Interpretability and appropriate cut-off score of occiput-bed distance to indicate risk of hyperkyphosis in older adults
Main Article Content
Abstract
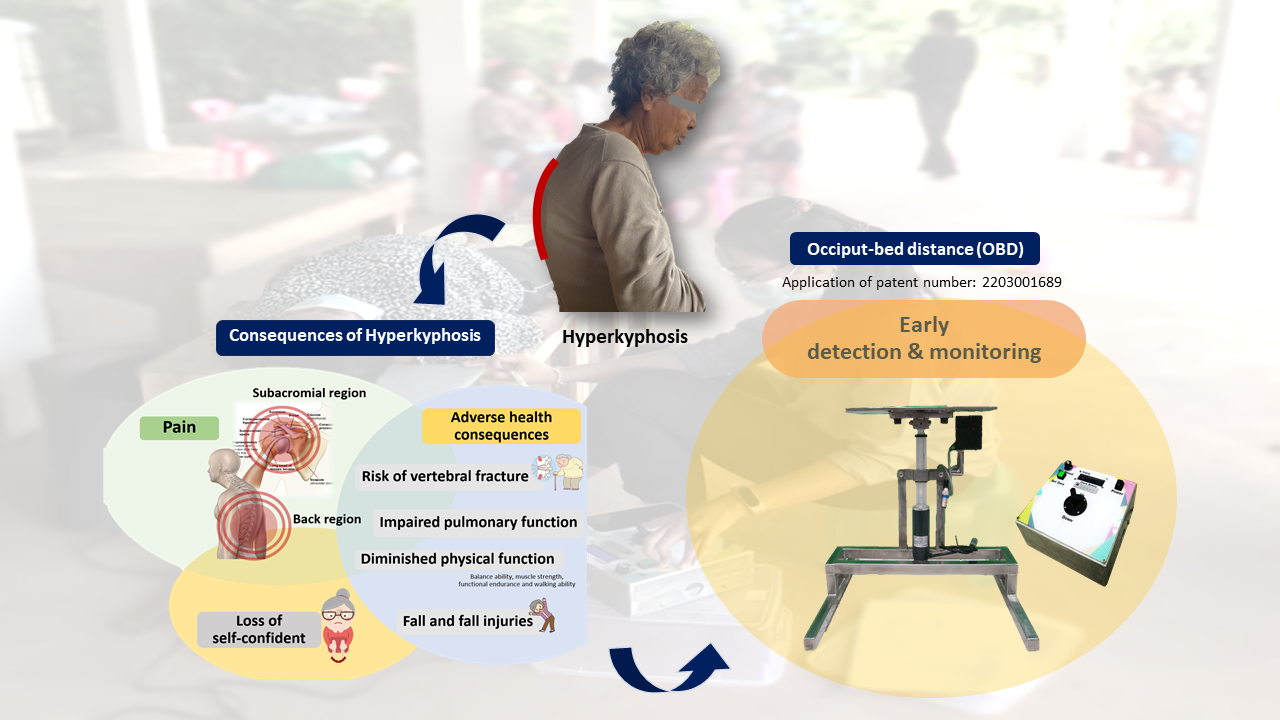
Background: Age-related hyperkyphosis has been described as a new geriatric syndrome. Therefore, early screening is critical. The occiput-bed distance (OBD) was developed as a new tool; however, there needed to be clear evidence supporting its clinical utility compared to the data from standard measurement.
Objective: To investigate the test-retest reliability and minimal detectable change (MDC) with standard measurement error (SEM). Moreover, the practical cut-off scores to determine the risk of hyperkyphosis are crucial compared to a standard Cobb’s method.
Materials and methods: This study was designed as a cross-sectional study conducted in ninety-six hyperkyphosis older adults aged at least 60 years. All participants were assessed for their hyperkyphosis using the OBD. Within seven days, they were at a hospital to complete a radiographic examination to determine the appropriate cut-off score of hyperkyphosis. Additionally, the first 30 participants were assessed for their hyperkyphosis again using the OBD to determine the interpretability.
Results: The outcomes of the OBD had excellent test-retest reliability (ICC 3,3 =0.887, p<0.001). The SEM and MDC95 values were 0.75 and 2.08 cm, respectively. In addition, the cut-off score of OBD was reported to be at least 7.40 cm (sensitivity 71.80%, specificity 73.70%, and AUC =0.734) to indicate the risk of hyperkyphosis.
Conclusion: The OBD is consistent, reliable, and has good diagnostic properties for hyperkyphosis. The findings confirm the use of OBD as a practical alternative method for early detection of hyperkyphosis in older individuals, particularly those who cannot stand for long and cannot access radiology.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Katzman WB, Harrison SL, Fink HA, Marshall LM, Orwoll E, Barrett-Connor E, et al. Physical function in older men with hyperkyphosis. J Gerontol A Biol Sci Med Sci. 2015; 70(5): 635-40. doi: 10.1093/gerona/glu213.
Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007; 147(5): 330-8. doi: 10.7326/0003-4819-147-5-200709040-00008.
Ailon T, Shaffrey CI, Lenke LG, Harrop JS, Smith JS. Progressive spinal kyphosis in the aging population. Neurosurgery. 2015; 77(Suppl 4): S164-72. doi: 10.1227/NEU.0000000000000944.
Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. J Orthop Sports Phys Ther. 2010; 40(6): 352-60. doi: 10.2519/jospt.2010.3099.
Hinman MR. Comparison of thoracic kyphosis and postural stiffness in younger and older women. J Spine. 2004; 4(4): 413-7. doi: 10.1016/j.spinee.2004.01.002.
Azadinia F, Kamyab M, Behtash H, Ganjavian M, Javaheri R. The validity and reliability of noninvasive methods for measuring kyphosis. J Spinal Disord Tech. 2014; 27: 212-8. doi: 10.1097/BSD.0b013e31829a3574
Amatachaya P, Wongsa S, Sooknuan T, Thaweewannakij T, Laophosri M, Manimanakorn N, et al. Validity and reliability of a thoracic kyphotic assessment tool measuring distance of the seventh cervical vertebra from the wall. Hong Kong Physiother J. 2016; 35: 30-6. doi: 10.1016/j.hkpj.2016.05.001.
Wongsa S, Amatachaya S. Kyphosis assessments. Arch AHS. 2014; 26(2): 105-16.
Chokphukiao P, Wiyanad A, Suwannarat P, Amatachaya S, Mato L, Wattanapan P, et al. Validity and reliability of the block method for measuring thoracic hyperkyphosis. Physiother Theory Pract. 2022; 38(13): 3037- 44. doi: 10.1080/09593985.2021.
Tran TH, Wing D, Davis A, Bergstrom J, Schousboe JT, Nichols JF, et al. Correlations among four measures of thoracic kyphosis in older adults. Osteoporos Int. 2016; 27(3): 1255-9. doi: 10.1007/s00198-015-3368-7.
Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006; 21(3): 419-23. doi: 10.1359/JBMR.051201.
Chokphukiao P, Wiyanad A, Suwannarat P, Amatachaya S, Wattanapan P, Mato L, et al. Discriminative ability of 1.7-cm block for kyphosis measurement. Proceedings of the national and international graduate research conference 2017; 2017 March 10; Pote Sarasin Building, Khon Kaen University, Thailand, 2017. Available from: https://gsbooks.gs.kku.ac.th/60/nigrc2017/pdf/MMP21.pdf.
Intaruk R, Ruangsri J, Noiphum L, Amatachaya P, Amatachaya S, Thaweewannakij T. Concurrent validity of the Occiput-Bed Distance for measuring hyperkyphosis. Thai J Phys Ther. 2023; 45(2): 135-45.
Portney LG, Watkins MP. Foundations of clinical research application to practice. 3rd Ed. Upper Saddle River: Pearson Prentice Hall; 2009.
Morrow JR, Jackson AW. How “significant” is your reliability? Res Q Exerc Sport. 1993; 64(3): 352-5. doi: 10.1080/02701367.1993.10608821.
de Oliveira TS, Candotti CT, La Torre M, Pelinson PPT, Furlanetto TS, Kutchak FM, et al. Validity and reproducibility of the measurements obtained using the flexicurve instrument to evaluate the angles of thoracic and lumbar curvatures of the spine in the sagittal plane. Rehabil Res Pract. 2012; 2012: 186156. doi: 10.1155/2012/186156.
Suwannarat P, Wattanapan P, Wiyanad A, Chokphukiao P, Wilaichit S, Amatachaya S. Reliability of novice physiotherapists for measuring Cobb angle using a digital method. Hong Kong Physiother J. 2017; 37: 34-8. doi: 10.1016/j.hkpj.2017.01.003.
Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010; 5(9): 1315-6. doi: 10.1097/JTO.0b013e3181ec173d.
de Vet HC TC, Mokkink LB, Knol DL. Measurement in Medicine. 1st Ed. The United States of America by Cambridge University Press: New York; 2011.
Siminoski K, Warshawski RS, Jen H, Lee KC. The accuracy of clinical kyphosis examination for detection of thoracic vertebral fractures: comparison of direct and indirect kyphosis measures. J Musculoskelet Neuronal Interact. 2011; 11(3): 249-56.
Wiyanad A, Chokphukiao P, Suwannarat P, Thaweewannakij T, Wattanapan P, Gaogasigam C, et al. Is the occiput-wall distance valid and reliable to determine the presence of thoracic hyperkyphosis? Musculoskelet Sci Pract. 2018; 38: 63-8. doi: 10.1016/j.msksp.2018.09.010.
Suwannarat P, Amatachaya P, Sooknuan T, Tochaeng P, Kramkrathok K, Thaweewannakij T, et al. Hyperkyphotic measures using distance from the wall: validity, reliability, and distance from the wall to indicate the risk for thoracic hyperkyphosis and vertebral fracture. Arch Osteoporos. 2018; 13(1): 25. doi: 10.1007/s11657-018-0433-9.
Lewis JS, Valentine RE. Clinical measurement of the thoracic kyphosis. A study of the intra-rater reliability in subjects with and without shoulder pain. BMC Musculoskelet Disord. 2010; 11: 39. doi: 10.1186/1471-2474-11-39.
Thaweewannakij T, Wongsa S, Kamruecha, Khaengkhan J, Wongkuanklom J, Konkamtan, et al. Validity and discriminative ability on physical impairment relating to kyphosis using 1.7-cm block. Asia Pac J Sci Technol. 2012; 17: 660-70.
Schafer R. Body Alignment, posture, and gait. 2nd Ed. Baltimore: Williams & Wilkins; 1983.