A review on the prevalence of unexpected alloantibodies in Thai patients across Thailand
Main Article Content
Abstract
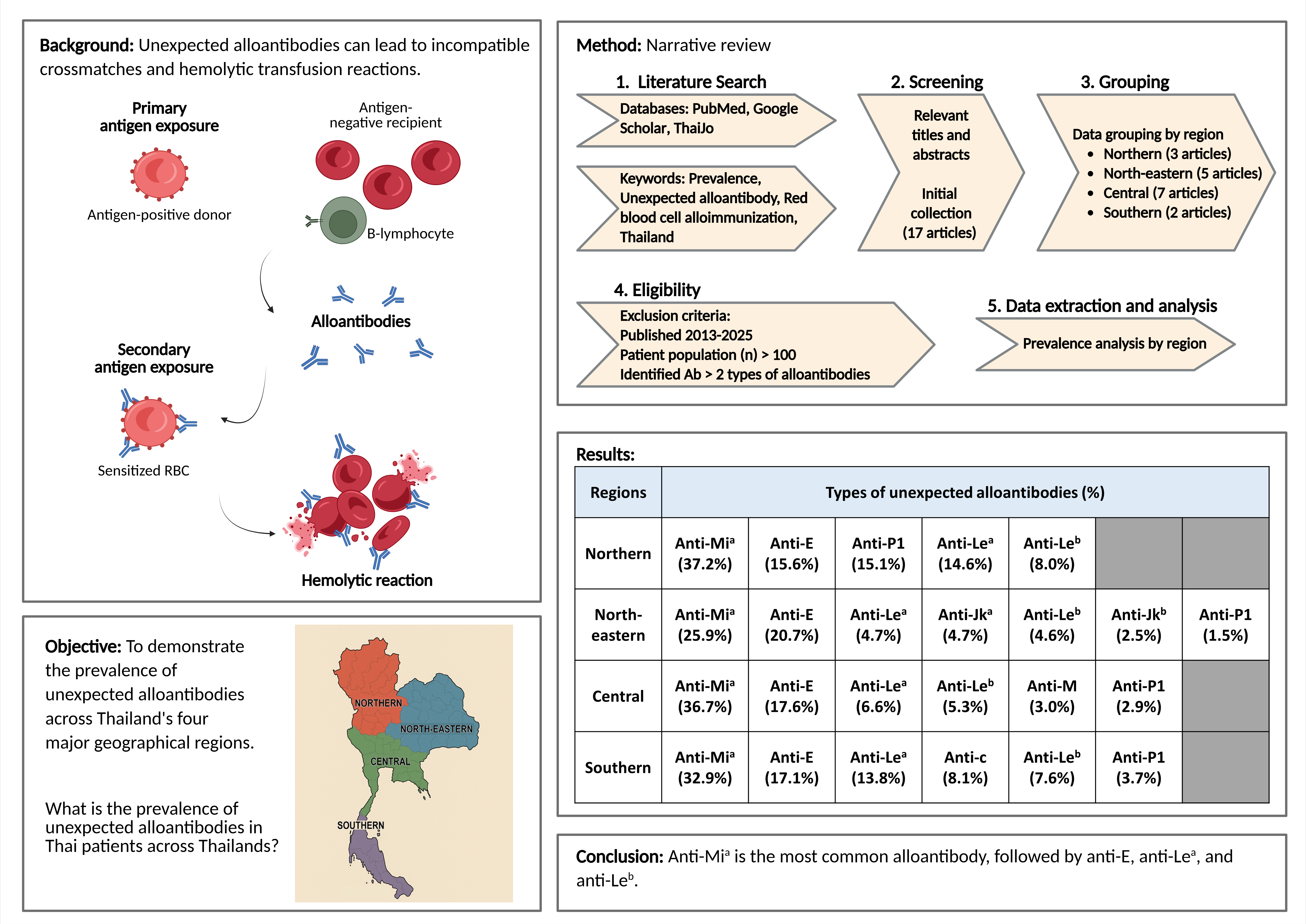
Background: Alloantibodies are immune responses produced by exposure to foreign red blood cell antigens. However, sensitized alloantibodies can lead to hemolytic transfusion reactions and complicate cross-matching procedures.
Objectives: This review article aims to demonstrate the prevalence of unexpected alloantibodies across Thailand’s four major geographical regions.
Materials and methods: A comprehensive literature search was conducted across PubMed, Google Scholar, and ThaiJo databases using keywords related to unexpected alloantibodies in Thailand, yielding 17 articles categorized by geographical region. Studies were filtered using strict criteria (published 2013-2025, sample size > 100, reporting > 2 alloantibody types) for final data analysis.
Results: It is revealed that anti-Mia is the highest unexpected alloantibody, with a prevalence rate of 25.9-37.2% across all four regions, followed by anti-E (15.6-20.7%), anti-Lea (4.7-14.6%), and anti-Leb (4.6-8.0%), respectively. Interestingly, anti-P1 is remarkably increased in the Northern region (15.1%), whereas anti-Jka (4.7%) and anti-Jkb (2.5%) are specifically higher in the Northeastern region.
Conclusion: This review highlights the importance of practicing antibody screening protocols, choosing compatible antigen status, and establishing rare donor registries in Thailand to avoid unexpected alloimmunization, thereby ensuring optimal transfusion safety.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Talukdar B, Bhattacharya P. Novel aspects in blood transfusion – From donor to patient. J Hematol Allied Sci. 2025; 5(1): 18-25. doi:10.25259/ JHAS_66_2024.
Tenorio GC, Gupte SC, Munker R. Transfusion Medicine and Immunohematology. In: Munker R, Hiller E, Glass J, Paquette R, Editors. Modern Hematology: Biology and Clinical Management. New Jersey: Humana Press; 2007: pp 401-32. doi: 10.1007/978-1-59745-149-9_22.
Daniels G, Poole J, De Silva M, Callaghan T, MacLennan S, Smith N. The clinical significance of blood group antibodies. Transfus Med. 2002; 12(5): 287-95. doi: 10.1046/j.1365-3148.2002.00399.x.
Pham BN, Le Pennec PY, Rouger P. Allo-immunisation anti-érythrocytaire. Transfus Clin Biol. 2012; 19(6): 321-32. doi: 10.1016/j.tracli.2012.06.007.
Schonewille H, Van De Watering LMG, Loomans DSE, Brand A. Red blood cell alloantibodies after transfusion: factors influencing incidence and specificity. Transfusion. 2006; 46(2): 250-6. doi: 10.1111/j.1537-2995.2006.00708.x.
Tormey CA, Hendrickson JE. Transfusion-related red blood cell alloantibodies: induction and consequences. Blood. 2019; 133(17): 1821-30. doi: 10.1182/blood-2018-08-833962.
Yang S, Yang HJ, Park HJ, Kwon SW. The Frequency and distribution of unexpected red Cell Antibodies and Analysis of Antigen Exposure. Korean J Clin Lab Sci. 2014; 45: 164-9.
Kahar MA, Patel RD. Phenotype frequencies of blood group systems (Rh, Kell, Kidd, Duffy, MNS, P, Lewis, and Lutheran) in blood donors of south Gujarat, India. Asian J Transfus Sci. 2014; 8(1): 51-5. doi: 10.4103/0973-6247.126693.
Hickey MJ, Valenzuela NM, Reed EF. Alloantibody Generation and Effector Function Following Sensitization to Human Leukocyte Antigen. Front Immunol. 2016; 7(2016): 00030. doi: 10.3389/f immu.2016.00030.
Tinckam KJ, Chandraker A. Mechanisms and role of HLA and non-HLA alloantibodies. Clin J Am Soc Nephrol. 2006; 1(3): 404-14. doi: 10.2215/CJN.00270106.
Zerra PE, Josephson CD. Chapter 73 - Delayed Hemolytic Transfusion Reactions. In: Shaz BH, Hillyer CD, Schwartz J, Gil MR, editors. Transfusion Medicine and Hemostasis. 4th ed. New York: Elsevier; 2025: pp 343-5. doi: 10.1016/B978-0- 323-96014-4.00087-2.
Panch SR, Montemayor-Garcia C, Klein HG. Hemolytic Transfusion Reactions. N Engl J Med. 2019; 381(2): 150-62. doi: 10.1056/NEJMra1802338.
Bhuva DK, Vachhani JH. Red cell alloimmunization in repeatedly transfused patients. Asian J Transfus Sci. 2017; 11(2): 115-20. doi: 10.4103/0973-6247.214347.
Delaney M, Matthews DC. Hemolytic disease of the fetus and newborn: managing the mother, fetus, and newborn. Hematology Am Soc Hematol Educ Program. 2015; 2015(1): 146-51. doi: 10.1182/asheducation-2015.1.146
Arinsburg SA. Chapter 21 - Pretransfusion Testing. In: Shaz BH, Hillyer CD, Reyes Gil M, editors. Transfusion Medicine and Hemostasis. 3rd ed. New York: Elsevier; 2019: pp 107-16. doi: 10.1016/ B978-0-12-813726-0.00021-0.
Saviano A, Perotti C, Zanza C, Longhitano Y, Ojetti V,Franceschi F, et al. Blood Transfusion for Major Trauma in Emergency Department. Diagnostics. 2024; 14(7): 708. doi: 10.3390/ diagnostics14070708.
Thai Red Cross Society, National Blood Centre. Blood Administration and Monitoring. In: Pimol C, Sasitorn B, Aphisit T, editors. The Appropriate Use of Blood and Blood Components. 2nd ed. Bangkok: Pimnaphat; 2023: pp 40-1.
Thai Red Cross Society, National Blood Center. Compatibility testing and selection of components. In: Pimol C, Sasitorn B, Aphisit T, editors. Standards for blood banks and transfusion service. 5th ed. Bangkok: Udomsuksa; 2024: pp 83-8.
Kahar MA. Formulation of in-house screening and panel red cell for red cell antibody detection and identification in blood recipients: How to do it? J Hematol Allied Sci. 2024; 4(3): 94-102. doi: 10.25259/JHAS_43_2024.
Chang Y-J, Ho C-Y, Zhou X-M, Yen H-R. Determination of degree of RBC agglutination for blood typing using a small quantity of blood sample in a microfluidic system. Biosens Bioelectron. 2018; 102: 234-41. doi: 10.1016/j.bios.2017.11.008.
Johnson ST, Puca KE. Evaluating patients with autoimmune hemolytic anemia in the transfusion service and immunohematology reference laboratory: pretransfusion testing challenges and best transfusion-management strategies. Hematology Am Soc Hematol Educ Program. 2022; 2022(1): 96-104. doi: 10.1182/hematology.2022000406.
Butryojantho C, Junta N, Pimphumee R, Srichai S, Darunikorn P, Puapairoj C, et al. Antibody screening and the prevalence of unexpected antibodies in the patients of Srinagarind Hospital. J Hematol Transfus Med. 2017; 27(1): 27-33 (in Thai).
Daowsee K, Urwijitaroon Y. Red cell alloantibodies in transfused patients detected by standard tube test and column gel agglutination: A Study for Improving Transfusion Service. J Hematol Transfus Med. 2013; 23(4): 269-76 (in Thai).
Po-ngernnak P, Sasjeenpong S, Chuesakul K, Pangwangthong K. The Prevalence of Red Blood Cell Alloantibodies in Lower Northern Thailand. J Med Assoc Thai. 2016; 99(12): 1337-43. PMID: 29952524.
Promwong C, Siammai S, Hassarin S, Buakaew J, Yeela T, Soisangwan P, et al. Frequencies and specificities of red cell alloantibodies in the Southern Thai population. Asian J Transfus Sci. 2013; 7(1): 16-20. doi: 10.4103/0973-6247.106718.
Rattakul A, Intharanut K, Nathalang O. The prevalence of red cell antibodies among patients and pregnant women in Pakchongnana Hospital. J Hematol Transfus Med. 2019; 29(4): 317-24 (in Thai).
Rungroung T, Vejbaesya S, Rodpong P, Pimsamsee W, Chongkolwatana V. Red cell phenotyping in blood donors to provide safe blood transfusion for transfused patients at Siriraj Hospital. J Hematol Transfus Med. 2018; 28(4): 423-30 (in Thai).
Thompat W, Boonpradit P, Wisetwut P, Oparatchatawat C, Srijinda S. The prevalence of unexpected antibodies in transfused cancer patients at National Cancer Institute. J Hematol Transfus Med. 2022; 32(4): 299-306 (in Thai).
Romphruk A, Butryojantho C, Jirasakonpat B, Junta N, Srichai S, Puapairoj C, et al. Phenotype frequencies of Rh (C, c, E, e), M, Mia and Kidd blood group systems among ethnic Thai blood donors from the north-east of Thailand. Int J Immunogenet. 2019; 46(3): 160-5. doi: 10.1111/iji.12420.
Toompokalang S, Peangchaiyaphoom N, Suwanwootichai P. C, E, c, e and Mia antigen test using Ortho Vision Max automated analyzer in blood donors at the Regional Blood Centre III, Chonburi province. J Hematol Transfus Med. 2023; 33(1): 21-7 (in Thai).
Agrawal S, Chowdhry M. A case report on anti-Mia antibody in a multi-transfused patient from India. Transfus Apher Sci. 2019; 58(5): 625-7. doi: 10.1016/j.transci.2019.08.027.
Pahuja S, Sehgal S, Sharma G, Singh M, Yadav R. The anti-Mia antibody – Report of four cases in a tertiary care hospital with review of literature. Glob J Transfus Med. 2019; 4(1): 79-83. doi: 10.4103/gjtm.gjtm_2_19.
Reid ME, Storry JR. Low-incidence MNS antigens associated with single amino acid changes and their susceptibility to enzyme treatment. Immunohematology. 2001; 17(3): 76-81. doi: 10.21307/immunohematology-2019-551.
Cheepsattayakorn R, Fongsatitkul L, Chotinaruemol S, Mahawongtong M. Anti-E as a cause of hemolytic disease of the newborn. J Med Assoc Thai. 1997; 80 Suppl 1: S1-4. PMID: 9347637.
Usman ASi, Mustaffa R, Ramli N, Diggi SA. Hemolytic disease of the fetus and newborn caused by anti-E. Asian J Transfus Sci. 2013; 7(1): 84-5. doi: 10.4103/0973-6247.106750.
Joy SD, Rossi KQ, Krugh D, O’Shaughnessy RW. Management of pregnancies complicated by anti-E alloimmunization. Obstet Gynecol. 2005; 105(1): 24-8. doi: 10.1097/01.aog.0000149153.93417.66.
Michalewska B, Ejduk A, Pniewska K. Acute haemolytic transfusion reaction apparently caused by the ‘enzyme-only’ anti-E. Vox Sang. 2005; 89(1):61-1. doi: 10.1111/j.1423-0410.2005.00641.x.
Combs MR. Lewis blood group system review. Immunohematology. 2009; 25(3): 112-8. doi: 10.21307/immunohematology-2019-243.
Nanakorn N, Boonthongkhao S, Mitundee S, Tonwong N. Prevalence of Lewis blood group polymorphisms in Southern Thai blood donors. J Health Sci Med Res. 2022; 40(4): 10. doi: 10.31584/jhsmr.2021847.
Nathalang O, Kuvanont S, Punyaprasiddhi P,Tasaniyanonda C, Sriphaisal T. A preliminary study of the distribution of blood group systems in Thai blood donors determined by the gel test. Southeast Asian J Trop Med Public Health. 2001; 32(1): 204-7. PMID: 11485086.
Subramaniyan R. Serological characteristics of Lewis antibodies and their clinical significance – A case series. Hematol Transfus Cell Ther. 2023; 45(2): 159-64. doi: 10.1016/j.htct.2021.07.007.
Kijkornpan S, Suebsaeng C, Chiewsilp P. Lewis antigens on newborn red cells. J Med Assoc Thai. 2000; 83(Suppl 1): S46-8. PMID: 10865406.
Karnes JH, Miller MA, White KD, Konvinse KC, Pavlos RK, Redwood AJ, et al. Applications of Immunopharmacogenomics: Predicting, Preventing, and Understanding Immune-Mediated Adverse Drug Reactions. Annu Rev Pharmacol Toxicol. 2019; 59: 463-86. doi: 10.1146/annurev-pharmtox010818-021818.
Moncharmont P, Barday G, Meyer F. Red blood cell alloimmunisation in 18 to 50-year old transfused women: a 3-year study. Blood Transfus. 2015; 13(2): 345-6. doi: 10.2450/2014.0211-14.
Moncharmont P, Barday G, Py JY, Meyer F.Acquired red blood cell alloantibodies in transfused patients of 80 years or over: a 2008-2013 national haemovigilance survey. Blood Transfus. 2017; 15(3): 254-8. doi: 10.2450/2016.0328-15.
Dogra A, Sidhu M, Kapoor R, Kumar D. Study of red blood cell alloimmunization in multitransfused thalassemic children of Jammu region. Asian J Transfus Sci. 2015; 9(1): 78-81. doi: 10.4103/0973-6247.150958.
Fluit CRMG, Kunst VAJM, Drenthe-Schonk AM. Incidence of red cell antibodies after multiple blood transfusion. Transfusion. 1990; 30(6): 532-5. doi: 10.1046/j.1537-2995.1990.30690333485.x.
Park HS, Shin KS, Son BR. Incidence of red blood cell alloantibody formation after platelet concentrate transfusions. Korean J Blood Transfus. 2019; 30(1): 33-41. doi: 10.17945/kjbt.2019.30.1.33.
Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. 2010; 63(6): 425-33. doi: 10.1111/j.1600-0897.2010.00836.x.
Westhoff CM. Molecular testing for transfusion medicine. Curr Opin Hematol. 2006; 13(6): 471-5. doi: 10.1097/01.moh.0000245695.77758.3d.
Shah A, Shah D, Shah D, Chordiya D, Doshi N, Dwivedi R. Blood bank management and inventory control database management system. Procedia Comput Sci. 2022; 198: 404-9. doi: 10.1016/j.procs.2021.12.261.
Raja ML, Musi R, Fattorini M, Piva E, Putoto G. Point of care Testing and transfusion safety in resource limited settings: A review. J Blood Disorders Transf. 2015; 6(2): 1000269. doi: 10.4172/2155-9864.1000269.
Sarkar S. Artificial blood. Indian J Crit Care Med. 2008; 12(3): 140-4. doi: 10.4103/0972-5229.43685.
Gammon RR, Dubey R, Gupta GK, Hinrichsen C, Jindal A, Lamba DS, et al. Patient Blood Management and Its Role in Supporting Blood Supply. J Blood Med. 2023; 14: 595-611. doi: 10.2147/jbm.S387322.
Thirunavukkarasu J, Subinesh KJ, Dharshan P, Boobesh S, Editors. A smart blood donor locator and component matching system for rapid disaster response. 2023 International Conference on Innovative Computing, Intelligent Communication and Smart Electrical Systems (ICSES); 2023: 1-7. doi: 10.1109/ICSES60034.2023.10465383.