A systematic review of the effect of the integration of speech therapy with music therapy on swallowing for patients with Parkinson’s disease
Main Article Content
Abstract
Background: Dysphagia, or swallowing impairment, is a common complication in individuals with Parkinson’s disease. Speech therapy is a non-pharmacological intervention that employs behavioral techniques to address this condition. A growing body of research also suggests that music therapy may have beneficial effects on swallowing function in this population. However, the effectiveness of integrating speech and music therapy for improving swallowing in individuals with Parkinson’s disease has not yet been systematically evaluated.
Objectives: The objective of this systematic review was to examine the effectiveness of integrating speech therapy with music therapy for swallowing in patients with Parkinson’s disease.
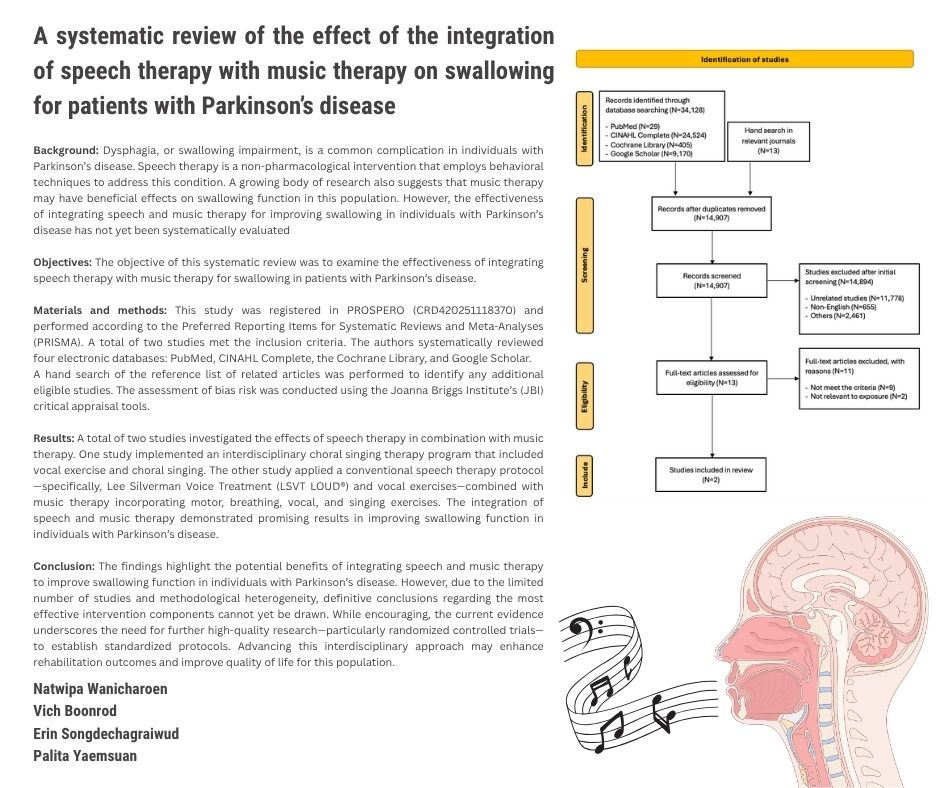
Materials and methods: This study was registered in PROSPERO (CRD420251118370) and performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A total of two studies met the inclusion criteria. The authors systematically reviewed four electronic databases: PubMed, CINAHL Complete, the Cochrane Library, and Google Scholar. A hand search of the reference list of related articles was performed to identify any additional eligible studies. The assessment of bias risk was conducted using the Joanna Briggs Institute’s (JBI) critical appraisal tools.
Results: A total of two studies investigated the effects of speech therapy in combination with music therapy. One study implemented an interdisciplinary choral singing therapy program that included vocal exercise and choral singing. The other study applied a conventional speech therapy protocol-specifically, Lee Silverman Voice Treatment (LSVT LOUD®) and vocal exercises-combined with music therapy incorporating motor, breathing, vocal, and singing exercises. The integration of speech and music therapy demonstrated promising results in improving swallowing function in individuals with Parkinson’s disease.
Conclusion: The findings highlight the potential benefits of integrating speech and music therapy to improve swallowing function in individuals with Parkinson’s disease. However, due to the limited number of studies and methodological heterogeneity, definitive conclusions regarding the most effective intervention components cannot yet be drawn. While encouraging, the current evidence underscores the need for further high-quality research particularly randomized controlled trials to establish standardized protocols. Advancing this interdisciplinary approach may enhance rehabilitation outcomes and improve quality of life for this population.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Marras C, Beck JC, Bower JH, et al. Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018; 4: 21. doi:10.1038/s41531-018-0058-0.
Parkinson’s disease: Causes, symptoms, and treatments. National Institute of Aging. 2022. https://www.nia.nih.gov/health/parkinsons-disease/parkinsons-disease-causes-symptoms-and-treatments. (accessed Dec 23, 2024).
Durcan R, Wiblin L, Lawson RA, et al. Prevalence and duration of non-motor symptoms in prodromal Parkinson’s disease. Eur J Neurol. 2019; 26(7): 979-85. doi:10.1111/ene.13919.
Sung HY, Kim JS, Lee KS, et al. The prevalence and patterns of pharyngoesophageal dysmotility in patients with early-stage Parkinson’s disease. Mov Disord. 2010; 25(14): 2361-8. doi:10.1002/mds.23290.
Ertekin C, Tarlaci S, Aydogdu I, et al. Electrophysiological evaluation of pharyngeal phase of swallowing in patients with Parkinson’s disease. Mov Disord. 2002; 17(5): 942-9. doi:10.1002/mds.10240.
Tjaden K. Speech and swallowing in Parkinson’s disease. Top Geriatr Rehabil. 2008; 24(2): 115-26. doi:10.1097/01.TGR.0000318899.87690.44.
Patel B, Legacy J, Hegland KW, Okun MS, Herndon NE. A comprehensive review of the diagnosis and treatment of Parkinson’s disease dysphagia and aspiration. Expert Rev Gastroenterol Hepatol. 2020; 14(6): 411-24. doi:10.1080/17474124.2020.1769475.
Kalf JG, de Swart BJ, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord. 2012; 18(4): 311-5. doi:10.1016/j.parkreldis.2011.11.006.
Gong S, Gao Y, Liu J, et al. The prevalence and associated factors of dysphagia in Parkinson’s disease: A systematic review and meta-analysis. Front Neurol. 2022; 13: 1000527. doi:10.3389/fneur.2022.1000527.
Carneiro D, das Graças Wanderley de Sales Coriolano M, Belo LR, de Marcos Rabelo AR, Asano AG, Lins OG. Quality of life related to swallowing in Parkinson’s disease. Dysphagia. 2014; 29(5): 578-82. doi:10.1007/s00455-014-9548-3.
Chan HF, Ng ML, Kim H, Kim DY. Swallowing-related quality of life among oral-feeding Chinese patients with Parkinson’s disease - a preliminary study using Chinese SWAL-QOL. Disabil Rehabil. 2022; 44(7): 1077-83. doi:10.1080/09638288.2020.1791979.
Suttrup I, Warnecke T. Dysphagia in Parkinson’s disease. Dysphagia. 2016; 31(1): 24-32. doi:10.1007/s00455-015-9671-9.
Robertson C, Thomson F. Speech therapy in Parkinson’s disease: a study of the efficacy and long-term effects of intensive treatment. Br J Disord Commun. 1984; 19(3): 213-24. doi: 10.3109/13682828409029837.
El Sharkawi A, Ramig L, Logemann JA, Pauloski BR, Rademaker AW, Smith CH, et al. Swallowing and voice effects of Lee Silverman Voice Treatment (LSVT®): a pilot study. J Neurol Neurosurg Psychiatry. 2002; 72(1): 31-6.
Russell JA, Ciucci MR, Connor NP, Schallert T. Targeted exercise therapy for voice and swallow in persons with Parkinson’s disease. Brain Res. 2010; 1341: 3-11. doi:10.1016/j.brainres.2010.03.029.
Miles A, Jardine M, Johnston F, de Lisle M, Friary P, Allen J. Effect of Lee Silverman Voice Treatment (LSVT LOUD®) on swallowing and cough in Parkinson’s disease: A pilot study. J Neurol Sci. 2017; 383: 180-7. doi:10.1016/j.jns.2017.11.015.
Baijens LW, Speyer R. Effects of therapy for dysphagia in Parkinson’s disease: systematic review. Dysphagia. 2009; 24(1): 91-102. doi:10.1007/s00455-008-9180-1.
Stegemöller EL, Hibbing P, Radig H, Wingate J. Therapeutic singing as an early intervention for swallowing in persons with Parkinson’s disease. Complement Ther Med. 2017; 31: 127-33. doi:10.1016/j.ctim.2017.03.002.
Yeo MS, Hwang J, Lee HK, Kim SJ, Cho SR. Therapeutic singing-induced swallowing exercise for dysphagia in advanced-stage Parkinson’s disease. Front Neurol. 2024; 15: 1323703. doi:10.3389/fneur.2024.1323703.
Machado Sotomayor MJ, Arufe-Giráldez V, Ruíz-Rico G, Navarro-Patón R. Music therapy and Parkinson’s disease: A systematic review from 2015-2020. Int J Environ Res Public Health. 2021; 18(21): 11618. doi: 10.3390/ijerph182111618.
Funderburke SK. Effects of interdisciplinary choral singing on the voice and swallowing function of individuals with Parkinson’s disease [master’s thesis]. Gainesville: University of Florida; 2012.
Mohseni Z, Saffarian A, Mohamadi R, Abolghasemi J, Habibi SA. Effect of conventional speech therapy combined with music therapy on swallowing in patients with Parkinson’s disease (Telerehabilitation): a randomized-controlled trial. k. Middle East J Rehabil Health Stud 2023;10(1): e131572. doi:10.5812/mejrh-131572.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372: n71. doi:10.1136/bmj.n71.
Barker TH, Habibi N, Aromataris E, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for quasi-experimental studies. JBI Evid Synth. 2024; 22(3): 378-88. doi:10.11124/JBIES-23-00268.
Barker TH, Stone JC, Sears K, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid Synth. 2023; 21(3): 494-506. doi:10.11124/JBIES-22-00430.
Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008; 51(1): S225-S239. doi:10.1044/1092-4388(2008/018).
Ramig L, Halpern A, Spielman J, Fox C, Freeman K. Speech treatment in Parkinson’s disease: Randomized controlled trial (RCT). Mov Disord. 2018; 33(11): 1777-91. doi:10.1002/mds.27460.
Ramig LO, Sapir S, Countryman S, et al. Intensive voice treatment (LSVT) for patients with Parkinson’s disease: a 2 year follow up. J Neurol Neurosurg Psychiatry. 2001; 71(4): 493-8. doi:10.1136/jnnp.71.4.493.
Ozdemir E, Norton A, Schlaug G. Shared and distinct neural correlates of singing and speaking. Neuroimage. 2006; 33(2): 628-35. doi:10.1016/j.neuroimage.2006.07.013.
Jacob P, Kahrilas PJ, Logemann JA, Shah V, Ha T. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989; 97(6): 1469-78. doi:10.1016/0016-5085(89)
-0.
Winiker K, Kertscher B. Behavioural interventions for swallowing in subjects with Parkinson’s disease: A mixed methods systematic review. Int J Lang Commun Disord. 2023; 58(4): 1375-1404. doi:10.1111/1460-6984.12865.
Fogg-Rogers L, Buetow S, Talmage A, et al. Choral singing therapy following stroke or Parkinson’s disease: an exploration of participants’ experiences. Disabil Rehabil. 2016; 38(10): 952-62. doi:10.3109/09638288.2015.1068875.