicable Diseases, Ministry of Public Health. Number and death rate from 5 non-communicable diseases 2017 - 2021 [Internet]. 2023 [cited 2023 Mar 6]. Available from: http://www.thaincd.com/2016/mission/documents-detail.php?id=14480&tid=32&gid=1-020 (in Thai)
International Diabetes Federation. Diabetes atlas 2022 [Internet]. 2023 [cited 2022 Mar 26]. Available from: https://www.idf.org/aboutdiabetes/what-is-diabetes.html
Cradock KA, ÓLaighin G, Finucane FM, Gainforth HL, Quinlan LR, Ginis KA. Behaviour change techniques targeting both diet and physical activity in type 2 diabetes: a systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity 2017;14(1):18. doi: 10.1186/s12966-016-0436-0.
American Diabetes Association. Standard of medical care in diabetes 2019 Abridged for primary care providers. Clin Diabetes 2019;37(1):11-34. doi: 10.2337/cd18-0105.
Huo R, Du T, Xu Y, Xu W, Chen X, Sun K, et al. Effects of mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. European Journal of Clinical Nutrition 2015;69(11):1200-8. doi: 10.1038/ejcn.2014.243.
Liu Y, Ye W, Chen Q, Zhang Y, Kuo CH, Korivi M. Resistance exercise intensity is correlated with attenuation of HbA1c and insulin in patients with type 2 diabetes: a systematic review and meta-analysis. International Journal of Environmental Research Public Health 20197;16(1):140. doi: 10.3390/ijerph16010140.
Lakerveld J, Palmeira AL, Van Duinkerken E, Whitelock V, Peyrot M, Nouwen A. Motivation: key to a healthy lifestyle in people with diabetes? current and emerging knowledge and applications. Diabet Medicine: a Journal of the British Diabetic Association 2020;37(3):464-72. doi: 10.1111/dme.14228.
Buasri Y. Effects of self-nd family mngement progrm on dietry behvior nd blood sugr level mong persons with type 2 dibetes [Dissertation]. Chonburi: Burapha University; 2021. (in Thai)
Lalum P, Chintanawat R, Pothiban L. Impacts of an individualized lifestyle adjustment programme on glycosylated hemoglobin levels in older people with type-2 diabetes. Journal of Thailand Nursing and Midwifery Council 2021;34(1):42-58. (in Thai)
Harnlue N, Simud S, Robroojane S, Chuchuay P. The effectiveness of self-care program for type non-insulin dependent II diabetes, Det Udom district, Ubon Ratchathani province. Thai Journal of Public Health and Health Sciences 2018;1(2):20-31. (in Thai)
Duangklad K, Lapvongwatana P, Chansatitporn N. Improvement of self-management program in uncontrolled type II diabetes patients. Journal of Health and Nursing Research 2020;36(1):66-83. (in Thai)
Homchui P, Wanaratvijid C, Pratoomsoot C. Effect of self-management support for self-care behavior and blood glucose level in patients with type 2 diabetes mellitus. Boromarajonani College of Nursing, Uttaradit Journal 2019;12(1):240-54. (in Thai)
Hongsavong S. Effectiveness of a self-management program for patients with type 2 diabetes mellitus. Journal of Health Science 2019;28(3):411-17. (in Thai)
Natkamyoung W. The effect develops a self-management model in patients with uncontrolled type 2 diabetes, Banthi hospital, Lamphun province. Journal of Nursing and Public Health Research 2023;3(2):78-9. (in Thai)
Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. Journal of Behavioral Medicine 2016;39(2):201-13. doi: 10.1007/s10865-015-9692-8.
Friis AM, Johnson MH, Cutfield RG, Consedine NS. Kindness matters: a randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care 2016;39(11):1963-71. doi: 10.2337/dc16-0416.
Jon KZ. Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice 2003;10(2):144-56. doi: 10.1093/clipsy.bpg016.
Lattimore P. Mindfulness-based emotional eating awareness training: taking the emotional out of eating. Eating and Weight Disorders 2020;25(3):649-57. doi: 10.1007/s40519-019-00667-y.
Stanszus LS, Frank P, Geiger SM. Healthy eating and sustainable nutrition through mindfulness? mixed method results of a controlled intervention study. Appetite 2019;141:104325. doi: 10.1016/j.appet.2019.104325.
Creer T. Self-management of chronic illness. In: Boekaerts M, Pintrich PR, Zeidner M, editors. Handbook of self-regulation 2020; California: Academic; 2000. p.601-29.
Framson C, Kristal AR, Schenk JM, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. Journal of the American Dietetic Association 2009;109(8):1439-44. doi: 10.1016/j.jada.2009.05.006.
Sukchaisong N, Pichayapinyo P, Lagampan S, Saslow LR, Aikens JE. Effectiveness of the mindfulness-based diabetes self- and family management support program among adults with uncontrolled diabetes: a randomized controlled trial. Pacific Rim International Journal of Nursing Research 2022;26(3):517-32.
Kiernan M, Schoffman DE, Lee K, Brown SD, Fair JM, Perri MG, et al. The stanford leisure-time activity categorical item (L-Cat): a single categorical item sensitive to physical activity changes in overweight/obese women. International Journal Obesity 2013;37(12):1597-602. doi: 10.1038/ijo.2013.36.
Medina WL, Wilson D, De Salvo V, Vannucchi B, De Souza ÉL, Lucena L, et al. Effects of mindfulness on diabetes mellitus: rationale and overview. Current Diabetes Reviews 2017;13(2):141-7. doi: 10.2174/1573399812666160607074817.
Kian AA, Vahdani B, Noorbala AA, Nejatisafa A, Arbabi M, Zenoozian S, et al. The impact of mindfulness-based stress reduction on emotional wellbeing and glycemic control of patients with type 2 diabetes mellitus. Journal of Diabetes Research 2018;10:1986820. doi: 10.1155/2018/1986820.
Dinardo M, Greco C, Phares AD, Beyer NM, Youk AO, Obrosky DS, et al. Effects of an integrated mindfulness intervention for veterans with diabetes distress: a randomized controlled trial. BMJ Open Diabetes Research and Care 2022;10(2):1-11. doi: 10.1136/bmjdrc-2021-002631.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















