ปัจจัยทำนายการเกิดภาวะแทรกซ้อนระยะ 7 วันหลังผ่าตัด ในผู้ป่วยที่ได้รับการผ่าตัดเนื้องอกสมอง
คำสำคัญ:
ดัชนีมวลกาย, เนื้องอกสมอง, ระยะเวลาระงับความรู้สึก, ความเปราะบาง, ภาวะแทรกซ้อนหลังผ่าตัดบทคัดย่อ
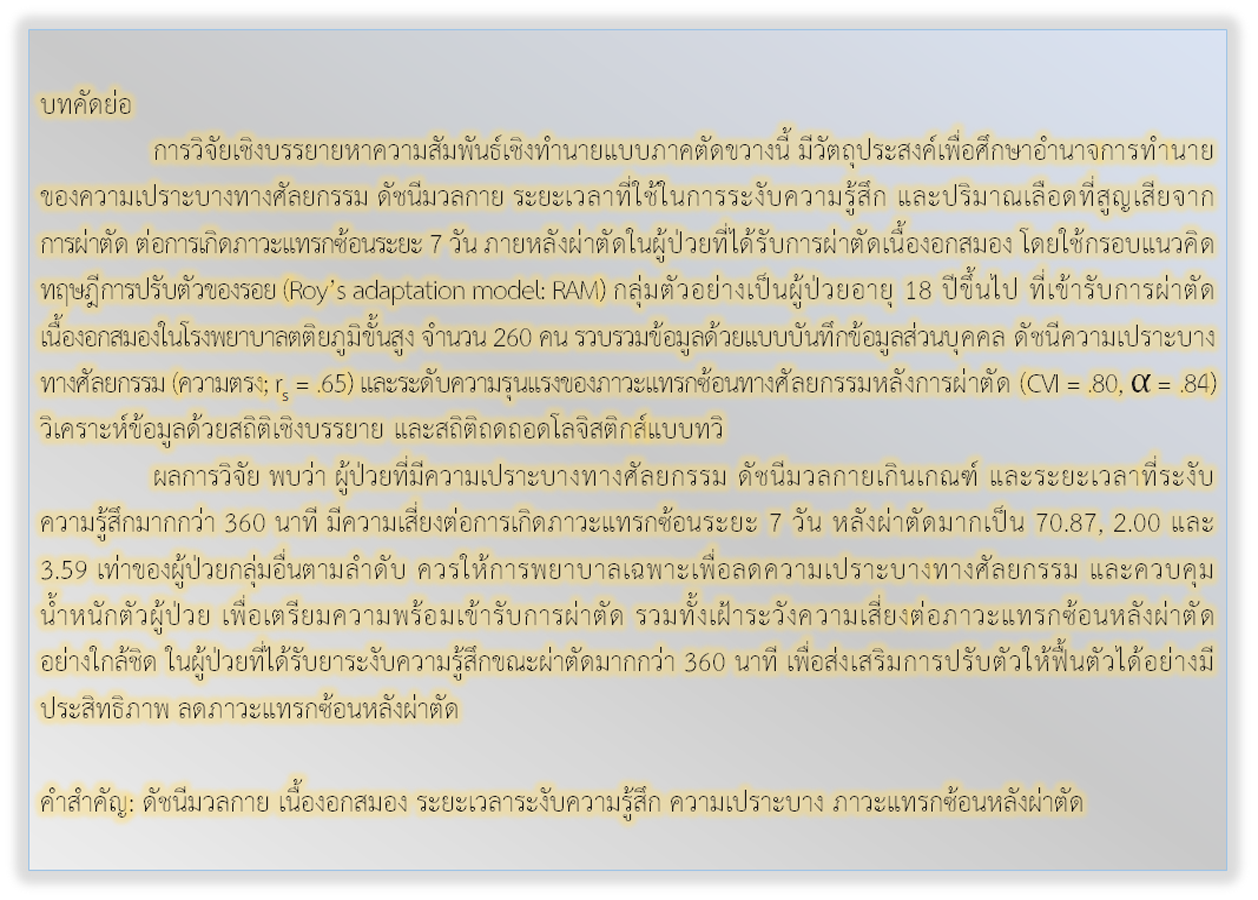
การวิจัยเชิงบรรยายหาความสัมพันธ์เชิงทำนายแบบภาคตัดขวางนี้ มีวัตถุประสงค์เพื่อศึกษาอำนาจการทำนายของความเปราะบางทางศัลยกรรม ดัชนีมวลกาย ระยะเวลาที่ใช้ในการระงับความรู้สึก และปริมาณเลือดที่สูญเสียจากการผ่าตัด ต่อการเกิดภาวะแทรกซ้อนระยะ 7 วัน ภายหลังผ่าตัดในผู้ป่วยที่ได้รับการผ่าตัดเนื้องอกสมอง โดยใช้กรอบแนวคิดทฤษฎีการปรับตัวของรอย (Roy’s adaptation model: RAM) กลุ่มตัวอย่างเป็นผู้ป่วยอายุ 18 ปีขึ้นไป ที่เข้ารับการผ่าตัดเนื้องอกสมองในโรงพยาบาลตติยภูมิขั้นสูง จำนวน 260 คน รวบรวมข้อมูลด้วยแบบบันทึกข้อมูลส่วนบุคคล ดัชนีความเปราะบางทางศัลยกรรม (ความตรง; rs = .65) และระดับความรุนแรงของภาวะแทรกซ้อนทางศัลยกรรมหลังการผ่าตัด (CVI = .80, = .84) วิเคราะห์ข้อมูลด้วยสถิติเชิงบรรยาย และสถิติถดถอดโลจิสติกส์แบบทวิ
ผลการวิจัย พบว่า ผู้ป่วยที่มีความเปราะบางทางศัลยกรรม ดัชนีมวลกายเกินเกณฑ์ และระยะเวลาที่ระงับความรู้สึกมากกว่า 360 นาที มีความเสี่ยงต่อการเกิดภาวะแทรกซ้อนระยะ 7 วัน หลังผ่าตัดมากเป็น 70.87, 2.00 และ 3.59 เท่าของผู้ป่วยกลุ่มอื่นตามลำดับ ควรให้การพยาบาลเฉพาะเพื่อลดความเปราะบางทางศัลยกรรม และควบคุมน้ำหนักตัวผู้ป่วย เพื่อเตรียมความพร้อมเข้ารับการผ่าตัด รวมทั้งเฝ้าระวังความเสี่ยงต่อภาวะแทรกซ้อนหลังผ่าตัดอย่างใกล้ชิด ในผู้ป่วยที่ได้รับยาระงับความรู้สึกขณะผ่าตัดมากกว่า 360 นาที เพื่อส่งเสริมการปรับตัวให้ฟื้นตัวได้อย่างมีประสิทธิภาพ ลดภาวะแทรกซ้อนหลังผ่าตัด
เอกสารอ้างอิง
Lapointe S, Perry A, Butowski NA. Primary brain tumours in adults. The Lancet 2018;392(10145):432-46.
Miller KD, Ostrom QT, Kruchko C, Patil N, Tihan T, Cioffi G, et al. Brain and other central nervous system tumor statistics, 2021. CA: A Cancer Journal for Clinicians 2021;71(5):381-406.
Veerasarn K, Yuthagovit S, Chailorrat A. Prevalence of brain tumor in Thailand from 2005 to 2014: data from the National Health Security Office. Journal of the Medical Association of Thailand 2016;99 Suppl 3:S62-73.
Roy SC. The Roy adaptation model. 3rd ed. Upper Saddle River, N.J: Pearson Education; 2009.
Lopes ROP, Braga DV, Castro J, Nogueira CSC, Silva R, Brandão MAG, et al. Complications in immediate postoperative recovery from elective cardiac surgery: a cross-sectional study based on Roy’s theory. Revista de Enfermagem Referencia 2019;22:23-32.
Viken HH, Iversen IA, Jakola A, Sagberg LM, Solheim O. When are complications after brain tumor surgery detected?. World Neurosurgery 2018;112:e702-10.
Senders JT, Muskens IS, Cote DJ, Goldhaber NH, Dawood HY, Gormley WB, et al. Thirty-day outcomes after craniotomy for primary malignant brain tumors: a national surgical quality improvement program analysis. Clinical Neurosurgery 2018;83(6):1249-59.
Lekan DA, Collins SK, Hayajneh AA. Definitions of frailty in qualitative research: a qualitative systematic review. Journal of Aging Research 2021;2021:6285058.
Cloney M, D'Amico R, Lebovic J, Nazarian M, Zacharia BE, Sisti MB, et al. Frailty in geriatric glioblastoma patients: a predictor of operative morbidity and outcome. World Neurosurgery 2016;89:362-7.
Castle-Kirszbaum MD, Tee JW, Chan P, Hunn MK. Obesity in neurosurgery: a narrative review of the literature. World Neurosurgery 2017;106:790-805.
Khemthong U, Chayaput P, Chanruangvanich W, Chuthapisith S. Influence of degrees of pain, type of food and oral health on post-operative oral cancer patients’ consumption of food. Thai Journal of Nursing Council 2015;30(2):60-74. (in Thai)
Cevasco M, Ashley S, Cooper Z. Physiologic response to surgery. In: McKean SC, Ross JJ, Dressler DD, Brotman DJ, Ginsberg JS, editors. Principles and practice of hospital medicine. New York: The McGraw-Hill Companies; 2012. p. 291-8.
Misal US, Joshi SA, Shaikh MM. Delayed recovery from anesthesia: a postgraduate educational review. Anesthesia: Essays and Researches 2016;10(2):164-72.
Maday KR, Hurt JB, Harrelson P, Porterfield J. Evaluating postoperative fever. Journal of the American Academy of Physician Assistants 2016;29(10):23-8.
McKenzie ME, Mastracci TM, Bhandari M, Mundi R, Rizoli SB, Nascimento BA, et al. Operative blood loss, blood transfusion and 30-day mortality in older patients after major noncardiac surgery. Canadian Journal of Surgery 2012;55(6):426-8.
Roy C, Bakan G, Li Z, Nguyen TH. Coping measurement: creating short form of coping and adaptation processing scale using item response theory and patients dealing with chronic and acute health conditions. Applied Nursing Research 2016;32:73-9.
Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. Journal of Surgical Research 2013;183(1):104-10.
Dasenbrock HH, Chavakula V, Gormley WB, Claus EB, Smith TR, Dunn IF, et al. Body habitus, serum albumin, and the outcomes after craniotomy for tumor: a national surgical quality improvement program analysis. Journal of Neurosurgery 2017;126(3):677-89.
Lemeshow S, Hosmer DW, Klar J, Lwanga SK. Adequacy of sample size in health studies. Chichester: Wiley; 1990.
Dindo D. The Clavien-Dindo classification of surgical complications. In: Cuesta MA, Bonjer HJ, editors. Treatment of postoperative complications after digestive surgery. London, United Kingdom: Springer; 2014. p. 13-7.
Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. The Journals of Gerontology: Series A 2007;62(7):738-43.
Youngerman BE, Bruce JN, Neugut AI, Hershman DL, Wright JD, Yang J. The modified frailty index and 30-day adverse events in oncologic neurosurgery. Journal of Neuro-Oncology 2018;136(1):197-206.
Gray JR, Grove SK. Understanding nursing research : building an evidence-based practice. 7th ed. St. Louis, Missouri: Elsevier Saunders; 2019.
Rattanamongkol C, Sindhu S, Toskulkao T, Iramaneerat C. Factors related to the severity of postoperative complications in patients with primary gastrointestinal (stomach, liver, bile duct, colon, and rectum) cancer. Thai Journal of Nursing Council 2016;31(3):97-109. (in Thai)
Lang LH, Parekh K, Tsui BYK, Maze M. Perioperative management of the obese surgical patient. British Medical Bulletin 2017;124(1):135-55.
Muscogiuri G, Pugliese G, Laudisio D, Castellucci B, Barrea L, Savastano S, et al. The impact of obesity on immune response to infection: plausible mechanisms and outcomes. Obesity Reviews 2021;22(6):e13216.
Golebiowski A, Drewes C, Gulati S, Jakola AS, Solheim O. Is duration of surgery a risk factor for extracranial complications and surgical site infections after intracranial tumor operations?. Acta Neurochirurgica 2015;157(2):235-40.
Rajagopalan V, Chouhan RS, Pandia MP, Lamsal R, Rath GP. Effect of intraoperative blood loss on perioperative complications and neurological outcome in adult patients undergoing elective brain tumor surgery. Journal of Neurosciences in Rural Practice 2019;10(4):631-40.
Wu WC, Trivedi A, Friedmann PD, Uttley G, Mor V, Poses RM, et al. Association between hospital intraoperative blood transfusion practices for surgical blood loss and hospital surgical mortality rates. Annals of Surgery 2012;255(4):708-14.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2022 วารสารเกื้อการุณย์

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
















