Proteinuria in Kidney Transplant Recipients
Main Article Content
Abstract
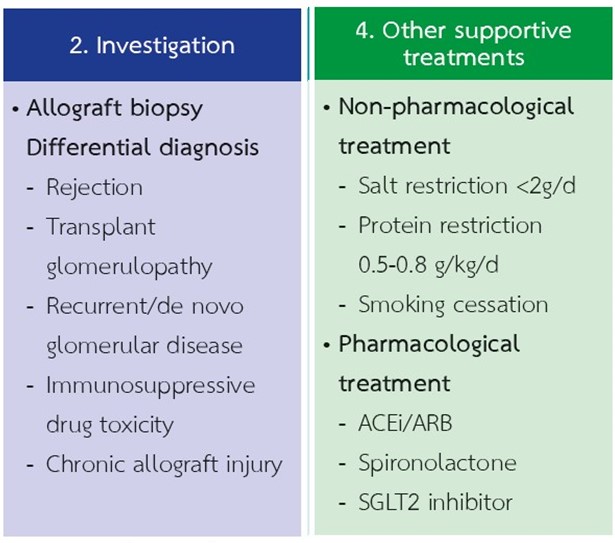
Proteinuria is a common complication following kidney transplantation and is a strong predictor of transplant rejection, allograft loss, and mortality. It can arise from several causes, including immune rejection of the transplanted kidney, underlying glomerular diseases, or tubular damage caused by immunosuppressive medications. The key to managing proteinuria in transplant recipients is identifying and directly addressing the underlying cause. Additionally, lifestyle modifications—such as quitting smoking and reducing salt and protein intake—are recommended. Blocking the renin-angiotensin system shows promise in reducing proteinuria, although its long-term effects on graft and patient survival remain uncertain. Research into new therapies for post-transplant proteinuria continues, with drugs like sodium-glucose cotransporter 2 inhibitors showing promising results in reducing proteinuria and slowing the decline in allograft function. However, more studies are needed to confirm their efficacy and safety in kidney transplant recipients.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Matsushita K, Jassal SK, Sang Y, Ballew SH, Grams ME, Surapaneni A, et al. Incorporating kidney disease measures into cardiovascular risk prediction: Development and validation in 9 million adults from 72 datasets. EClinicalMedicine. 2020;27:100552.
Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49-61.
Knoll GA. Proteinuria in kidney transplant recipients: prevalence, prognosis, and evidence-based management. Am J Kidney Dis. 2009;54(6):1131-44.
Ponticelli C, Graziani G. Proteinuria after kidney transplantation. Transpl Int. 2012;25(9):909-17.
Fernandez-Fresnedo G, Plaza JJ, Sanchez-Plumed J, Sanz-Guajardo A, Palomar-Fontanet R, Arias M. Proteinuria: a new marker of long- term graft and patient survival in kidney transplantation. Nephrol Dial Transplant. 2004;19 Suppl 3:iii47-51.
Molcho M, Rozen-Zvi B, Shteinmats T, Ben Dor N, Vahav I, Nesher E, et al. Temporal changes of proteinuria after kidney transplantation: association with cardiovascular morbidity and mortality. J Nephrol. 2020;33(5):1059-66.
รายงานข้อมูลการปลูกถ่ายอวัยวะ ประจำปี 2565 [Internet]. บริษัท ปริ้นท์แอนด์มอร์ จำกัด. 2022 [cited December 4, 2022]. Available from: https://www.transplantthai.org/?page=annual-report-old.
Myslak M, Amer H, Morales P, Fidler ME, Gloor JM, Larson TS, et al. Interpreting post-transplant proteinuria in patients with proteinuria pre-transplant. Am J Transplant. 2006;6(7):1660-5.
Oblak M, Mlinsek G, Kojc N, Frelih M, Buturovic-Ponikvar J, Arnol M. Spot Urine Protein Excretion in the First Year Following Kidney Transplantation Associates With Allograft Rejection Phenotype at 1-Year Surveillance Biopsies: An Observational National-Cohort Study. Front Med (Lausanne). 2021;8:781195.
Zhang Q, Budde K, Schmidt D, Halleck F, Duerr M, Naik MG, et al. Clinicopathologic Features and Risk Factors of Proteinuria in Transplant Glomerulopathy. Front Med (Lausanne). 2021;8:666319.
Canaud G, Dion D, Zuber J, Gubler MC, Sberro R, Thervet E, et al. Recurrence of nephrotic syndrome after transplantation in a mixed population of children and adults: course of glomerular lesions and value of the Columbia classification of histological variants of focal and segmental glomerulosclerosis (FSGS). Nephrol Dial Transplant. 2010;25(4):1321-8.
Uffing A, Perez-Saez MJ, Mazzali M, Manfro RC, Bauer AC, de Sottomaior Drumond F, et al. Recurrence of FSGS after Kidney Transplantation in Adults. Clin J Am Soc Nephrol. 2020;15(2):247-56.
Kashgary A, Sontrop JM, Li L, Al-Jaishi AA, Habibullah ZN, Alsolaimani R, et al. The role of plasma exchange in treating post-transplant focal segmental glomerulosclerosis: A systematic review and meta-analysis of 77 case-reports and case-series. BMC Nephrol. 2016;17(1):104.
Kidney Disease: Improving Global Outcomes Glomerular Diseases Work G. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 2021;100(4S):S1-S276.
Leon J, Perez-Saez MJ, Batal I, Beck LH, Jr., Rennke HG, Canaud G, et al. Membranous Nephropathy Posttransplantation: An Update of the Pathophysiology and Management. Transplantation. 2019;103(10):1990-2002.
Moroni G, Belingheri M, Frontini G, Tamborini F, Messa P. Immunoglobulin A Nephropathy. Recurrence After Renal Transplantation. Front Immunol. 2019;10:1332.
Di Vico MC, Messina M, Fop F, Barreca A, Segoloni GP, Biancone L. Recurrent IgA nephropathy after renal transplantation and steroid withdrawal. Clin Transplant. 2018;32(4):e13207.
Leeaphorn N, Garg N, Khankin EV, Cardarelli F, Pavlakis M. Recurrence of IgA nephropathy after kidney transplantation in steroid continuation versus early steroid-withdrawal regimens: a retrospective analysis of the UNOS/OPTN database. Transpl Int. 2018;31(2):175-86.
Leal R, Tsapepas D, Crew RJ, Dube GK, Ratner L, Batal I. Pathology of Calcineurin and Mammalian Target of Rapamycin Inhibitors in Kidney Transplantation. Kidney Int Rep. 2018;3(2):281-90.
Kidney Disease: Improving Global Outcomes Transplant Work G. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9 Suppl 3:S1-155.
Gleixner EM, Canaud G, Hermle T, Guida MC, Kretz O, Helmstadter M, et al. V-ATPase/mTOR signaling regulates megalin-mediated apical endocytosis. Cell Rep. 2014;8(1):10-9.
Akbari A, Fergusson D, Kokolo MB, Ramsay T, Beck A, Ducharme R, et al. Spot urine protein measurements in kidney transplantation: a systematic review of diagnostic accuracy. Nephrol Dial Transplant. 2014;29(4):919-26.
Noborisaka Y, Ishizaki M, Yamada Y, Honda R, Yokoyama H, Miyao M, et al. The effects of continuing and discontinuing smoking on the development of chronic kidney disease (CKD) in the healthy middle-aged working population in Japan. Environ Health Prev Med. 2013;18(1):24-32.
Ohkuma T, Nakamura U, Iwase M, Ide H, Fujii H, Jodai T, et al. Effects of smoking and its cessation on creatinineand cystatin C-based estimated glomerular filtration rates and albuminuria in male patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. Hypertens Res. 2016;39(10):744-51.
Lee S, Kang S, Joo YS, Lee C, Nam KH, Yun HR, et al. Smoking, Smoking Cessation, and Progression of Chronic Kidney Disease: Results From KNOW-CKD Study. Nicotine Tob Res. 2021;23(1):92-8.
Fu YC, Xu ZL, Zhao MY, Xu K. The Association Between Smoking and Renal Function in People Over 20 Years Old. Front Med (Lausanne). 2022;9:870278.
Lopez V, Martin M, Cobelo C, Aranda P, Cabello M, Sola E, et al. Renin-angiotensin system dual blockade using angiotensin receptor plus aliskiren decreases severe proteinuria in kidney transplant recipients. Transplant Proc. 2010;42(8):2883-5.
Underwood PW, Sheetz KH, Cron DC, Terjimanian MN, Englesbe MJ, Waits SA. Cigarette smoking in living kidney donors: donor and recipient outcomes. Clin Transplant. 2014;28(4):419-22.
Verma A, Popa C. The Interplay Between Dietary Sodium Intake and Proteinuria in CKD. Kidney Int Rep. 2023;8(6):1133-6.
Cirillo M, Cavallo P, Zulli E, Villa R, Veneziano R, Costanzo S, et al. Sodium Intake and Proteinuria/Albuminuria in the Population-Observational, Cross-Sectional Study. Nutrients. 2021;13(4).
Kim HJ, Jung CY, Kim HW, Park JT, Yoo TH, Kang SW, et al. Proteinuria Modifies the Relationship Between Urinary Sodium Excretion and Adverse Kidney Outcomes: Findings From KNOW-CKD. Kidney Int Rep. 2023;8(5):1022-33.
de Vries LV, Dobrowolski LC, van den Bosch JJ, Riphagen IJ, Krediet CT, Bemelman FJ, et al. Effects of Dietary Sodium Restriction in Kidney Transplant Recipients Treated With Renin-Angiotensin-Aldosterone System Blockade: A Randomized Clinical Trial. Am J Kidney Dis. 2016;67(6):936-44.
Rosenberg ME, Salahudeen AK, Hostetter TH. Dietary protein and the renin-angiotensin system in chronic renal allograft rejection. Kidney Int Suppl. 1995;52:S102-6.
Biesenbach G, Zazgornik J, Janko O, Hubmann R, Syre G. Effect of mild dietary protein restriction on urinary protein excretion in patients with renal transplant fibrosis. Wien Med Wochenschr. 1996;146(4):75-8.
Bernardi A, Biasia F, Pati T, Piva M, D’Angelo A, Bucciante G. Long-term protein intake control in kidney transplant recipients: effect in kidney graft function and in nutritional status. Am J Kidney Dis. 2003;41(3 Suppl 1):S146-52.
Kidney Disease: Improving Global Outcomes Blood Pressure Work G. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021;99(3S):S1-S87.
Hiremath S, Fergusson D, Doucette S, Mulay AV, Knoll GA. Renin angiotensin system blockade in kidney transplantation: a systematic review of the evidence. Am J Transplant. 2007;7(10):2350-60.
Hiremath S, Fergusson DA, Fergusson N, Bennett A, Knoll GA. Renin-Angiotensin System Blockade and Long-term Clinical Outcomes in Kidney Transplant Recipients: A Meta-analysis of Randomized Controlled Trials. Am J Kidney Dis. 2017;69(1):78-86.
Gonzalez Monte E, Andres A, Polanco N, Toribio MJ, Santana R, Gutierrez Martinez E, et al. Addition of spironolactone to dual blockade of renin angiotensin system dramatically reduces severe proteinuria in renal transplant patients: an uncontrolled pilot study at 6 months. Transplant Proc. 2010;42(8):2899-901.
de Sousa MV, Guida JP, do Valle CF, Camargo LF, Rivelli GG, Mazzali M. Spironolactone in Post-Transplant Proteinuria: A Safe Alternative Therapy. Transplant Proc. 2017;49(4):813-6.
Margonato D, Galati G, Mazzetti S, Cannistraci R, Perseghin G, Margonato A, et al. Renal protection: a leading mechanism for cardiovascular benefit in patients treated with SGLT2 inhibitors. Heart Fail Rev. 2021;26(2):337-45.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380(24):2295-306.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2020;383(15):1436-46.
The E-KCG, Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, et al. Empagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2023;388(2):117-27.
Oliveras L, Montero N, Cruzado JM. Searching in the maze: sodium-glucose cotransporter-2 inhibitors in kidney transplant recipients to improve survival. Clin Kidney J. 2023;16(6):909-13.
Demir ME, Ozler TE, Merhametsiz O, Sozener U, Uyar M, Ercan Z, et al. The results of SGLT-2 inhibitors use in kidney transplantation: 1-year experiences from two centers. Int Urol Nephrol. 2023;55(11):2989-99.