Association between sensory processing patterns and stress among communitydwelling people with metabolic syndrome
Main Article Content
Abstract
Background: Stress is a risk factor for metabolic syndrome (MetS). High and low sensory stimulation can trigger high stress, but no research exists on the relationship between sensory processing patterns and stress among people with MetS.
Objective: This study examined the association between sensory processing patterns and stress.
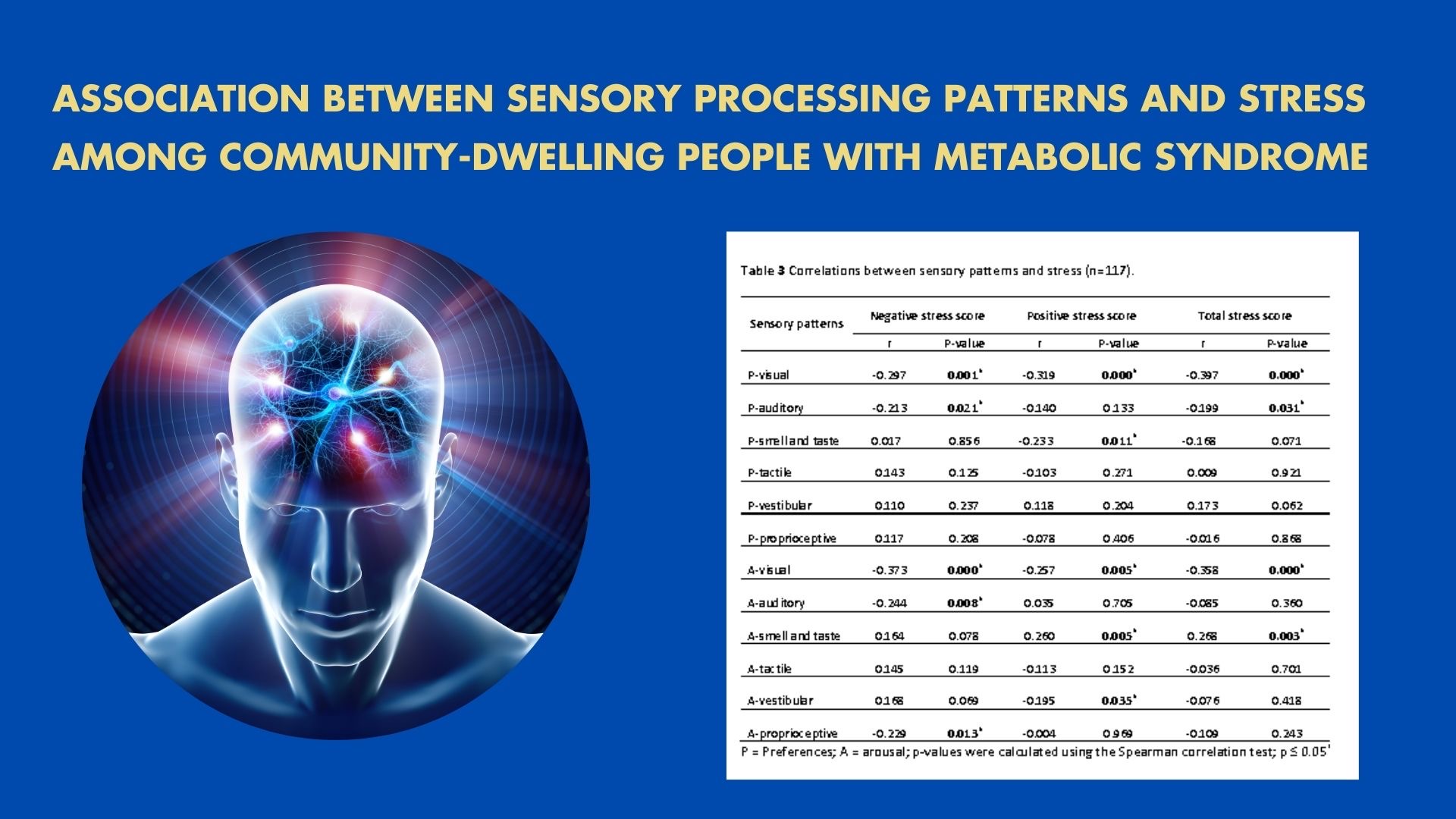
Materials and methods: A total of 117 people with MetS in the Nam Phrea subdistrict, Hang-Dong District, Chiang-Mai Province, Thailand, aged 35-85, completed the Thai Sensory Patterns Assessment-Adult Version (TSPA) and the Thai Stress Test (TST-24). Demographic and metabolic variable information was gathered. Descriptive statistics were used to summarize the demographic characteristics and stress. Spearman’s correlation and regression analysis examined the associations between the sensory processing patterns in each sensory modality and stress scores.
Results: A total stress score was significantly correlated with preferences in visual and auditory senses, as well as with arousal levels in visual and smell-taste senses (r =-0.397, -0.199, -0.358, 0.268, and p<0.05). Regression analysis revealed that stress can be predicted by preferences and arousal levels in visual and smell-taste senses (R2 =0.156, 0.039, 0.174, and 0.050, respectively; p<0.05).
Conclusion: The results suggest that sensory processing patterns might associated with stress, which is a predictor of MetS. Health professionals can utilize acquired knowledge to implement sensory-based interventions for individuals with MetS to address their stress issues.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome. Circulation. 2009; 120(16): 1640-5. doi: 10.1161/CIRCULATIONAHA.109.192644.
O’Neill S, O’Driscoll L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015; 16(1): 1-12. doi: 10.1111/obr.12229.
Guembe MJ, Fernandez-Lazaro CI, Sayon-Orea C, Toledo E, Moreno-Iribas C. Risk for cardiovascular disease associated with metabolic syndrome and its components: A 13-year prospective study in the RIVANA cohort. Cardiovasc Diabetol. 2020; 19(1): 195. doi: 10.1186/s12933-020-01166-6.
Ngoc HN, Kriengsinyos W, Rojroongwasinkul N, Aekplakorn W. Prevalence of Metabolic Syndrome and Its Prediction by Simple Adiposity Indices in Thai Adults. J Health Sci Med Res. 2021; 39(4): 13. doi: 10.31584/jhsmr.2021791.
Li X, Zhai Y, Zhao J, He H, Li Y, Liu Y, et al. Impact of Metabolic Syndrome and It’s Components on Prognosis in Patients With Cardiovascular Diseases: A Meta-Analysis. Front Cardiovasc Med. 2021; 8: 1-13. doi: 10.3389/fcvm.2021.704145.
Li Y, Sun Y, Wu H, Yang P, Huang X, Zhang L, et al. Metabolic syndromes increase significantly with the accumulation of bad dietary habits. J Nutr Health Aging. 2024; 28(2): doi: 100017. 10.1016/j.jnha.2023.100017.
Lemes IR, Sui X, Fernandes RA, Blair SN, Turi-Lynch BC, Codogno JS, et al. Association of sedentary behavior and metabolic syndrome. Public Health. 2019; 167: 96-102. doi: 10.1016/j.puhe.2018.11.007.
Yeo Y, Cho IY, Sim MS, Song HG, Song Y-M. Relationship Between Daily Sedentary Behaviors and Metabolic Syndrome in Middle-Aged Adults: Results from a Health Survey in Taean-Gun, Republic of Korea. Metab Syndr Relat Disord. 2020; 19(1): 48-55. doi: 10.1089/met.2020.0021.
Tamashiro KL, Sakai RR, Shively CA, Karatsoreos IN, Reagan LP. Chronic stress, metabolism, and metabolic syndrome. Stress. 2011; 14(5): 468-74. doi: 10.3109/10253890.2011.606341.
Kuo WC, Bratzke LC, Oakley LD, Kuo F, Wang H, Brown RL. The association between psychological stress and metabolic syndrome: A systematic review and meta-analysis. Obes Rev. 2019; 20(11): 1651-64. doi: 10.1111/obr.12915.
Dunn W. Living sensationally: Understanding your senses. London: Jessica Kingsley; 2008.
Dunn W. The sensations of everyday life: empirical, theoretical, and pragmatic considerations. Am J Occup Ther. 2001; 55(6): 608-20.
Harrold A, Keating K, Larkin F, Setti A. The association between sensory processing and stress in the adult population: A systematic review. Applied Psychology: Health and Well-Being. 2024: 1-31. doi: 10.1111/aphw.12554
Benham G. The highly sensitive person: Stress and physical symptom reports. Pers Individ Dif. 2006; 40(7): 1433-40. doi: 10.1016/j.paid.2005.11.021.
Corbett BA, Schupp CW, Levine S, Mendoza S. Comparing cortisol, stress, and sensory sensitivity in children with autism. Autism Res. 2009; 2(1): 39-49. doi: 10.1002/aur.64.
Kongngern T. Relationship between sensory patterns and stresses of relapsed alcohol dependence clients in Suansaranroom Psychiatric Hospital, Suratthani Province [Thesis]. Faculty of Associated Medical Sciences: Chiang Mai University; 2012. [in Thai]
Chang M, Turner T, Kwee S, Shaul J, Stanbach T, Stringari J. The Effects of Sensory Processing Patterns on Perceived Stress and Sleep Quality Among College Students. Am J Occup Ther. 2019; 73(4_ Supplement_1): 7311505182p1-p1. doi: 10.5014/ajot.2019.73S1-PO7022.
van den Boogert F, Spaan P, Sizoo B, Bouman YHA, Hoogendijk WJG, Roza SJ. Sensory Processing, Perceived Stress and Burnout Symptoms in a Working Population during the COVID-19 Crisis. Int J Environ Res Public Health. 2022; 19(4): 2043. doi: 10.3390/ijerph19042043.
Engel-Yeger B, Dunn W. The Relationship between Sensory Processing Difficulties and Anxiety Level of Healthy Adults. Br J Occup Ther. 2011; 74(5): 210-6. doi: 10.4276/030802211X13046730116407.
Wu X, Zhang R, Li X, Feng T, Yan N. The moderating role of sensory processing sensitivity in the link between stress and depression: A VBM study. Neuropsychologia. 2021; 150: 107704. doi: 10.1016/j.neuropsychologia.2020.107704.
Corbett BA, Muscatello RA, Blain SD. Impact of Sensory Sensitivity on Physiological Stress Response and Novel Peer Interaction in Children with and without Autism Spectrum Disorder. Front Neurosci. 2016; 10: 278. doi: 10.3389/fnins.2016.0027.
Das UN. Metabolic syndrome pathophysiology: The role of essential fatty acids. UK: Wiley-Blackwell; 2010.
Boongerd P. Interesting topic about dementia. Dementia Association of Thailand, Newsletter. 2018; 10: 1-4.
Pomngen I, Srikhamjak T, Putthinoi S. Development of the Sensory Patterns Assessment [Thesis]. Faculty of Associated Medical Sciences, Chiang Mai University; 2020. [in Thai]
Phattharayuttawat S, Ngamthipwattana T, Sukhatungkha K. The Development of the Thai Stress Test. J Psychiatr Assoc Thailand. 2000; 45(3): 237-50 doi: 10.1.1.522.2455&rep=rep1&type =pdf.
Engel-Yeger B, Dunn W. The Relationship between Sensory Processing Difficulties and Anxiety Level of Healthy Adults. Br J Occup Ther. 2011; 74(5): 210-6. doi: 10.4276/030802211X13046730116407
Carr M, Matthews E, Williams J, Blagrove M. Testing the theory of Differential Susceptibility to nightmares: The interaction of Sensory Processing Sensitivity with the relationship of low mental wellbeing to nightmare frequency and nightmare distress. J Sleep Res. 2021; 30(3): e13200. doi: 10.1111/jsr.13200.
Lundy-Ekman L. Neuroscience: Fundamentals for rehabilitation. 4th ed. St Louis: Elsevier; 2013.
Masuo Y, Satou T, Takemoto H, Koike K. Smell and Stress Response in the Brain: Review of the Connection between Chemistry and Neuropharmacology. Molecules. 2021; 26(9). 2571. doi: 10.3390/molecules26092571.
Cox T, Mackay C. A psychological model of occupational stress: A paper presented to the medical research council. London: Mental Health in Industry; 1976.
Payne RA, Donaghy M. Payne’s handbook of relaxation techniques: A practical guide for the health care professional. New York: Elsevier; 2010.
Pagliano. The multisensory handbook. New York, NY: Taylor & Francis Group; 2012.
Horii Y, Nagai K, Nakashima T. Order of exposure to pleasant and unpleasant odors affects autonomic nervous system response. Behav Brain Res. 2013; 243: 109-17. doi: 10.1016/j.bbr.2012.12.042.
Hirasawa Y, Shirasu M, Okamoto M, Touhara K. Subjective unpleasantness of malodors induces a stress response. Psychoneuroendocrinology. 2019; 106: 206-15. doi: 10.1016/j.psyneuen.2019.03.018.
Cheon Y, Park J, Jeong BY, Park EY, Oh J-K, Yun EH, et al. Factors associated with psychological stress and distress among Korean adults: the results from Korea National Health and Nutrition Examination Survey. Scientific Reports. 2020; 10(1): 15134. doi: 10.1038/s41598-020-71789-y.