Work performance assessment in Thai homeless shelters: An exploratory factor analysis
Main Article Content
Abstract
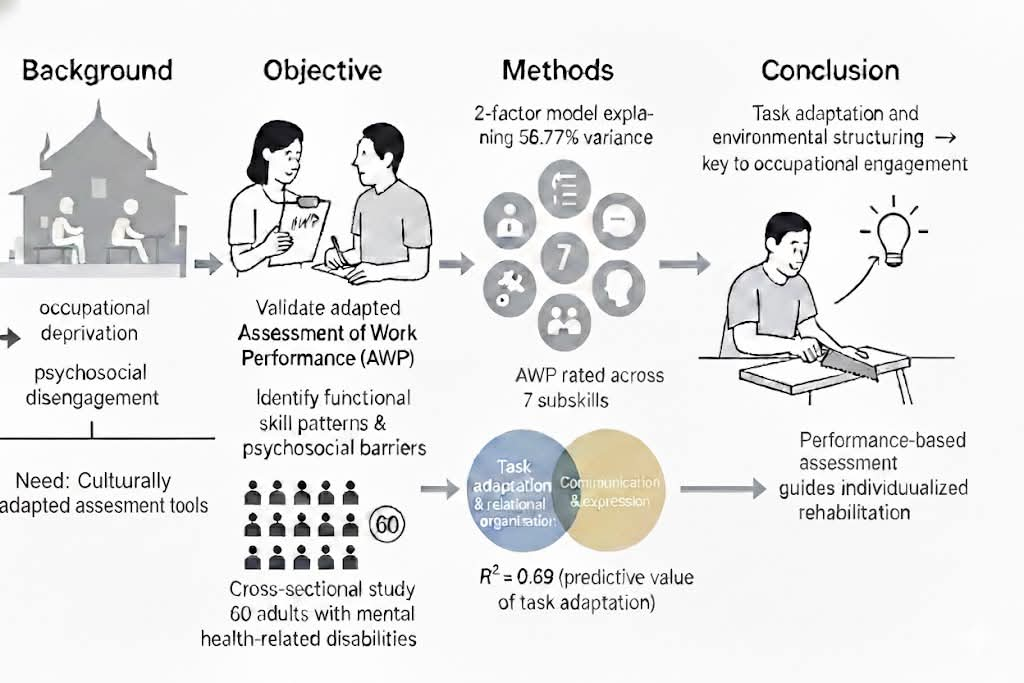
Background: Institutional sheltering can lead to occupational deprivation and psychosocial disengagement, particularly among adults with mental health-related disabilities. In Thailand, homeless shelters operate under rigid custodial systems that may hinder functional recovery, highlighting the need for culturally adapted assessment tools.
Objectives: To validate an adapted version of the Assessment of Work Performance (AWP) for use in Thai homeless shelters and to identify functional skill patterns and psychosocial barriers that inform allied health service planning.
Materials and methods: A cross-sectional study was conducted with 60 adults with mental health–related disabilities residing in a government-operated destitute shelter. Participants completed a work-based AWP task rated across seven subskills. Exploratory factor analysis (EFA) examined the underlying factor structure, while regression analysis tested the predictive value of extracted factors on occupational performance.
Results: The EFA supported a two-factor solution; 1) task adaptation and relational organization, and 2) communication and expression-accounting for 56.78% of the total variance (KMO=0.696, Bartlett’s test significant). Regression analysis showed that task adaptation and relational organization significantly predicted occupational performance, explaining 69.6% of the variance (R²=0.696).
Conclusion: Task adaptation and environmental structuring are key determinants of occupational engagement in institutional shelter settings. Performance-based assessment, combined with structured observation during task engagement, provides a culturally relevant strategy for allied health professionals to guide individualized rehabilitation for marginalized populations in Thai homeless shelters.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Gonyea JG, Mills-Dick K, Bachman SS. Enhancing occupational therapy services for homeless populations. Occup Ther Health Care. 2010; 24(1): 3-20. doi.org/10.3109/07380570903410803.
O’Neill J, Farrow T, Cramond L. Occupational therapy for people experiencing homelessness: A scoping review. Aust Occup Ther J. 2019; 66(5): 538–50. doi.org/10.1111/1440-1630.12617.
Raphael-Greenfield EI. Assessing executive and community functioning among homeless persons with substance use disorders using the EFPT. Occup Ther Ment Health. 2012; 28(2): 125-40. doi. org/10.1080/0164212X.2012.679593.
Marshall CA, Davidson L, Li A, Gewurtz R, Roy L, Barbic S, et al. Boredom and meaningful activity in adults experiencing homelessness: A mixed-methods study. Can J Occup Ther. 2019; 86(5): 357–70. doi.org/10.1177/0008417419833402.
Cunningham MJ, Slade A. Exploring the lived experience of homelessness from an occupational perspective. Scand J Occup Ther. 2019; 26(1): 19–32. doi.org/10.1080/11038128.2017.1304572.
Kirsh B, Martin L, Hultqvist J, Eklund M. Occupational therapy interventions in mental health: a literature review in search of evidence. Occup Ther Ment Health. 2019; 35(2): 109-56. doi:10.1080/0164212X.2019.1588832.
Mentrup C. The fourth edition of Gary Kielhofner’s book, Model of Human Occupation: Theory and Application. Occup Ther Health Care. 2008; 22 (2–3): 201-2. doi:10.1080/07380570801991834.
Ministry of Social Development and Human Security. Five-year strategic plan (2023–2027) [Thai]. Bangkok: Ministry of Social Development and Human Security; 2023. Available from: https://www.m-society.go.th
Sandqvist J. Development and evaluation of validity and utility of the instrument Assessment of Work Performance (AWP) [dissertation]. Linköping: Linköping University; 2007. Available from: https://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-10577
Sandqvist J, Henriksson C, Törnquist K. Validity of the Swedish version of the Assessment of Work Performance. Scand J Occup Ther. 2010; 17(1): 30–8. doi.org/10.3109/11038120903047386.
Yang Y, Hu L, Ng SM. Enhancing occupational identity and self-regulation through narrative-based OT in cancer care. Hong Kong J Occup Ther. 2020; 33(1): 19–26. doi.org/10.1177/1569186120917893.
Marshall CA, Boland L, Westover LA, Isard R, Gutman SA. A systematic review of occupational therapy interventions in the transition from homelessness. Scand J Occup Ther. 2021; 28(3): 171–87. doi.org/10.1177/0008417419833402.
O’Shaughnessy BR, Greenwood RM. Empowering features and outcomes of homeless interventions: A systematic review and narrative synthesis. Am J Community Psychol. 2020; 66(1–2): 144–65. doi.org/10.1002/ajcp.12422.
Waddell A, Kunstler B, Lennox A, Pattuwage L, Grundy EA, Tsering D, Olivier P, Bragge P. How effective are interventions in optimizing workplace mental health and well-being? A scoping review of reviews and evidence map. Scand J Work Environ Health. 2023; 49(4): 235–48. doi:10.5271/sjweh.4087.
Rider JV, Selim J, Garcia A. Health and disability among persons experiencing homelessness. Occup Ther Ment Health. 2022; 38(1): 49–66. doi.org/10.1080/0164212X.2021.1975010.
Menon J, Kantipudi SJ, Mani A, Radhakrishnan R. Cognitive functioning and functional ability in women with schizophrenia and homelessness. Schizophr Res Cogn. 2025; 39: 100338. doi.org/10.1016/j.scog.2024.100338.
MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychol Methods. 1999; 4(1): 84-99. doi:10.1037/1082-989X.4.1.84.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. doi:10.1176/appi.books.9780890425596.
Storey JE, Rowland JT, Basic D, Conforti DA, Dickson HG. The Rowland Universal Dementia Assessment Scale (RUDAS): A multicultural cognitive assessment scale. Int Psychogeriatr. 2004; 16(1): 13–31. doi:10.1017S1041610204000043.
Limpawattana P, Tiamkao S, Sawanyawisuth K, Thinkhamrop B. Can Rowland Universal Dementia Assessment Scale replace MMSE for dementia screening in Thai geriatric outpatient setting? Am J Alzheimers Dis Other Demen. 2012; 27(4): 254–9. doi.org/10.1177/1533317512447886.
Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962; 10(3): 799–812. doi.org/10.2466/pr0.1962.10.3.799.
Kittirattanapiboon P. Brief psychiatric rating scale (BPRS). Chiang Mai: Suanprung Psychiatric Hospital; 2001.
Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “the drift busters.” Int J Methods Psychiatr Res. 1993; 3(4): 221-44. Available from: https://psycnet.apa.org/record/1994-27973-001
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis. Struct Equ Modeling. 1999; 6(1): 1–55. doi.org/10.1080/10705519909540118.
Kline RB. Principles and practice of structural equation modeling. 5th ed. New York: Guilford Press; 2023.
Wolf EJ, Harrington KM, Clark SL, Miller MW. Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educ Psychol Meas. 2013; 73(6): 913–34. doi.org/10.1177/0013164413495237.
Piskur B, Magasi S, Holzemer W. Environmental factors influencing occupational performance among people with psychiatric disability. Scand J Occup Ther. 2020; 27(4): 280–90. doi.org/10.1080/11038128.2019.1572164.
Baum CM, Connor LT, Morrison T, Hahn M, Dromerick A. Reliability, validity, and clinical utility of the Executive Function Performance Test. Am J Occup Ther. 2008; 62(4): 446–55. doi.org/10.5014/ajot.62.4.446.
Cogan AM, Hatton C, Oldreive W. Identifying rehabilitation priorities in a mental health recovery setting: The role of occupational therapy. Br J Occup Ther. 2021; 84(2): 84–92. doi.org/10.1177/0308022620930523.
Marshall CA, Davidson L, Li A, Gewurtz R, Roy L, Barbic S, Kirsh B, Lysaght R. Boredom and meaningful activity in adults experiencing homelessness: A mixed-methods study. Can J Occup Ther. 2019; 86(5): 357–70. doi:10.1177/0008417419833402.
Katz N, Tadmor I, Felzen B, Hartman-Maeir A. Validity of the Executive Function Performance Test in people with schizophrenia. OTJR (Thorofare N J). 2011; 31(1): 17–23. doi.org/10.3928/15394492-20100510-01.
Mursaleen MH, Begum N, Arain T, Ali SA, Lakhani U, Iqbal B. Efficacy of occupational therapy interventions in improving cognitive function and daily living skills among individuals with substance use disorder. Allied Med Res J. 2025; 3(1): 110–5. Available from: https://ojs.amrj.net/index.php/1/article/view/248
Yan Y, Leung M, Dey A. Factors affecting retention of occupational therapists in adult mental health services: A systematic review.
Br J Occup Ther. 2024; 87(2): 89–102. doi. org/10.1177/03080226231111620.
Mello ACC, Araujo AS, Costa ALB, Marcolino TQ. Meaning-making in occupational therapy interventions: A scoping review. Cad Bras Ter Ocup. 2021; 29: e2859. doi.org/10.1590/2526-8910.ctoAR2158.
Honey A, Fortune T, Karanikolas A, Morris A. Hope-promoting practices in occupational therapy: Insights from people experiencing homelessness. Aust Occup Ther J. 2023; 70(4): 435–46. doi.org/10.1111/1440-1630.12869.