ผลของโปรแกรมป้องกันการเกิดแผลกดทับในผู้ป่วยได้รับการผ่าตัดกระดูกสันหลัง
บทคัดย่อ
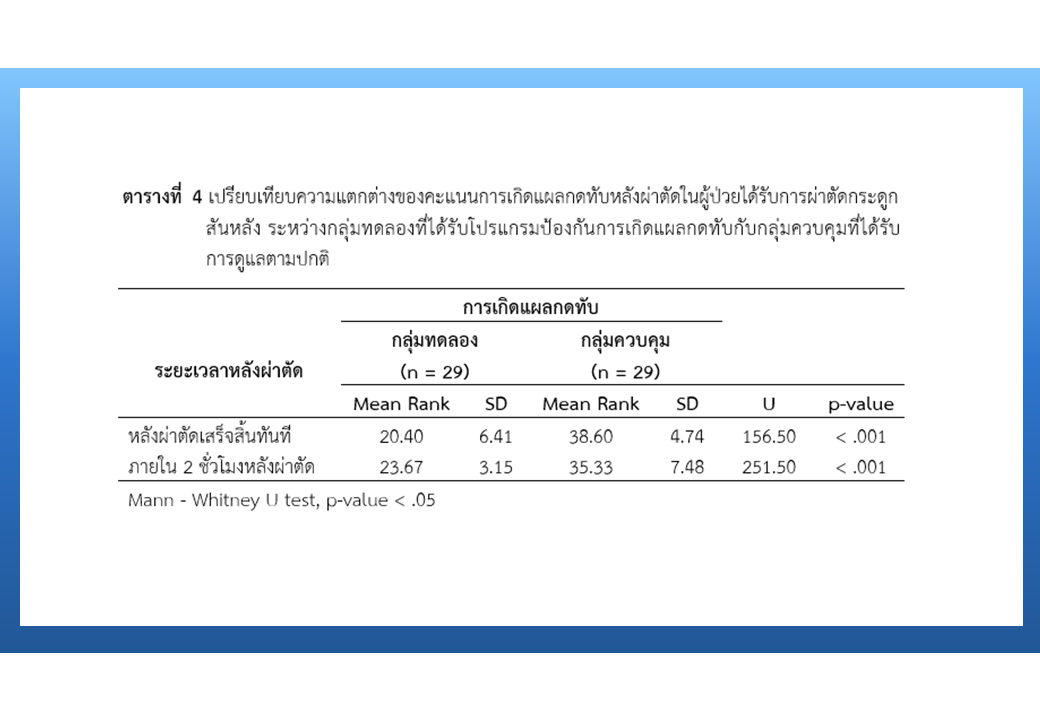
การวิจัยกึ่งทดลองแบบสองกลุ่มวัดผลก่อนและหลัง วัตถุประสงค์เพื่อศึกษาเปรียบเทียบการเกิดแผลกดทับในผู้ป่วยที่ได้รับการผ่าตัดกระดูกสันหลัง ระหว่างกลุ่มที่ได้รับโปรแกรมป้องกันการเกิดแผลกดทับกับกลุ่มที่ได้รับการดูแลตามปกติ โดยศึกษาผู้ป่วยที่มีอายุตั้งแต่ 18 ปีขึ้นไป คัดเลือกแบบเฉพาะเจาะจงจำนวน 58 คน แบ่งเป็นกลุ่มควบคุม และกลุ่มทดลองจำนวนเท่ากัน กลุ่มทดลองได้รับโปรแกรมป้องกันการเกิดแผลกดทับ กลุ่มควบคุมได้รับการพยาบาลตามปกติ ประเมินการเกิดแผลกดทับโดยใช้เครื่องมือ the Bates-Jensen wound assessment tool (BWAT) ได้ค่าดัชนีความตรงตามเนื้อหา เท่ากับ 1.00 และค่าความเชื่อมั่นเท่ากับ .98 วิเคราะห์ข้อมูลด้วยสถิติเชิงพรรณนา สถิติไคสแควร์ สถิติฟิชเชอร์ และสถิติแมน-วิทนีย์ ยู
ผลการศึกษา พบว่า กลุ่มทดลองเกิดแผลกดทับต่ำกว่ากลุ่มควบคุมอย่างมีนัยสำคัญทางสถิติที่ระดับ .001 ทั้งหลังผ่าตัดเสร็จทันที และภายใน 2 ชั่วโมงหลังผ่าตัด จากผลการศึกษานี้ แสดงให้เห็นว่าโปรแกรมป้องกันการเกิดแผลกดทับในผู้ป่วยได้รับการผ่าตัดกระดูกสันหลังสามารถลดการเกิดแผลกดทับได้ ดังนั้น โปรแกรมนี้สามารถนำไปประยุกต์ใช้ป้องกันการเกิดแผลกดทับในผู้ป่วยได้รับการผ่าตัดกระดูกสันหลังที่ไม่มีข้อจำกัดของภาวะบาดเจ็บที่กระดูกสันหลังส่วนคอ และไม่มีการมีใช้เครื่องมือยึดตรึงกะโหลกศีรษะระหว่างผ่าตัด
เอกสารอ้างอิง
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. Journal of Wound Ostomy and Continence Nursing 2016;43(6):585-97 doi: 10.1097/WON.0000000000000281.
Furuno Y, Sasajima H, Goto Y, Taniyama I, Aita K, Owada K, et al. Strategies to prevent positioning-related complications associated with the lateral suboccipital approach. Journal of Neurological Surgery 2014;75(1):35-40. doi: 10.1055/s-0033-1353366.
Srinopkun P, Wutthitham N, Jaiprommeung S. The effectiveness of nursing program “rubber bed sheet innovation for pressure sore prevention” in patients with pressure sore risk. Nursing Journal 2021;48(4):294-307. (in Thai)
Whitty JA, Mclnnes E, Bucknall T, Webster J, Gillespie BM, Banks M, et al. The cost-effectiveness of a patient centred pressure ulcer prevention care bundle: findings from the INTACT cluster randomised trial. International Journal of Nursing Studies 2017;75:35-42. doi: 10.1016/j.ijnurstu.2017.06.014.
AORN. Guidelines for perioperative practice 2018. Denver: Association of PeriOperative Registered Nurses (AORN); 2018.
Capasso V, Cox J, Cuddigan J, Delmore B, Tescher A. Pressure injury prevention - PIP tips for prone positioning [Internet]. 2020 [cited 2022 Jan 15]. Available from: https://cdn.ymaws.com/npiap.com/resource/resmgr/press_releases/NPIAP_PIP_Tips_for_Proning.pdf
Nasiri E, Mollaei A, Birami M, Lotfi M, Rafiei MH. The risk of surgery-related pressure ulcer in diabetics: a systematic review and meta-analysis. Annals of Medicine and Surgery 2021;65:102336. doi: 10.1016/j.amsu.2021.102336.
Oray M, Samra KA, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opinion on Drug Safety 2016;15(4):457-65. doi: 10.1517/14740338.2016.1140743.
Gao L, Yang L, Li X, Chen J, Du J, Yang H. Risk factors for intraoperative pressure ulcers in surgical patients. International Journal Clinical Experimental Medicine 2018;11(7):7429-35.
Shaw F, Chang PC, Lee JF, Kung HY, Tung TH. Incidence and predicted risk factors of pressure ulcers in surgical patients: experience at a medical center in Taipei, Taiwan. BioMed Research International 2014:1-9. doi: 10.1155/2014/728539.
Emery SE, Daffner SD, France JC, Ellison M, Grose BW, Hobbs GR, et al. Effect of headposition on intraocular pressure during lumbar spine fusion: a randomized, prospective study. The Journal of Bone and Joint Surgery 2015;97(22):1817-23. doi: 10.2106/JBJS.O.00091.
Goodwin CR, Recinos PF, Omeis I, Momin EN, Witham TF, Bydon A, et al. Prevention of facial pressure ulcers using the mayfield clamp for sacral tumor resection. Journal of Neurosurgery: Spine 2011;14:85-7. doi: 10.3171/2010.9.SPINE09516.
Haleem S, Mihai R, Rothenfluh DA, Reynolds J. Preventing iatrogenic facial pressure ulcers during spinal surgery: prospective trial using a novel method and review of literature. International Wound Journal 2020;17(5):1391-5. doi: 10.1111/iwj.13402.
Chui J, Craen RA. An update on the prone position: continuing professional development. Canadian Journal of Anesthesia 2016;63(6):737-67. doi 10.1007/s12630-016-0634-x.
Makhsous M, Priebe M, Bankard J, Rowles R, Zeigler M, Chen D, et al. Measuring tissue perfusion during pressure relief maneuvers: insights into preventing pressure ulcers. The Journal of Spinal Cord Medicine 2007;30(5):497-507. doi: 10.1177/1099800410392772.
Coleman S, Nixon J, Keen J, Wilson L, McGinnis E, Dealey C, et al. A new pressure ulcer conceptual framework. Journal of Advanced Nursing 2014;70(10):2222-34. doi: 10.1111/jan.12405.
Wu T, Wang ST, Lin PC, Liu CL, Chao YFC. Effects of using a high-density foam pad versus a viscoelastic polymer pad on the incidence of pressure ulcer development during spinal surgery. Biological Research for Nursing 2011;13(4):419-24. doi: 10.1177/1099800410392772.
Bates-Jensen BM, Vredevoe DL, Brecht ML. Validity and reliability of the pressure sore status tool. Decubitus 1992;5(6):20-8.
Neuroscience Institute. Nursing guidelines for brain surgery patients for nurse anesthetists posture for brain surgery patients. Bangkok: Institute of Neurology, Department of Medical Services, Ministry of Public Health; 2014. (in Thai)
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















