Factors associated with musculoskeletal pain in ambulatory individuals with spinal cord injury
Main Article Content
Abstract
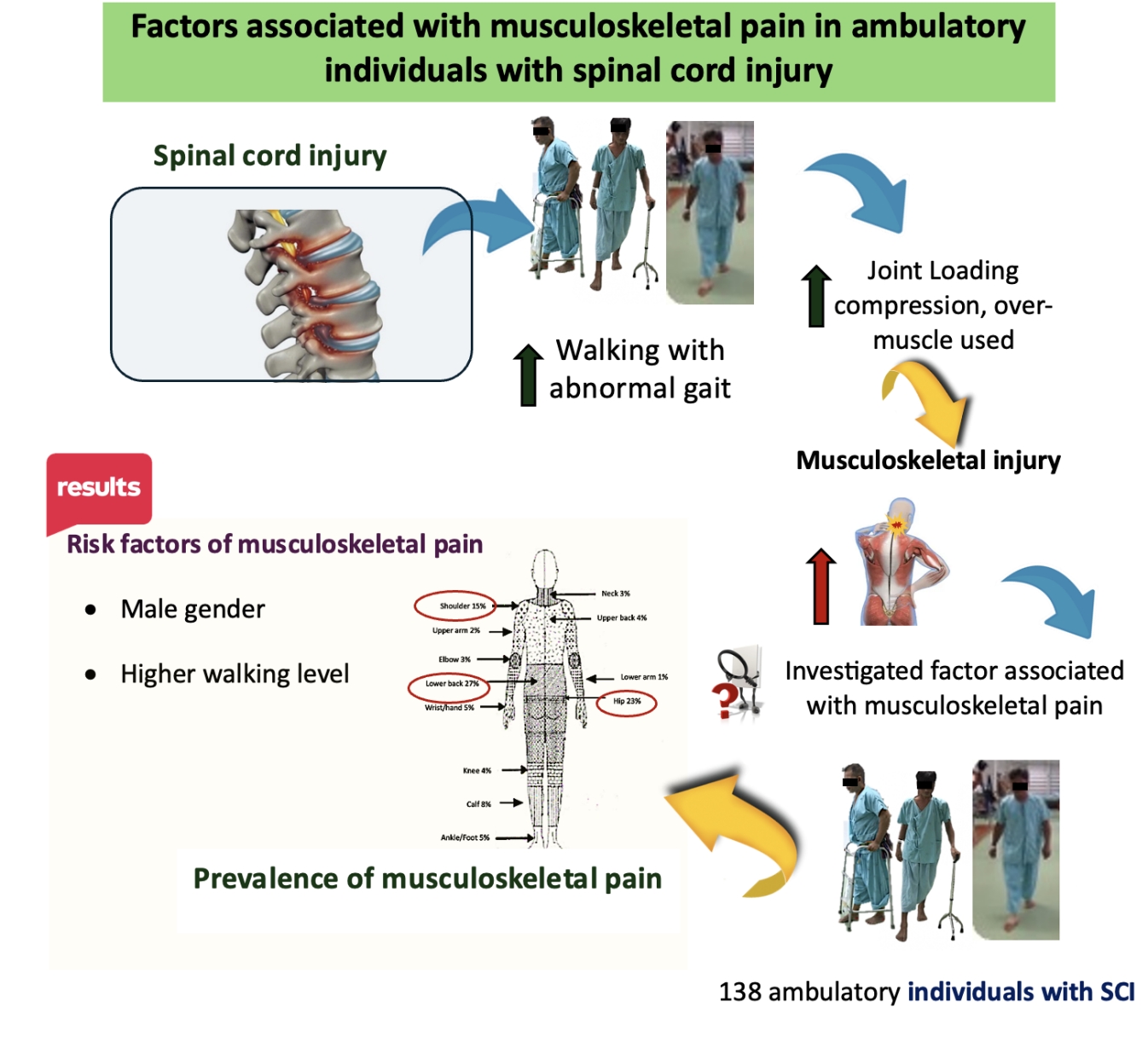
Background: Such myriad consequences of musculoskeletal pain were common and distorted the level of functioning after spinal cord injury (SCI). No known data identifies pain-related factors in ambulatory individuals with SCI.
Objective: To examine the risk factors for musculoskeletal pain in ambulatory patients with SCI.
Materials and methods: A total of 138 ambulatory participants with SCI were interviewed and evaluated for their demographics, SCI traits, levels of locomotor disability (Functional Independence Measure-Locomotor), and data on musculoskeletal pain, including area, cause, and severity of pain using a body chart diagram and Visual Analogue Scale. Then, logistic regression was used to analyze risk factors associated with musculoskeletal pain.
Results: Precisely, 55.07% of the 138 ambulatory individuals with SCI reported musculoskeletal pain. The common top three areas of pain include the lower back (27%), hip (23%) and shoulder (15%). Factors associated with musculoskeletal pain include being a man and FIM-L 6 in which males had OR=3.56 (95% CI, 1.62-7.84; p=0.002) and FIM-L 6 had OR=2.57 (95% CI, 1.08-6.10; p=0.032).
Conclusion: The present findings revealed that musculoskeletal pain is highly prevalent in ambulatory individuals with SCI. Ambulatory individuals with SCI who are males and able to walk at least 50 meters while using gait devices are most concerned about musculoskeletal pain problems.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M, et al. Spinal cord injury and aging: Challenges and recommendations for future research. Am J Phys Med Rehabil. 2012; 91: 80-93. doi: 10.1097/PHM.0b013e31821f70bc.
Zullo S, Ingravallo F, Crespi V, Cascioli M, D’Alessandro R, Gasperini M, et al. The impact of the COVID-19 pandemic on people with neurological disorders: An urgent need to enhance the health care system’s preparedness. Neurol Sci. 2021; 42(3): 799-804. doi: 10.1007/s10072-020-04984-4.
Haisma JA, van der Woude LH, Stam HJ, Bergen MP, Sluis TA, Post MW, et al. Complications following spinal cord injury: Occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. J Rehabil Med. 2007; 39: 393-8. doi: 10.2340/16501977-0067.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003; 103:249-57. doi: 10.1016/S0304-3959(02)00452-9.
Das A, Equebal A, Kumar S. Incidence of musculoskeletal pain and its impact on daily and functional activities in Indian spinal cord injury patients. Int J Physioth Res. 2013; 3: 99-106.
Hassanijirdehi M, Khak M, Afshari-Mirak S, HolakouieNaieni K, Saadat S, Taheri T, et al. Evaluation of pain and its effect on quality of life and functioning in men with spinal cord Injury. Korean J Pain. 2015; 28: 129-36. doi: 10.3344/kjp.2015.28.2.129.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: A 6-year follow-up study. Spinal Cord. 2004; 42: 513-25. doi: 10.1038/sj.sc.3101629.
Ragnarsson K. Management of pain in persons with spinal cord injury. J Spinal Cord Med. 1997; 20: 186- 99. doi:10.1080/10790268.1997.11719468.
Rintala DH, Loubser PG, Castro J, Hart KA, Fuhrer MJ. Chronic pain in a community-based sample of men with spinal cord injury: prevalence, severity, and relationship with impairment, disability, handicap, and subjective well-being. Arch Phys Med Rehabil. 1998; 79: 604-01. doi: 10.1016/s0003-9993(98)90032-6.
Kennedy P, Frankel H, Gardner B, Nuseibeh I. Factors associated with acute and chronic pain following traumatic spinal cord injuries. Spinal Cord. 1997; 35: 814-17. doi: 10.1038/sj.sc.3100569.
Tsuritani I, Honda R, Noborisaka Y, Ishida M, Ishizaki M, Yamada Y. Impact of obesity on musculoskeletal pain and difficulty of daily movements in Japanese middle-aged women. Maturitas. 2002; 42: 23-30. doi: 10.1016/s03785122(02)00025-7.
Barbetta DC, Lopes AC, Chagas FN, Soares PT, Casaro FM, Poletto MF, et al. Predictors of musculoskeletal pain in the upper extremities. Spinal Cord. 2016; 54: 145-9. doi: 10.1038/sc.2015.126.
Müller R, Brinkhof MW, Arnet U, Hinrichs T, Landmann G, Jordan X, et al. Prevalence and associated factors of pain in the Swiss spinal cord injury population. Spinal Cord. 2017; 55: 346-54. doi: 10.1038/sc.2016.157.
Phonthee S, Saengsuwan J, Siritaratiwat W, Amatachaya S. Incidence and factors associated with falls in independent ambulatory individuals with spinal cord injury: A 6-month prospective study. Phys Ther. 2012; 93: 1061-72. doi: 10.2522/ptj.20120467.
Saensook W, Phonthee S, Srisim K, Mato L, Wattanapan P, Amatachaya S. Ambulatory assistive devices and walking performance in patients with incomplete spinal cord injury. Spinal Cord. 2014; 52: 216-9. doi: 10.1038/sc.2013.120.
Behrman AL, Harkema SJ. Locomotor training after human spinal cord injury: A series of case studies. Phys Ther. 2000; 80(7): 688-700. doi:10.1093/PTJ/80.7.688.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med. 2001; 34: 547-54. doi: 10.1179/107902611X13186000420242.
Reed MD, van Nostran W. Assessing pain intensity with the visual analog scale: A plea for uniformity. J Clin Pharmacol. 2014; 54(3): 241-4. doi: 10.1002/jcph.250.
Weigl K, Forstner T. Design of paper-based visual analogue scale Items. Educ Psychol Meas. 2021 ;81(3):595-611. doi: 10.1177/0013164420952118.
Crawford B, Bouhassira D, Wong A, Dukes E. Conceptual adequacy of the neuropathic pain symptom inventory in six countries. Health Qual Life Outcomes. 2008; 6:62. doi: 10.1186/1477-7525-6-62.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011; 63: S2040-52. doi: 10.1002/acr.20543.
Kumprou M, Amatachaya P, Sooknuan T, Thaweewannakij T, Mato L, Amatachaya S. Do ambulatory patients with spinal cord injury walk symmetrically? Spinal Cord. 2017; 55: 204-7. doi: 10.1038/sc.2016.149.
Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequence. Arch Phys Med Rehabil. 2005; 86: 134-45. doi: 10.1016/j.apmr.2004.04.023.
van Drongelen S, de Groot S, Veeger HE, Angenot EL, Dallmeijer AJ, Post MW, et al. Upper extremity musculoskeletal pain during and after rehabilitation in wheelchair-using persons with a spinal cord injury. Spinal Cord. 2006; 44: 152-9. doi: 10.1038/sj.sc.3101826.
Hassan R, Kamrujjaman M. A cross-sectional study of spinal cord injury-induced musculoskeletal Pain. Curr Med Res Opin. 2019; 2(12): 367-71. doi: 10.15520/jcmro.v2i12.234.