Factors affecting hemoglobin levels of patients with end-stage kidney disease in the maintenance phase: A prospective observational study
Main Article Content
Abstract
Background: Patients with end-stage kidney disease (ESKD) undergoing hemodialysis almost invariably develop anemia, which can significantly impair their quality of life. It is uncommon to find patients with consistently normal hemoglobin (Hb) levels; therefore, identifying the contributing factors is essential.
Objectives: This study aimed to identify factors affecting Hb levels in ESKD patients during maintenance phase.
Materials and methods: This prospective observational study was conducted at a regional hospital in Yogyakarta. The Hb cutoff point of 10 g/dL was used as the minimum standard for the maintenance phase, based on the Dialysis Consensus of the Indonesian Nephrology Association. The study included ESKD patients aged ≥18 years undergoing hemodialysis. The initial sample comprised 76 patients (38 with Hb >10 gm/dL and 38 with Hb ≤10 gm/dL); however, 65 patients were included in the final analysis after 11 were excluded due to dropout. Samples were matched based on age, sex, duration of hemodialysis, and comorbidities. Data were collected using patient medical record observation sheets, food record sheets, and the brief illness perception questionnaire (B-IPQ). Statistical analyses were performed using chi-square and logistic regression with a backward elimination method.
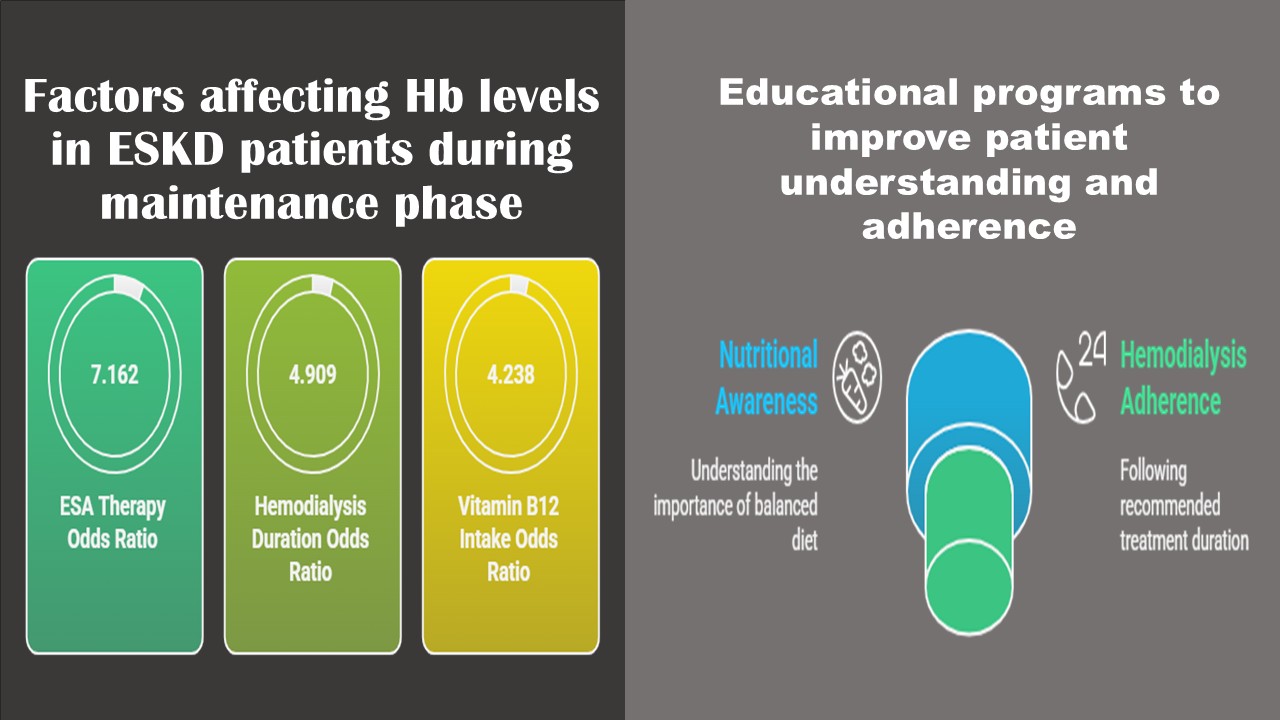
Results: A total of 65 participants were analyzed (33 patients with Hb >10 and 32 patients with Hb ≤10). Factors that showed significant associations with Hb levels were erythropoietin-stimulating agent (ESA) therapy odds ratio (OR)=7.162, 95% confidence interval [CI]=2.046-25.071, p=0.002), duration of hemodialysis (OR=4.909, 95% CI=1.299-18.551, p=0.019), and vitamin B12 intake (OR=4.238, 95% CI=1.183-15.176, p=0.027).
Conclusion: Erythropoietin stimulating agent therapy, duration of hemodialysis, and vitamin B12 intake were identified as factors influencing the improvement of Hb levels in patients with ESKD. Educational interventions are needed to enhance patients’ understanding of the importance of maintaining balanced nutritional intake and adhering to optimal hemodialysis duration.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
CDC. Chronic Kidney Disease in the United States, 2021. Published 2021. https://www.cdc.gov/kidneydisease/publicationsresources/CKDnational-facts.html%0AWhen.
Indonesian Renal Registry. Report of Indonesian Renal Registry.; 2018. https://www.indonesianrenalregistry.org/data/IRR 2018.pdf.
Cases A, Egocheaga MI, Tranche S, et al. Anemia of chronic kidney disease: protocol of study, management and referral to nephrology. Nefrología. 2018; 38(1): 8-12. doi:10.1016/j.nefroe.2018.01.007.
Mathias SD, Blum SI, Sikirica V, Johansen KL, Colwell HH, Okoro T. Symptoms and impacts in anemia of chronic kidney disease. J Patient-Reported Outcomes. 2020; 4(1): 64-74. doi:10.1186/s41687-020-00215-8.
Offurum A, Wagner LA, Gooden T. Adverse safety events in patients with chronic kidney disease (CKD). Expert Opin Drug Saf. 2016; 15(12): 1597-607. doi:10.1080/14740338.2016.1236909.
NICE. Guidance chronic kidney disease: Managing anaemia. National Institute for Health and Care Excellence. Published June 3, 2015. Accessed December 8, 2021. https://www.nice.org.uk/guidance/ng8.
Wjayantii S, Yetti K, Masfuri. Analysis of the factors affecting the hospital readmission incidence of hemodialysis patients in Bandar Lampung, Indonesia. Enferm Clin. 2019; 29(2): 720-4. doi:10.1016/j.enfcli.2019.04.110.
Shiferaw WS, Akalu TY, Aynalem YA. Risk factors for anemia in patients with chronic renal failure: a systematic review and meta-analysis. Ethiop J Health Sci. 2020; 30(5): 829-42. doi:10.4314/ejhs.v30i5.23.
Obeagu EI, Babar Q, Obeagu GU. Megaloblastic anaemia - a review. Int J Curr Res Med Sci. 2021; 7(5): 17-24. doi:10.22192/ijcrms.2021.07.05.004.
González-Ortiz A, Correa-Rotter R, Vázquez-Rangel A, Vega-Vega O, Espinosa-Cuevas Á. Relationship between protein-energy wasting in adults with chronic hemodialysis and the response to treatment with erythropoietin. BMC Nephrol. 2019; 20(1): 1-9. doi:10.1186/s12882-019-1457-0.
Lopez MJ, Mohiuddin SS. Biochemistry, essential amino acids. StatPearls Publishing; 2022. Accessed August 2, 2022. https://www.ncbi.nlm.nih.gov/books/NBK557845/.
Mikhail A, Brown C, Williams JA, et al. Renal association clinical practice guideline on anaemia of chronic kidney disease. BMC Nephrol. 2017; 18(1): 345-74. doi:10.1186/S12882-017-0688-1.
Froese DS, Fowler B, Baumgartner MR. Vitamin B12, folate, and the methionine remethylation cycle-biochemistry, pathways, and regulation. J Inherit Metab Dis. 2019; 42(4): 673-85. doi:10.1002/jimd.12009.
Hansen DK, Inselman AL. Folic acid. StatPearls Publishing; 2022. doi:10.1016/B978-0-12-386454-3.00731-4.
Hekmat R. Hemodialysis adequacy and its impact on long-term patient survival in demographically, socially, and culturally homogeneous patients. Int J Nephrol. 2020; 2020. doi:10.1155/2020/9857123.
Ayesh MH, Bataineh A, Elamin E, Khader Y, Alawneh K, Rababah M. Adequate Hemodialysis improves anemia by enhancing glucose-6-phosphate dehydrogenase activity in patients with end-stage renal disease. BMC Nephrol. 2014; 15(1): 1-5. doi:10.1186/1471-2369-15-155.
Ghasemi F, Abdi A, Salari N, Tohidi MR, Faraji A. Comparing the effects of intravenous and subcutaneous erythropoietin on blood indices in hemodialysis patients. Sci Rep. 2019; 9(1): 1-8. doi:10.1038/s41598-018-38193-z.
Kim S, Kim E, Ryu E. Illness perceptions, self-care management , and clinical outcomes according to age-group in Korean hemodialysis patients. Int J Environ Res Public Health. 2019; 16(22): 1-12. doi:10.3390/ijerph16224459.
Gunarathne TGNS, Tang LY, Lim SK, Nanayakkara N, Damayanthi HDWT, Abdullah KL. Factors associated with aymptom burden in adults with chronic kidney disease undergoing hemodialysis: a prospective study. Int J Environ Res Public Health. 2022; 19(9): 1-13. doi:10.3390/ijerph19095540.
Xu Y, Evans M, Barany P, James G, Sjölander A, Carrero JJ. Factors affecting pre-end-stage kidney disease haemoglobin control and outcomes following dialysis initiation: a nationwide study. Clin Kidney J. 2021; 14(7): 1780-8. doi:10.1093/ckj/sfaa213.
Yin S, Du Y, Guo Y, Guo G, Sun D, Yao L. Multifactorial analysis of renal anemia-associated substandard hemoglobin levels and prevalence of anemia in patients on maintenance hemodialysis in Liaoning Province: a cross-sectional study. Ann Palliat Med. 2022; 11(12): 3743-54. doi:10.21037/apm-22-1348.
Sutranto AL, Liwang F, Nugroho P, Harimurti K. Pos-620 factors influencing hemoglobin variability in chronic hemodialysis patients: A prospective cohort study in tertiary hospital, Jakarta, Indonesia. Kidney Int Reports. 2021; 6(Suppl 4): S270. doi:https://doi.org/10.1016/j.ekir.2021.03.649.
Qian G, Zhu Y, Tao S, et al. Increased hemoglobin concentration and related factors in maintenance hemodialysis patients in Anhui, China. Med (United States). 2022; 101(46): E31397. doi:10.1097/MD.0000000000031397.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1): S31-S34. doi:10.4103/sja.SJA_543_18.
Indonesian Nephrology Association. Dialysis consensus. 1st Edition; 2003. https://www.pernefri.org/konsensus/KonsensusDialisis.pdf.
Par’i HM, Wiyono S, Harjatmo TP. Nutritional status assessment. Center for Health Human Resources Education, Indonesian Ministry of Health; 2017.
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006; 60(6): 631-7. doi:10.1016/j.jpsychores.2005.10.020.
Hadisa N, Susanti R, Robiyanto. Validity andreliability test of Indonesian Version B-IPQ to CRF Outpatients in RSUD Soedarso Pontianak. J Manaj dan Pelayanan Farm. 2017; 7(4): 175-81. doi:10.22146/jmpf.33340.
Indonesian Nephrology Association. Consensus on anemia management in chronic kidney disease. 2nd Edition; 2011. https://www.pernefri.org/konsensus/Konsensus Anemia - Isi.pdf.
Brar SK, Perveen S, Chaudhry MR, AlBabtain S, Amreen S, Khan S. Erythropoietin-induced hypertension: A review of pathogenesis, treatment, and role of blood v iscosity. Cureus. 2021; 13(1): e12804. doi:10.7759/CUREUS.12804.
Puspita AA, Setianingrum ELS, Lidia K. The effect of hemodialysis frequency on the differences hemoglobin levels and erythrocyte indices in chronic kidney failure patients pre and post hemodialysis at Prof. Dr. W. Z. Johannes Hospital. Cendana Med J. 2019; 7(1): 102-111. doi:10.35508/cmj.v7i1.1462.
Kim HJ, Kim TE, Han M, et al. Effects of blood urea nitrogen independent of the estimated glomerular filtration rate on the development of anemia in non-dialysis chronic kidney disease: the results of the KNOW-CKD Study. PLoS One. 2021; 16(9): e0257305. doi:10.1371/journal.pone.0257305.
Tayebi A, Biniaz V, Savari S, et al. Effect of vitamin B12 supplementation on serum homocysteine in patients undergoing hemodialysis: a randomized controlled trial. Saudi J Kidney Dis Transpl. 2016; 27(2): 256-62. doi:10.4103/1319-2442.178255.
Nahas ARFM, Al Zarzour RH, Abu Laila ASM, et al. Effect of B12 supplementation on renal anemia among hemodialysis patients at El-Najar hospital, Gaza strip. J Ren Inj Prev. 2022; x(x): 1-5. doi:10.34172/jrip.2022.32009.
Vittoria V. The relationship between food intake, nutritional status and hemodialysis adequacy with anemia in terminal renal failure patients undergoing routine hemodialysis at RSUP Dr.Sardjito Hospital, Yogyakarta. Published online 2016. https://etd.repository.ugm.ac.id/penelitian/detail/103973.
Gvili AG, Schechter A, Zvi BR. Iron deficiency anemia in chronic kidney disease. Acta Haematol. 2019; 142(1): 44-50. doi:10.1159/000496492.
Loutradis C, Skodra A, Georgianos P, et al. Diabetes mellitus increases the prevalence of anemia in patients with chronic kidney disease: a nested case-control study. World J Nephrol. 2016; 5(4): 358. doi:10.5527/wjn.v5.i4.358.
Cappuccilli M, Bergamini C, Giacomelli FA, et al. Vitamin B supplementation and nutritional intake of methyl donors in patients with chronic kidney disease : a critical review of the impact on epigenetic machinery. MDPI Nutr. 2020; 12(5): 1234-53. doi:10.3390/nu12051234.
Raza ST, Singh N, Kumar D, Singh S, Chatterji T, Zaidi Z. A study to compare hemoglobin levels and body mass index in normal and diagnosed diabetic stages of CKD patients visiting a tertiary care hospital. Indian J Clin Anat Physiol. 2021; 8(3): 230-4. doi:10.18231/J.IJCAP.2021.051.
Brzózka AG, Franczyk B, Olszewski R, Rysz J. The influence of inflammation on anemia in CKD patients. Int J Mol Sci. 2020; 21(3): 725-49. doi:10.3390/IJMS21030725.
Ginting L, Aziz A, Wulandari, Lasono DB, Koerniawan D. The relationship between hemodialysis adequacy achievement and the incidence of anemia in chronic kidney disease (CKD) patients on hemodialysis at the Hemodialysis Unit, RSUP Fatmawati. Diklit RS Fatmawati Jakarta. Published online 2018; 2(2): 3-12. http://diklitrsfatmawati.com/jurnal/single.php?id=27.
Somji SS, Ruggajo P, Moledina S. Adequacy of hemodialysis and its associated factors among patients undergoing chronic hemodialysis in Dar es Salaam, Tanzania. Int J Nephrol. 2020; 2020: 1-6. doi:10.1155/2020/9863065.
Richardson SR, O’Malley GF. Glucose 6 phosphate dehydrogenase deficiency. StatPearls Publishing; 2022. Accessed July 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470315/.
Broadbent E, Wilkes C, Koschwanez H, Weinman J, Norton S, Petrie KJ. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol Heal. 2015; 30(11): 1361-85. doi:10.1080/08870446.2015.1070851.
Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014; 140(2): 511-43. doi:10.1037/a0033065.
Mollaoglu M, Candan F, Mollaoglu M. Illness perception and hopelessness in hemodialysis. Arch Clin Nephrol. 2016; 2(1): 044-8. doi:10.17352/acn.000014.