Metformin Associated Lactic Acidosis
Main Article Content
Abstract
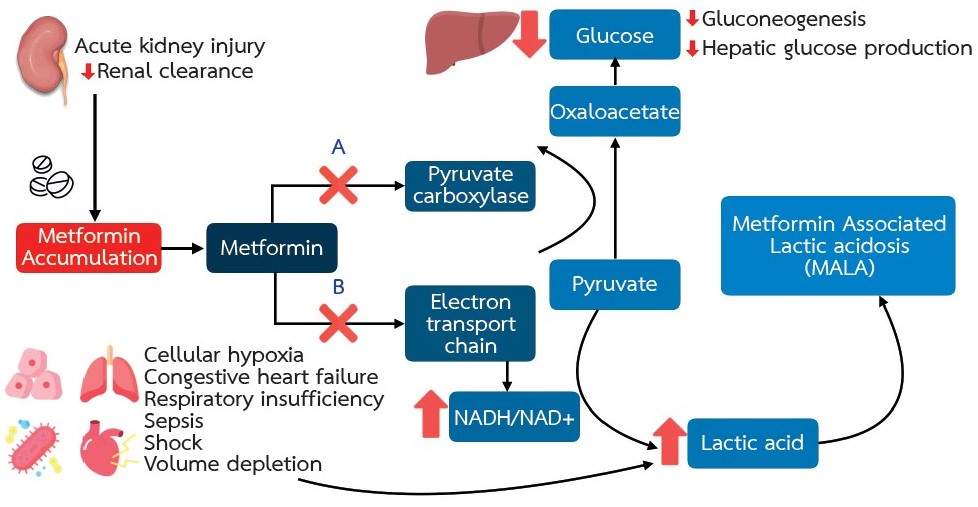
Metformin is recommended as the first-line treatment for type 2 diabetes mellitus and its use is widespread all over the world. The drug can be prescribed as a single agent or in combination with other glucose lowering medications. The use of metformin is associated with a reduction in the risk of death from cardiovascular disease. Gastrointestinal symptoms are the most frequent side effect. Metformin-associated lactic acidosis (MALA) is a less common but life-threatening complication of metformin. MALA is caused by an accumulation of metformin and lactic acid in the body as a result of reduced renal excretion. Prompt diagnosis and management are required to reduce adverse patient outcomes. The management includes close monitoring, correction of electrolytes and acid-base disturbances, treatment of other comorbid conditions and, in severe cases, removal of metformin from the body by hemodialysis. Prevention can be achieved through risk assessment prior to prescribing the medication and adjustment of the dosage in patients with reduced kidney function. The patients should be advised to stop taking the medication when suspicious symptoms of MALA occur and promptly seek medical attention.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Hadden DR. Goat's rue - French lilac - Italian fitch - Spanish sainfoin: gallega officinalis and metformin: the Edinburgh connection. J R Coll Physicians Edinb. 2005;35(3):258-60.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140-S57.
Lv Z, Guo Y. Metformin and Its Benefits for Various Diseases. Front Endocrinol (Lausanne). 2020;11:191.
Foretz M, Guigas B, Bertrand L, Pollak M, Viollet B. Metformin: from mechanisms of action to therapies. Cell Metab. 2014;20(6):953-66.
Jackson RA, Hawa MI, Jaspan JB, Sim BM, Disilvio L, Featherbe D, et al. Mechanism of metformin action in non-insulin-dependent diabetes. Diabetes. 1987;36(5):632-40.
Bailey CJ, Wilcock C, Scarpello JH. Metformin and the intestine. Diabetologia. 2008;51(8):1552-3.
Bailey CJ, Turner RC. Metformin. N Engl J Med. 1996;334(9):574-9.
Graham GG, Punt J, Arora M, Day RO, Doogue MP, Duong JK, et al. Clinical pharmacokinetics of metformin. Clin Pharmacokinet. 2011;50(2):81-98.
Bonnet F, Scheen A. Understanding and overcoming metformin gastrointestinal intolerance. Diabetes Obes Metab. 2017;19(4):473-81.
Blumenberg A, Benabbas R, Sinert R, Jeng A, Wiener SW. Do Patients Die with or from Metformin-Associated Lactic Acidosis (MALA)? Systematic Review and Meta-analysis of pH and Lactate as Predictors of Mortality in MALA. J Med Toxicol. 2020;16(2):222-9.
Thammavaranucupt K, Phonyangnok B, Parapiboon W, Wongluechai L, Pichitporn W, Sumrittivanicha J, et al. Metformin-associated lactic acidosis and factors associated with 30-day mortality. PLoS One. 2022;17(8):e0273678.
Richy FF, Sabido-Espin M, Guedes S, Corvino FA, Gottwald-Hostalek U. Incidence of lactic acidosis in patients with type 2 diabetes with and without renal impairment treated with metformin: a retrospective cohort study. Diabetes Care. 2014;37(8):2291-5.
Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60(9):1577-85.
Pham AQ, Xu LH, Moe OW. Drug-Induced Metabolic Acidosis. F1000Res. 2015;4.
Hunter RW, Hughey CC, Lantier L, Sundelin EI, Peggie M, Zeqiraj E, et al. Metformin reduces liver glucose production by inhibition of fructose-1-6-bisphosphatase. Nat Med. 2018;24(9):1395-406.
Hur KY, Lee MS. New mechanisms of metformin action: Focusing on mitochondria and the gut. J Diabetes Investig. 2015;6(6):600-9.
DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism. 2016;65(2):20-9.
Asif S, Bennett J, Marakkath B. Metformin-associated Lactic Acidosis: An Unexpected Scenario. Cureus. 2019;11(4):e4397.
Ashraf S, Upreti P, Karki S, Khan M, Nasr R. Metformin-Associated Lactic Acidosis: A Case Report and Review. Cureus. 2022;14(4):e24220.
Schadle P, Tschritter O, Kellerer M. Metformin Associated Lactic Acidosis in Clinical Practice - A Case Series. Exp Clin Endocrinol Diabetes. 2021;129(11):842-7.
Gan SC, Barr J, Arieff AI, Pearl RG. Biguanide-associated lactic acidosis. Case report and review of the literature. Arch Intern Med. 1992;152(11):2333-6.
Almirall J, Briculle M, Gonzalez-Clemente JM. Metformin-associated lactic acidosis in type 2 diabetes mellitus: incidence and presentation in common clinical practice. Nephrol Dial Transplant. 2008;23(7):2436-8.
Lalau JD, Lemaire-Hurtel AS, Lacroix C. Establishment of a database of metformin plasma concentrations and erythrocyte levels in normal and emergency situations. Clin Drug Investig. 2011;31(6):435-8.
Kraut JA, Madias NE. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol. 2010;6(5):274-85.
Lalau JD, Race JM. Lactic acidosis in metformin-treated patients. Prognostic value of arterial lactate levels and plasma metformin concentrations. Drug Saf. 1999;20(4):377-84.
Teale KF, Devine A, Stewart H, Harper NJ. The management of metformin overdose. Anaesthesia. 1998;53(7):698-701.
Feeney-Stewart F. The sodium bicarbonate controversy. Dimens Crit Care Nurs. 1990;9(1):22-8.
Cuhaci B, Lee J, Ahmed Z. Sodium bicarbonate controversy in lactic acidosis. Chest. 2000;118(3):882-4.
Rosival V. Evaluating sodium bicarbonate controversy. Chest. 2001;119(5):1622-3.
Calello DP, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, Gosselin S, et al. Extracorporeal Treatment for Metformin Poisoning: Systematic Review and Recommendations From the Extracorporeal Treatments in Poisoning Workgroup. Crit Care Med. 2015;43(8):1716-30.
Harding SA, Biary R, Hoffman RS, Su MK, Howland MA. A Pharmacokinetic Analysis of Hemodialysis for Metformin-Associated Lactic Acidosis. J Med Toxicol. 2021;17(1):70-4.
Correia MS, Horowitz BZ. Continuous extracorporeal clearance in metformin-associated lactic acidosis and metformin-induced lactic acidosis: a systematic review. Clin Toxicol (Phila). 2022;60(11):1266-76.
Deepak V, Neel S, Lohana AC, Tanase A. Metformin-associated Lactic Acidosis Successfully Treated with Continuous Renal Replacement Therapy. Cureus. 2019;11(8):e5330.
Regolisti G, Antoniotti R, Fani F, Greco P, Fiaccadori E. Treatment of Metformin Intoxication Complicated by Lactic Acidosis and Acute Kidney Injury: The Role of Prolonged Intermittent Hemodialysis. Am J Kidney Dis. 2017;70(2):290-6.
Navaneethan SD, Zoungas S, Caramori ML, Chan JCN, Heerspink HJL, Hurst C, et al. Diabetes Management in Chronic Kidney Disease: Synopsis of the KDIGO 2022 Clinical Practice Guideline Update. Ann Intern Med. 2023;176(3):381-7.
Hanna RM, Rhee CM, Kalantar-Zadeh K. Metformin in chronic kidney disease: a strong dose of caution. Kidney Int. 2020;98(5):1101-5.
Jones GC, Macklin JP, Alexander WD. Contraindications to the use of metformin. BMJ. 2003;326(7379):4-5.
Landewe-Cleuren S, van Zwam WH, de Bruin TW, de Haan M. [Prevention of lactic acidosis due to metformin intoxication in contrast media nephropathy]. Ned Tijdschr Geneeskd. 2000;144(40):1903-5.