Radiation dose and image quality optimization in lumbar spine digital radiography for overweight and obese patients: Phantom study
Main Article Content
Abstract
Background: Lumbar spine radiography plays an important role in routine use for clinical practice in overweight and obese patients. The radiographer is responsible for setting suitable exposure factors for the tradeoffs between radiation dose and image quality (IQ).
Objective: To investigate the effect of different kVp values combined with AEC used on radiation dose and IQ for routine lumbar spine radiography in overweight and obese patients.
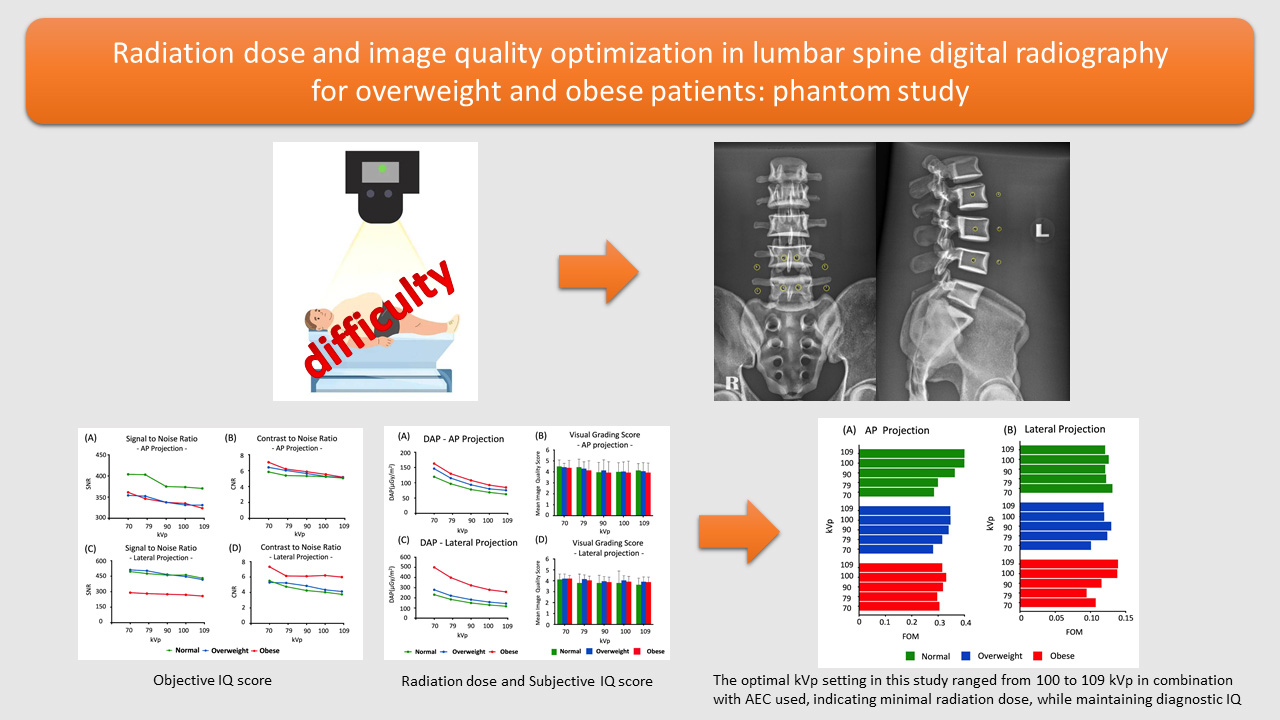
Materials and methods: A 1.5 and 3 cm thickness of frozen pork lard was placed on a pelvis phantom to simulate an overweight and obese patient, respectively. The phantom was imaged at 10 kVp intervals in combination with AEC used. For IQ evaluation, CNR and SNR were calculated, and the observer study was determined using visual grading scores (VGS) with a 5-point Likert scale. The radiation dose was measured using a DAP meter, and then the figure of merit (FOM) was calculated.
Results: SNR and CNR for both AP and lateral projection showed a slightly decreasing trend when kVp increased in all groups. The DAP values decreased when the higher kVp was selected with AEC used in each group. The VGS by five radiographers showed good image quality in all groups, while the FOM at 100 and 109 kVp was the highest score for both AP and lateral projections.
Conclusion: The optimal kVp setting in this study ranged from 100 to 109 kVp in combination with AEC used, indicating minimal radiation dose, while maintaining diagnostic IQ.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
World Health Organization. Obesity and overweight world health organization [Internet]. [cited 2021 Apr 1]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
De Lorenzo A, Gratteri S, Gualtieri P, et al. Why primary obesity is a disease? J Transl Med. 2019; 17: 1-13. doi.org/10.1186/s12967-019-1919-y.
Le NTT, Robinson J, Lewis SJ. Obese patients and radiography literature: what do we know about a big issue? J Med Radiat Sci. 2015; 62: 132-41. doi.org/10.1002/jmrs.105
Yanch JC, Behrman RH, Hendricks MJ, et al. Increased radiation dose to overweight and obese patients from radiographic examinations. Radiology. 2009; 252: 128-39. doi.org/10.1148/radiol.2521080141.
Van den Heuvel J, Punch A, Aweidah L, et al. Optimizing projectional radiographic imaging of the abdomen of obese patients: an e-delphi study. J Med Imaging Radiat Sci. 2019; 50:289-96. doi.org/10.1016/j.jmir. 2019.01.004.
Carucci LR. Imaging obese patients: problems and solutions. Abdom Imaging. 2013; 38: 630-46. doi. org/10.1007/s00261-012-9959-2.
Alqahtani SJ, Knapp KM. Imaging patients with obesity. J Med Radiat Sci. 2022; 69(1): 3-4. doi.org/10.1002/jmrs.560.
Chan CTP, Fung KKL. Dose optimization in lumbar spine radiographic examination by air gap method at CR and DR systems: A phantom study. J Med Imaging Radiat Sci. 2015; 46: 65-77. doi.org/10.1016/ j.jmir.2014.08.003.
Yoshizumi T, Nakamura T, Yamane M, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999; 211: 283-86. doi.org/10.1148/radiology.211.1.r99ap15283.
Ferreira T, Rasband W. ImageJ User Guide-Version 1. 44. 2012.
Gatt S, Portelli JL, Zarb F. Optimisation of the AP abdomen projection for larger patient body thicknesses. Radiography. 2022; 28: 107-14. doi.org/10.1016/j.radi.2021.08.009.
Office for Official Publications of the European Communities. European guidelines on quality criteria for diagnostic radiographic images. Luxemburg; 1996.
Hauge IH, Aandahl IJ, Baranzelli JP, et al. Radiography: impact of lower tube voltages on image quality and radiation dose in chest phantom radiography for averaged sized and larger patients. In: OPTIMAX 2017: optimising image quality for medical image. 2017. p. 47-62.
Cicchetti D V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994; 6: 284-90. doi.org/10.1037/1040-3590.6.4.284.
Birwadkar G, Ratta AK. Assessment of risk factors of obesity among residents of class iv employees’ quarters of a tertiary care hospital. J Evol Med Dent Sci. 2019; 8: 2367-70. doi.10.14260/jemds/2019/518.
Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc Dis. 2016; 5. doi.org/10.1177/2048004016633371.
Anuradha R, Hemachandran S, Dutta R. The waist circumference measurement: a simple method for assessing the abdominal obesity. J Clin Diagnostic Res. 2012; 6: 1510-3. doi.org/10.7860/JCDR/2012/4379.2545.
Ismail AA, Othman NS, Mohamad M, et al. Evaluating the relationship of body mass index and waist circumference on the image quality of abdominal computed radiography. J Sains Kesihat Malaysia. 2020; 18: 11-8. https://ejournal.ukm.my/jskm/article/view/26118/10301.
Allisy-Roberts P, Williams J. Farr’s physics for medical imaging. 2nd Ed. Elsevier Health Sciences; 2007.
Mifsud K, Portelli JL, Zarb F, et al. Evaluating the use of higher kVp and copper filtration as a dose optimisation tool in digital planar radiography. Radiography. 2022; 28: 586-92. doi.org/10.1016/j.radi.2022.04.002.
Bontrager KL, Lampignano JP. Textbook of positioning and related anatomy. 8th Ed. 2014.
Ghayour-Saffar N, Ehsanbakhsh A, Keshtkar M, Pandesh S. Evaluation of DAP Values Obtained from Chest X-rays in Children under 12 Years of Age Referred to Educational Hospitals of Birjand University of Medical Sciences in 2020. Frontiers Biomed Technol. 2022; 9(3): 185-90. doi.org/10.18502/fbt.v9i3.9644.