Estimation of organ-absorbed doses in patients undergoing chest and abdominal X-ray examinations using Monte Carlo-based software
Main Article Content
Abstract
Background: Medical imaging is essential for diagnosis and treatment. However, it raises long-term radiation exposure concerns for patient safety. The measurements of entrance surface air kerma (ESAK), entrance surface dose (ESD), and dose area product (DAP) have been widely used to estimate patient doses. However, these parameters cannot represent the patient’s organ-absorbed doses.
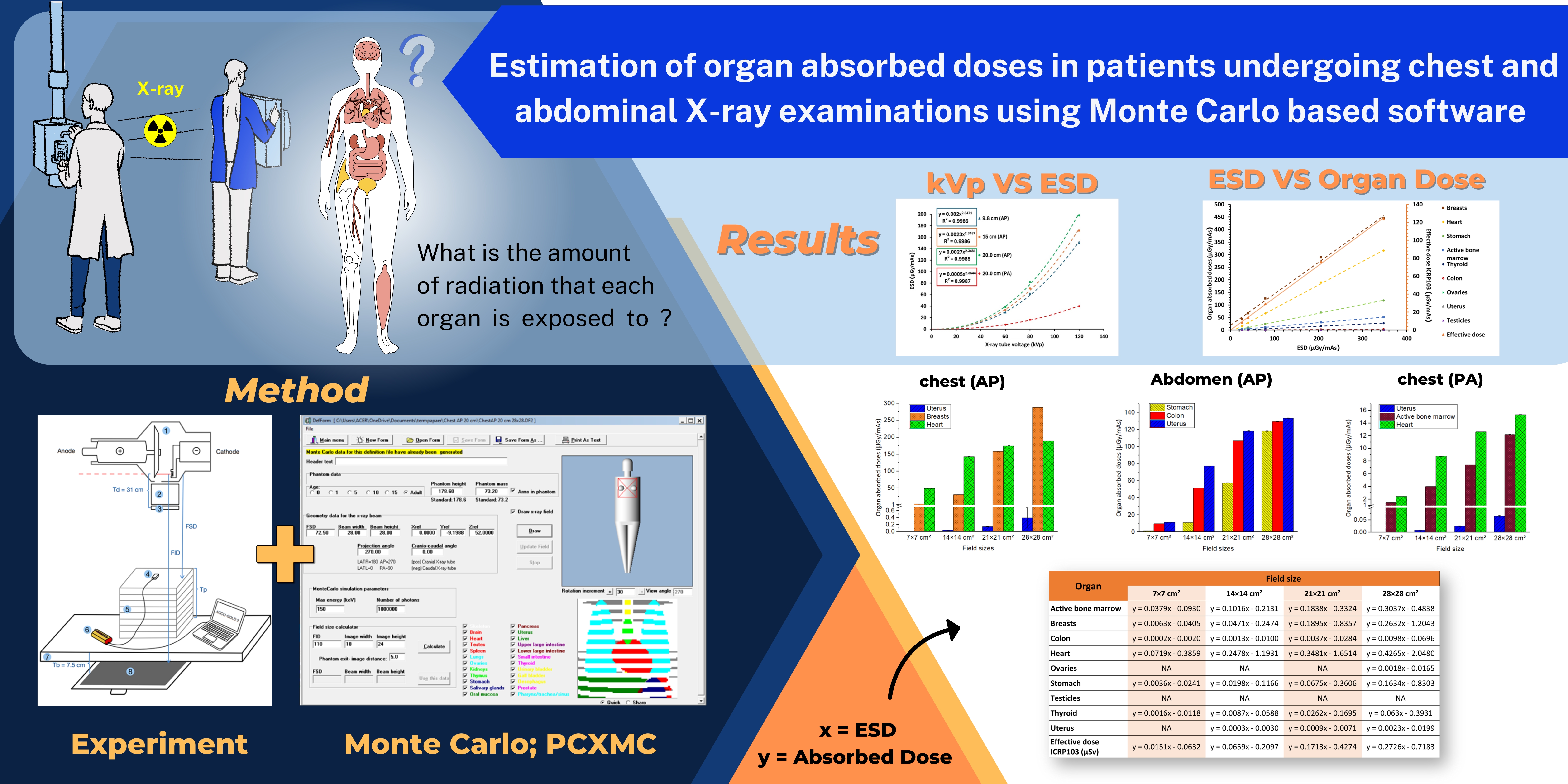
Objective: To establish a relationship between ESD and organ-absorbed doses, calculated using Monte Carlo-based software to estimate organ-absorbed doses in patients undergoing chest and abdominal X-ray examinations.
Materials and methods: The SHIMADZU RADspeed Pro X-ray machine with VacuDAP meter, Radcal, and AGMS-D+ solid-state detector with Accu-Gold software was used to measure ESD. Tissue-equivalent slab phantoms with 9.8, 15.0, and 20.0 cm thickness were used at 60, 80, and 120 kVp and 3.2 mAs. Surface field sizes varied from 7×7 cm2 to 28×28 cm2. Organ-absorbed doses were calculated using PCXMC 2.0 from STUK (Finland) using the same X-ray exposure techniques as the experiment.
Results: The X-ray tube voltage (kVp) is proportional to the ESD (µGy/mAs). This relationship can be described using a power equation. The ESD increased as the phantom thickness increased for each beam field size. A linear function was used to estimate the relationship between ESD and organ-absorbed doses. Due to their anatomical positions, which are most adjacent to the X-ray source, the breast, uterus, and heart have the highest organ-absorbed doses undergoing examinations of the chest (anteroposterior; AP), abdomen (AP), and chest (posteroanterior; PA), respectively.
Conclusion: The relationships between ESD and kVp were established as power functions, but the relationships with DAP were linear functions. The relationship between ESD and organ-absorbed doses was described using linear equations that varied with beam field size and patient thickness. This study provides a helpful method for estimating organ-absorbed and effective patient doses. This is important in assessing the risk of radiation exposure from diagnostic radiography.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Hall E, Brenner D. Cancer risks from diagnostic radiology. Br J Radiol. 2008; 81(965): 362-78. doi: 10.1259/bjr/01948454.
Dainiak N. Radiation dose and stochastic risk from exposure to medical imaging. Chest. 2013; 144(5): 1431-3. doi: 10.1378/chest.13-1064.
Matthews K, Brennan P. The application of diagnostic reference levels: General principles and an Irish perspective. Radiography. 2009; 15(2): 171-8. doi: 10.1016/j.radi.2008.03.001.
Vaño E, Miller D, Martin C, Rehani M, Kang K, Rosenstein M, et al. ICRP publication 135: Diagnostic Reference Levels in Medical Imaging. Ann ICRP. 2017; 46(1): 78-80. doi: 10.1177/0146645317717209.
Uniya S, Chaturvedi V, Sharma S, Raghuvanshi S. Estimation of entrance surface air kerma due to diagnostic X-ray examinations of adult patients in Uttarakhand, India and establishment of local diagnostic reference levels. Australas Phys Eng Sci Med. 2017; 40: 687-94. doi: 10.1007/s13246-017-0577-8.
Jibiri N, Olowookere C. Evaluation of dose-area product of common radiographic examinations towards establishing a preliminary diagnostic reference levels (PDRLs) in Southwestern Nigeria. J Appl Clin Med Phys. 2016; 17(6): 392-404. doi: 10.1120/jacmp.v17i6.6011.
Davoodi R, Eydian M, Karampour H, Nassarpour M, Rezazadeh-Farokh R, Maraei A, et al. Application of Dose Area Product (DAP) to Estimate Entrance Surface Dose (ESD) in Pediatric Chest X-Rays. Mod Health Sci. 2020; 3(2): 1-6. doi: 10.30560/mhs.v3n2p1.
Kaushik C, Sandhu IS, Srivastava AK, Chitkara M. Estimation of entrance surface air kerma in digital radiographic examinations. Radiat Prot Dosimetry. 2021; 193(1): 16-23. doi: 10.1093/rpd/ncab018.
Jamal N, Sayed I, Syed W. Estimation of organ-absorbed dose in pediatric chest X-ray examination: A phantom study. Radiat Phys Chem. 2020; 166: 108472. doi: 10.1016/j.radphyschem.2019.108472.
Ibrahim I, Hassan F, Abdulkareem N. Effective Dose Calculation for Patients Undergoing X-ray Examinations in Erbil Hospitals. Int Electron Med. 2020; 9(3): 121- 3. doi: 10.34172/IEJM.2020.22.
Alonso M, Barriuso T, Castañeda M, Díaz-Caneja N, Gutiérrez I, Sarmiento J, et al. Monte carlo estimation of absorbed dose to organs in diagnostic radiology. Health Phys. 1999; 76(4): 388-92. doi: 10.1097/00004032-199904000-00006.
Massoud E, Diab H. Optimization of Dose to Patient in Diagnostic Radiology Using Monte Carlo Method. J Cell Sci Ther. 2014;5(1). doi: 10.4172/2157-7013.1000155.
Tapiovaara M, Siiskonen T. PCXMC A Monte Carlo program for calculating patient doses in medical x-ray examinations 2ed. Findland2008. 49 p.
ICRP. Annals of the ICRP PUBLICATION 103 “The 2007 Recommendations of the International Commission on Radiological Protection”. Polestar Wheatons Ltd, Exeter, UK: International Commission on Radiological Protection, 2007. 332 p. doi: 10.1016/j.icrp.2007.10.003.
Markku Tapiovaara TS. PCXMC 2.0 User’s Guide. Helsinki, FINLAND: STUK • SÄTEILYTURVAKE; 2008.
Kawaura C, Aoyama T, Koyama S, Achiwa M, Mori M. Organ and effective dose evaluation in diagnostic radiology based on in-phantom dose measurements with novel photodiode-dosimeters. Radiat Prot Dosimetry. 2005; 118(4): 421-30. doi: 10.1093/rpd/nci372.
Kumaresan M, Kumar R, Biju K, Choubey A, Kantharia S. Measurement of entrance skin dose and estimation of organ dose during pediatric chest radigraphy. Health Phys. 2011; 100(6): 654-7. doi: 10.1093/rpd/nci372.
Ma H, Elbakri I, Reed M. Estimation of organ and effective doses from newborn radiography of the chest and abdomen. Radiat Prot Dosimetry. 2013; 156(2): 160-7. doi: 10.1093/rpd/nct050.
Dolenc L, Petrinjak B, Mekiš N, Škrk D. The impact of body mass index on patient radiation dose in general radiography. J Radiol Prot. 2022;42(4):041505. doi: 10.1088/1361-6498/ac9f1f.
Yanch JC, Behrman RH, Hendricks MJ, McCall JH. Increased radiation dose to overweight and obese patients from radiographic examinations. Radiology. 2009; 252(1): 128-39. doi: 10.1148/radiol.2521080141.
Prapan A, Chuprempri K, Fong-in P, Kheawtubtim P, Rattanarungruangchai N, Pengpan T. Radiation dose and image quality optimization in lumbar spine digital radiography for overweight and obese patients: Phantom study. J Assoc Med Sci. 2024; 57(3): 1-7. doi: 10.12982/JAMS.2024.041.