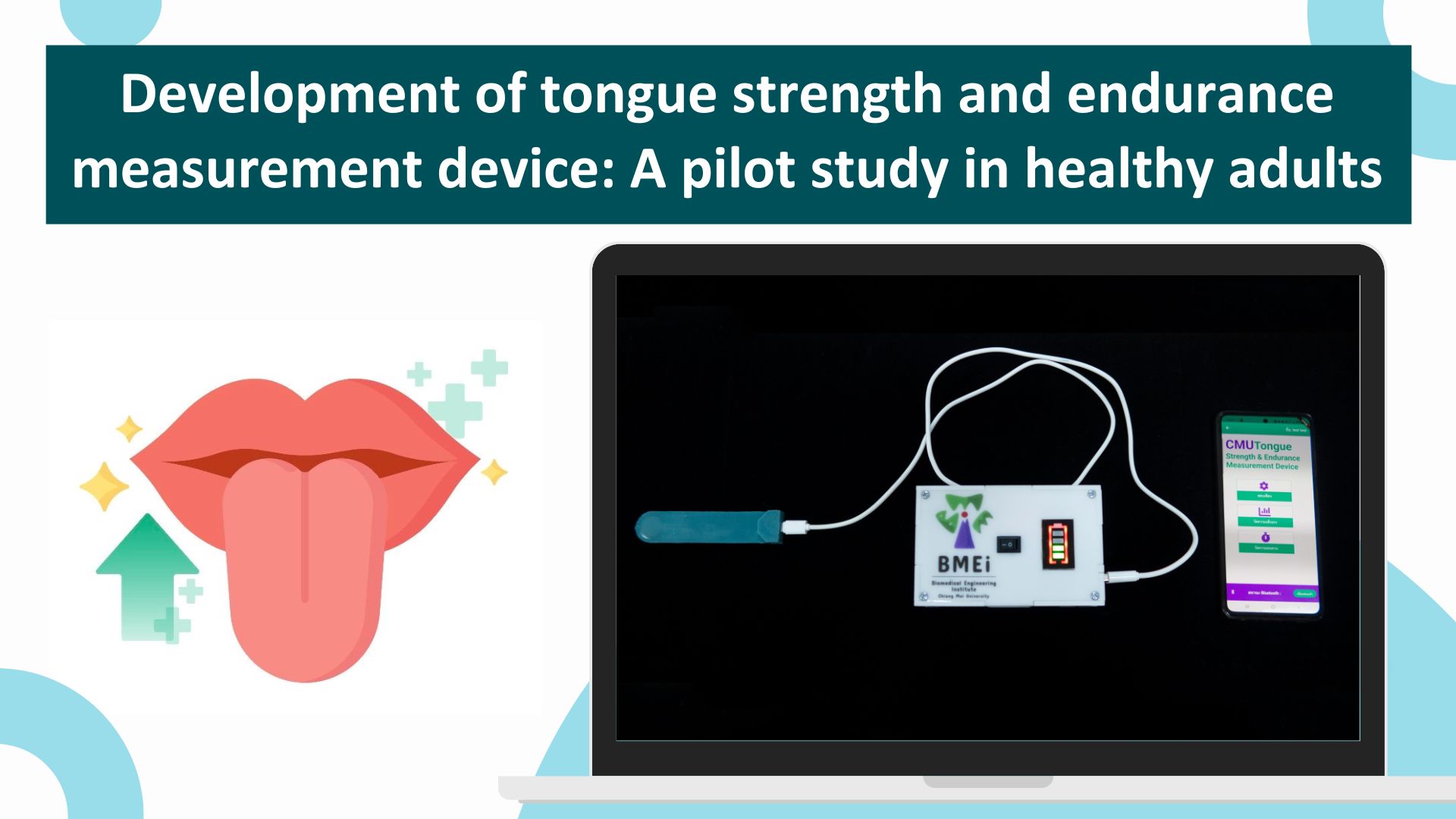
Development of tongue strength and endurance measurement device: A pilot study in healthy adults
Main Article Content
Abstract
Background: Safe and efficient swallowing relies on adequate tongue strength and endurance. Thus, tongue strength and endurance assessments are essential for swallowing rehabilitation for individuals with swallowing difficulties due to tongue structure and function abnormalities. These tongue functions can be objectively measured using a standard device. However, in Thailand, assessing tongue strength and endurance using standard devices is not widespread in clinical practice due to the high cost of importing these devices.
Objective: This study aimed to develop a precise, accurate, and reliable tongue function measurement device for the clinical assessment of tongue strength and endurance.
Materials and methods: This study was divided into three phases: 1) Development of a tongue strength and endurance measurement device in a laboratory setting and administration of a satisfaction questionnaire, 2) Trial of the prototype device with six participants, and 3) Assessment of the test-retest reliability of the developed device and investigation of tongue strength and endurance values with twenty participants.
Results: As a result of this development, a novel device for measuring tongue strength and endurance was obtained, which provides measurements in units of newtons (N) and kilopascals (kPa) for strength and seconds (s) for endurance. The device’s development cost was significantly lower compared to imported commercially available devices while maintaining the performance standards for medical measurement devices. This was demonstrated by its accuracy ranging from 96.40% to 100%, high precision with a Coefficient of Variation (% CV) of 0.90% to 4.21%, and moderate to excellent reliability with an Intraclass Correlation Coefficient (ICC) of 0.56 to 0.93. Furthermore, statistically significant differences (p<0.01) were observed between genders, especially in anterior tongue strength.
Conclusion: The tongue strength and endurance measurement device developed through this study can be utilized for clinical tongue function assessment, giving patients more access to objective evaluations of tongue strength and endurance at a lower examination cost.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008; 19(4): 691-707. doiL: 10.1016/j.pmr.2008.06.001.
Youmans SR, Stierwalt JA. Measures of tongue function related to normal swallowing. Dysphagia. 2006; 21(2): 102-11. doi: 10.1007/s00455-006-9013-z.
Groher ME. Normal swallowing in adults. In: Groher ME, Crary MA, editors. Dysphagia: clinical management in adults and children. 2nd Ed. St. Louis, Missouri: Elsevier; 2016. p. 19-40.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995; 50(5): 257-62. doi: 10.1093/gerona/50a.5.m257.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: Is there a diminished strength reserve? Dysphagia. 2009; 24(1): 57-65. doi: 10.1007/s00455-008-9171-2.
Kays SA, Hind JA, Gangnon RE, Robbins J. Effects of dining on tongue endurance and swallowing-related outcomes. J Speech Lang Hear Res. 2010; 53(4): 898- 907. doi: 10.1044/1092-4388(2009/09-0048).
Namasivayam AM, Steele CM, Keller H. The effect of tongue strength on meal consumption in long term care. Clin Nutr. 2016; 35(5): 1078-83. doi: 10.1016/j.clnu.2015.08.001.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015; 30(1): 80-7. doi: 10.1007/s00455-014-9577-y.
Stierwalt JAG, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007; 16(2): 148-56. doi: 10.1044/1058-0360(2007/019).
Minagi Y, Ono T, Hori K, Fujiwara S, Tokuda Y, Murakami K, et al. Relationships between dysphagia and tongue pressure during swallowing in Parkinson’s disease patients. J Oral Rehabil. 2018; 45(6): 459-66. doi: 10.1111/joor.12626.
Lazarus CL, Logemann JA, Pauloski BR, Rademaker AW, Larson CR, Mittal BB, et al. Swallowing and tongue function following treatment for oral and oropharyngeal cancer. J Speech Lang Hear Res. 2000; 43(4): 1011-23. doi: 10.1044/jslhr.4304.1011.
Hasegawa Y, Sugahara K, Fukuoka T, Saito S, Sakuramoto A, Horii N, et al. Change in tongue pressure in patients with head and neck cancer after surgical resection. Odontology. 2017; 105(4): 494-503. doi: 10.1007/s10266-016-0291-0.
Adams V, Mathisen B, Baines S, Lazarus C, Callister R. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia. 2013; 28(3): 350-69. doi: 10.1007/s00455-013-9451-3.
McCormack J, Casey V, Conway R, Saunders J, Perry A. OroPress a new wireless tool for measuring oro-lingual pressures: a pilot study in healthy adults. J Neuro Engineering Rehabil. 2015; 12(1):32.
Arakawa I, Igarashi K, Imamura Y, Müller F, AbouAyash S, Schimmel M. Variability in tongue pressure among elderly and young healthy cohorts: A systematic review and meta-analysis. J Oral Rehabil. 2021;48(4): 430-448. doi: 10.1111/joor.13076.
IOPI Medical. Product information. 2020 [cited 2020 Dec 26]. Available from: https://iopimedical.com/medical-professionals/.
JMS Co. Ltd. Product information. 2011 [cited 2020 Dec 26]. Available from: http://orarize.com/zetsuatsu/product.html.
AIM Technologies LLC. Digital Swallowing Workstation™ (DSW), model 7200. 2020 [cited 2020 Dec 24]. Available from: http://aimtech.ru/en/catalog/101.
Swallow Solutions LLC. SwallowSTRONG device. 2017 [cited 2020 Dec 24]. Available from: http://www.swallowsolutions.com/product-information/swallowstrong-device.
Hori K, Ono T, Tamine K, Kondo J, Hamanaka S, Maeda Y, et al. Newly developed sensor sheet for measuring tongue pressure during swallowing. J Prosthodont Res. 2009; 53(1): 28-32. doi: 10.1016/j.jpor.2008.08.008.
Sonnanta S. Measurement instruments and electrical measurements. Bangkok: SE-Education; 2000. (in Thai).
Kanyawattana N, Nakham N. Guidelines for the verification of applicability of chemical testing methods. Bangkok: Department of Primary Industries and Mines; 2012. (in Thai).
Pitsanlayanon M, Sitthithamwilai W, Pitsittaksak C, Waliprakon P, Itthasakul P, Pitithammaphon A. Effectiveness of Rama disposable bite block in patients undergoing electroconvulsive therapy: A pilot study. J Psychiatr Assoc Thailand [internet]. 2021 Jan 9 [cited 2021 Feb 15]; 65(3): 279-88. Available from: https://he01.tci-thaijo.org/index.php/JPAT/article/view/242152. (in Thai)
Hongsanun W, Insuk S. Quality assessment criteria for mobile health apps: A systematic review. WJST. 2020; 17(8): 745-59. doi: 10.48048/wjst.2020.6482
Turner RC, Carlson L. Indexes of item-objective congruence for multidimensional items. Int J Test. 2003; 3(2): 163-71. doi: 10.1207/S15327574IJT0302_5.
Edmiaston J, Connor LT, Loehr L, Nassief A. Validation of a dysphagia screening tool in acute stroke patients. Am J Crit Care. 2010; 19(4): 357-64. doi: 10.4037/ajcc2009961.
The Dental Association of Thailand. Guidelines for the control and prevention of COVID-19 infections in dentistry version 1. 2020 [cited 2021 Apr 5]. Available from: https://www.thaidental.or.th/main/download/upload/upload-204211344051371.pdf.
World Health Organization (WHO). Cleaning and disinfection of environmental surfaces in the context of COVID-19. 2020 [cited 2021 Apr 5]. Available from: https://www.who.int/publications/i/item/cleaningand-disinfection-of-environmental-surfaces-inthe-context-of-covid-19.
IBM. How to cite IBM SPSS Statistics or earlier versions of SPSS 2014 [cited 2024 May 24]. Available from: https://www.ibm.com/support/pages/how-citeibm-spss-statistics-or-earlier-versions-spss.
Interlink Electronics Inc. FSR 400 series data sheet. 2019 [cited 2022 May 25]. Available from: https://files.seeedstudio.com/wiki/Grove-Round_Force_ Sensor_FSR402/res/FSR402.pdf.
Zerynth documentation. DOIT Esp32 DevKit v1. 2021 [cited 2021 Jan 15]. Available from: https://docs.zerynth.com/latest/reference/boards/doit_esp32/docs/.
Webster JG, Eren H, Webster JG, Eren H. Measurement, instrumentation, and sensors handbook: spatial, mechanical, thermal, and radiation measurement. 2nd Ed. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2014.
Saengnil K, Posunnont P.”Reliability, validity, accuracy and precision on exercise physiology research” Method agreement and measurement error in the physiology of exercise. Veridian E-journal, Silpakorn University, Science and Technology Branch [internet]. 2018 Dec 12 [cited 2021 Jan 24]; 5(6): 1-19. Available from: https://ph01.tci-thaijo.org/index.php/VESTSU/article/view/159850. (in Thai).
Srisatitnarakul B. Development and verification of research instruments: psychometric measurement properties. Bangkok: Chulalongkorn University Printing House; 2012. (in Thai).
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2): 155-63. doi: 10.1016/j. jcm.2016.02.012.
Sedtasuppana A, Nunthayanon K, Prasitsak T, Tanaslarak R, Satrawaha S, Piyapattamin T. Comparison of arch widths measurements made on digital and plaster models. NUJST [internet]. 2017 Sep 15 [cited 2021 Jan 23]; 25(4): 9-16. Available from https://ph03. tci-thaijo.org/index.php/ahstr/article/view/1653.
Arakawa I, Abou-Ayash S, Genton L, Tsuga K, Leles CR, Schimmel M. Reliability and comparability of methods for assessing oral function: Chewing, tongue pressure and lip force. J Oral Rehabil. 2020; 47(7): 862-71. doi: 10.1111/joor.12976.
Center for Disease Control and Prevention (CDC). Guideline for disinfection and sterilization in healthcare facilities. 2008 [cited 6 Apr 2021]. Available from: https://www.cdc.gov/infection-control/media/pdfs/Guideline-Disinfection-H.pdf
Hao G, Chih Y-C, Ni A, Harada K, Thompson J, Chen S-C, et al. Maximum isometric tongue strength and tongue endurance in healthy adults. Oral Sci Int. 2023;20(2):115-24. doi: 10.1002/osi2.1158
Jeong DM, Shin YJ, Lee NR, Lim HK, Choung HW, Pang KM, et al. Maximal strength and endurance scores of the tongue, lip, and cheek in healthy, normal Koreans. J Korean Assoc Oral Maxillofac Surg. 2017; 43(4): 221-8. doi: 10.5125/jkaoms.2017.43.4.221