The reliability and validity of the Thai version of Visual Cognitive Assessment Test (VCAT:Th )
Main Article Content
Abstract
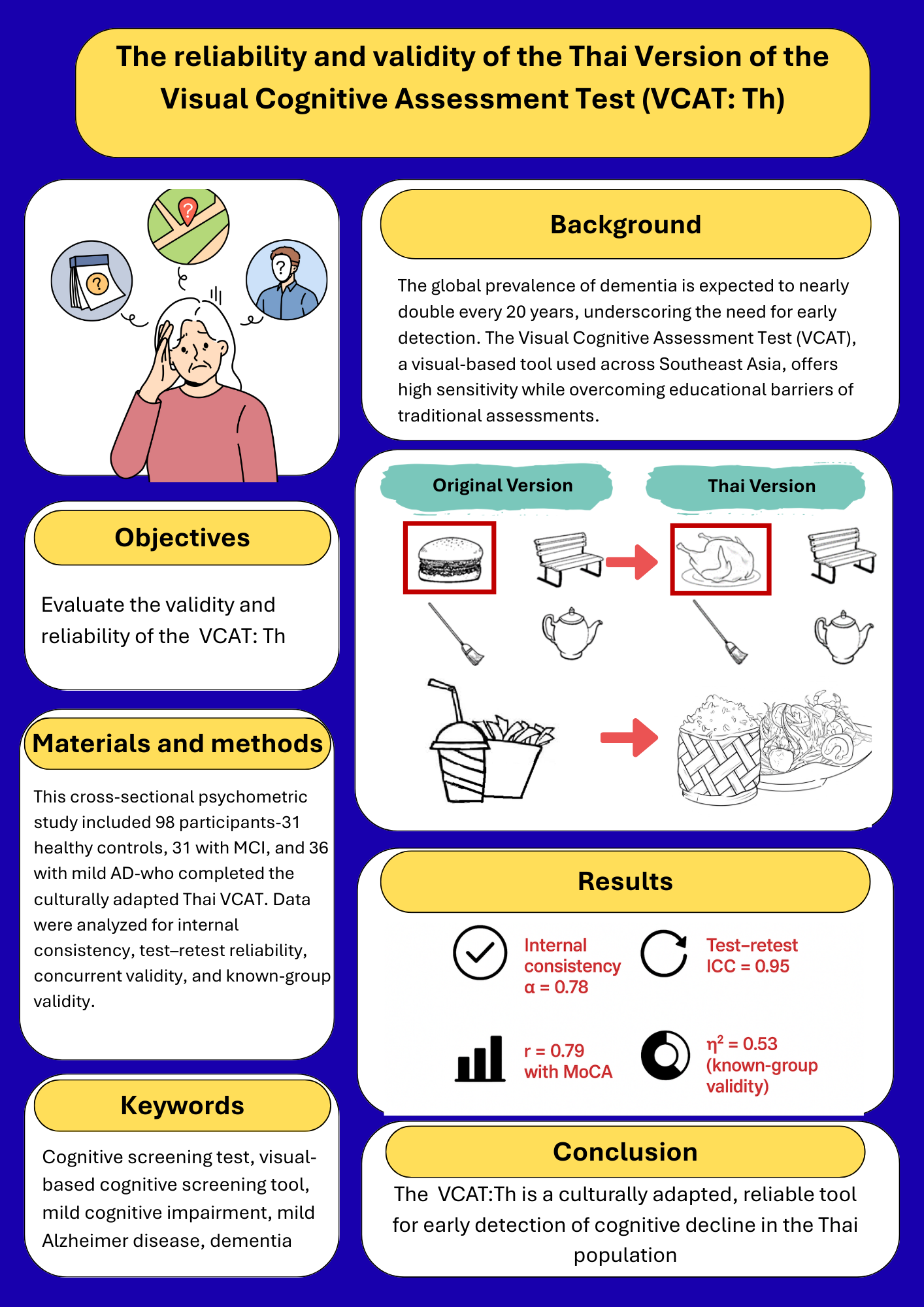
Background: The global prevalence of dementia is projected to nearly double every 20 years, significantly impacting the quality of life for both individuals with dementia and their caregivers. Early detection is therefore critical, particularly in the context of Thailand’s rapidly aging population. The Visual Cognitive Assessment Test (VCAT) is a visual-based cognitive screening tool designed to overcome educational limitations commonly associated with traditional assessments. Widely adopted across Southeast Asia, the VCAT demonstrates high sensitivity in detecting cognitive impairments from the earliest stages.
Objectives: This study aims to evaluate the validity and reliability of the Thai version of the Visual Cognitive Assessment (VCAT: Th)
Materials and methods: This study employed a cross-sectional, psychometric design and included 98 participants, consisting of 31 healthy controls (HC), 31 individuals with mild cognitive impairment (MCI), and 36 individuals with mild Alzheimer’s disease (AD). The HC group was recruited from community-dwelling individuals residing in Bangkok and its surrounding metropolitan areas, while the MCI and mild AD groups were recruited from the Faculty of Medicine Ramathibodi Hospital, Mahidol University. All participants completed the Thai version of the Visual Cognitive Assessment Test (VCAT: Th), which was culturally adapted from the original version to suit the Thai context. The collected data was then used to evaluate internal consistency, test–retest reliability, concurrent validity, and known-group validity.
Results: The VCAT: Th demonstrated strong psychometric properties. Internal consistency was highly acceptable (α=0.78), and test-retest reliability was excellent (ICC=0.95). Concurrent validity showed a strong and significant correlation with MoCA scores (r=0.79,p<0.001). Known-group validity revealed significant group differences with a large effect size (η²=0.53).
Conclusion: The VCAT: Th is a culturally adapted cognitive assessment tool that effectively identifies impairments typically present in the early stages of cognitive decline. It demonstrates acceptable psychometric properties and is appropriate for use within the Thai population.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
World Health Organization. Dementia in refugees and migrants: epidemiology, public health implications and global responses. Geneva: World Health Organization; 2024.
Aretouli E, Brandt J. Everyday functioning in mild cognitive impairment and its relationship with executive cognition. Int J Geriatr Psychiatry. 2010; 25(3): 224-33.doi: 10.1002/gps.2325.
Chang CW, Su KC, Lu FC, Cheng HM, Cheng CY. Visual function and visual perception among senior citizens with mild cognitive impairment in Taiwan. Healthcare (Basel). 2021; 10(1): 20. doi: 10.3390/healthcare10010020.
Feng YR, Meuleners L, Stevenson M, Heyworth J, Murray K, Fraser M, et al. The impact of cognition and gender on speeding behaviour in older drivers with and without suspected mild cognitive impairment. NPJ Aging. 2021; 16: 1473-83.doi: 10.2147/cia.S319129.
Bennett S, Laver K, Voigt-Radloff S, Letts L, Clemson L, Graff M, et al. Occupational therapy for people with dementia and their family carers provided at home: a systematic review and meta-analysis. BMJ open. 2019; 9(11): e026308. doi: 10.1136/bmjopen-2018-026308.
Graff MJL, Vernooij-Dassen MJM, Thijssen M, et al. Community based occupational therapy for patients with dementia and their care givers: randomised controlled trial. BMJ. 2006; 333(7580): 1196. doi: 10.1136/bmj.39001.688843.BE.
Kandiah N, Zhang A, Bautista DC, Silva E, Ting SKS, Ng A, et al. Early detection of dementia in multilingual populations: Visual Cognitive Assessment Test (VCAT). J Neurol Neurosurg Psychiatry. 2016; 87(2): 156-60. doi: 10.1136/jnnp-2014-309647.
Lim L, Ng TP, Ong AP, Tan MP, Cenina AR, Gao Q, et al. A novel language-neutral Visual Cognitive Assessment Test (VCAT): validation in four Southeast Asian countries. Alzheimers Res Ther. 2018;10(1): 6. doi: 10.1186/s13195-017-0333-z.
Ng KP, Ong GCF, Saffari SE, Bernardes MM, de Carvalho AB, Schilling LP, et al. Visual Cognitive Assessment Test (VCAT): A language-neutral test to detect mild cognitive impairment and dementia in multinational cohorts. Alzheimers Dement. 2024; 20(S3): e090328. doi: 10.1002/alz.090328.
Low A, Lim L, Lim L, Wong B, Silva E, Ng KP, et al. Construct validity of the Visual Cognitive Assessment Test (VCAT)-a cross-cultural language-neutral cognitive screening tool. Int Psychogeriatr. 2020; 32(1): 141-9. doi: 10.1017/s1041610219000504.
Ng Y, Chin CJ, Danial M, Albart S, Suppiah PD, Ganasegeran K,et al. Validation of the Visual Cognitive Assessment Test (VCAT) for the early diagnosis of cognitive impairment in multilingual population in Malaysia. Psych. 2022; 4(1): 38-48. doi: 10.3390/psych4010003.
American Psychiatric Association. Diagnostic and statistical manual of mental disorder [cited 2024 December 11]. Available from: https://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011; 7(3): 270-9. doi: 10.1016/j.jalz.2011.03.008.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr., Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011; 7(3): 263-9. doi: 10.1016/j.jalz.2011.03.005.
Lim L, Ng TP, Ong AP, Tan MP, Cenina AR, Gao Q, et al. A novel language-neutral Visual Cognitive Assessment Test (VCAT): validation in four Southeast Asian countries. Alzheimers Res Ther. 2018;10(1):6. doi: 10.1186/s13195-017-0333-z.
Waltz CF, Strickland OL, Lenz ER. Measurement in nursing and health research. (5th Ed.). New York: Springer Publishing Company; 2016.
Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychol Bull. 1979; 86(2): 420-8. doi: 10.1037/0033-2909.86.2.420.
Taber KS. The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018; 48(6): 1273-96.doi: 10.1007/s11165-016-9602-2.
Koo TK, Li MY. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2): 155-63.doi: https://doi.org/10.1016/j.jcm.2016.02.012.
Prion S, Haerling KA. Making sense of methods and measurement: Spearman-Rho ranked-order correlation coefficient. Clin Simul Nurs. 2014; 10(10): 535-6.doi: 10.1016/j.ecns.2014.07.005.
Heesch KC, Mâsse LC. Lack of time for physical activity: perception or reality for African American and Hispanic women? Women Health. 2004; 39(3): 45-62. doi: 10.1300/J013v39n03_04.
Daga M, Mohanty P, Krishna R, Priya S. Statistical validation in cultural adaptations of cognitive tests: a multi-regional systematic review. arXiv [Preprint]. 2025. doi:https://doi.org/10.48550/arXiv.2504.13495.
Frtusova J, Rivest J, Doody A, Leach L. Selective and divided visual attention in mild cognitive impairment as measured with the Baycrest Attention Test and Traditional Neuropsychological Tests. Alzheimers Dement. 2010; 6: e30-e30. doi: 10.1016/j.jalz.2010.08.095.
Alescio-Lautier B, Michel BF, Herrera C, Elahmadi A, Chambon C, Touzet C, et al. Visual and visuospatial short-term memory in mild cognitive impairment and Alzheimer disease: Role of attention. Neuropsychologia. 2007; 45(8): 1948-60.doi: https://doi.org/10.1016/j.neuropsychologia.2006.04.033.
Oltra-Cucarella J, Sánchez-SanSegundo M, Lipnicki DM, Crawford JD, Lipton RB, Katz MJ, et al. Visual memory tests enhance the identification of amnestic MCI cases at greater risk of Alzheimer’s disease. Int Psychogeriatr. 2019; 31(7): 997-1006. doi: 10.1017/s104161021800145x.
Mueller KD, Hermann B, Mecollari J, Turkstra LS. Connected speech and language in mild cognitive impairment and Alzheimer’s disease: A review of picture description tasks. J Clin Exp Neuropsychol. 2018; 40(9): 917-39.doi: 10.1080/13803395.2018.1446513.
Jung YH, Park S, Jang H, Cho SH, Kim SJ, Kim JP, et al. Frontal-executive dysfunction affects dementia conversion in patients with amnestic mild cognitive impairment. Sci Rep. 2020; 10(1): 772. doi: 10.1038/s41598-020-57525-6.
Reinvang I, Grambaite R, Espeseth T. Executive dysfunction in MCI: Subtype or early symptom. Int J Alzheimers Dis. 2012; 2012 :936272. doi: 10.1155/2012/936272.
Brandt J, Aretouli E, Neijstrom E, Samek J, Manning K, Albert MS, et al. Selectivity of executive function deficits in mild cognitive impairment. Neuropsychology. 2009; 23(5): 607-18. doi: 10.1037/a0015851.
Oh H, Madison C, Haight TJ, Markley C, Jagust WJ. Effects of age and β-amyloid on cognitive changes in normal elderly people. Neurobiol Aging. 2012; 33(12): 2746-55. doi: 10.1016/j.neurobiolaging.2012.02.008.