Prevalence and hematological characteristics of bacterial vaginosis in postmenopausal women
Main Article Content
Abstract
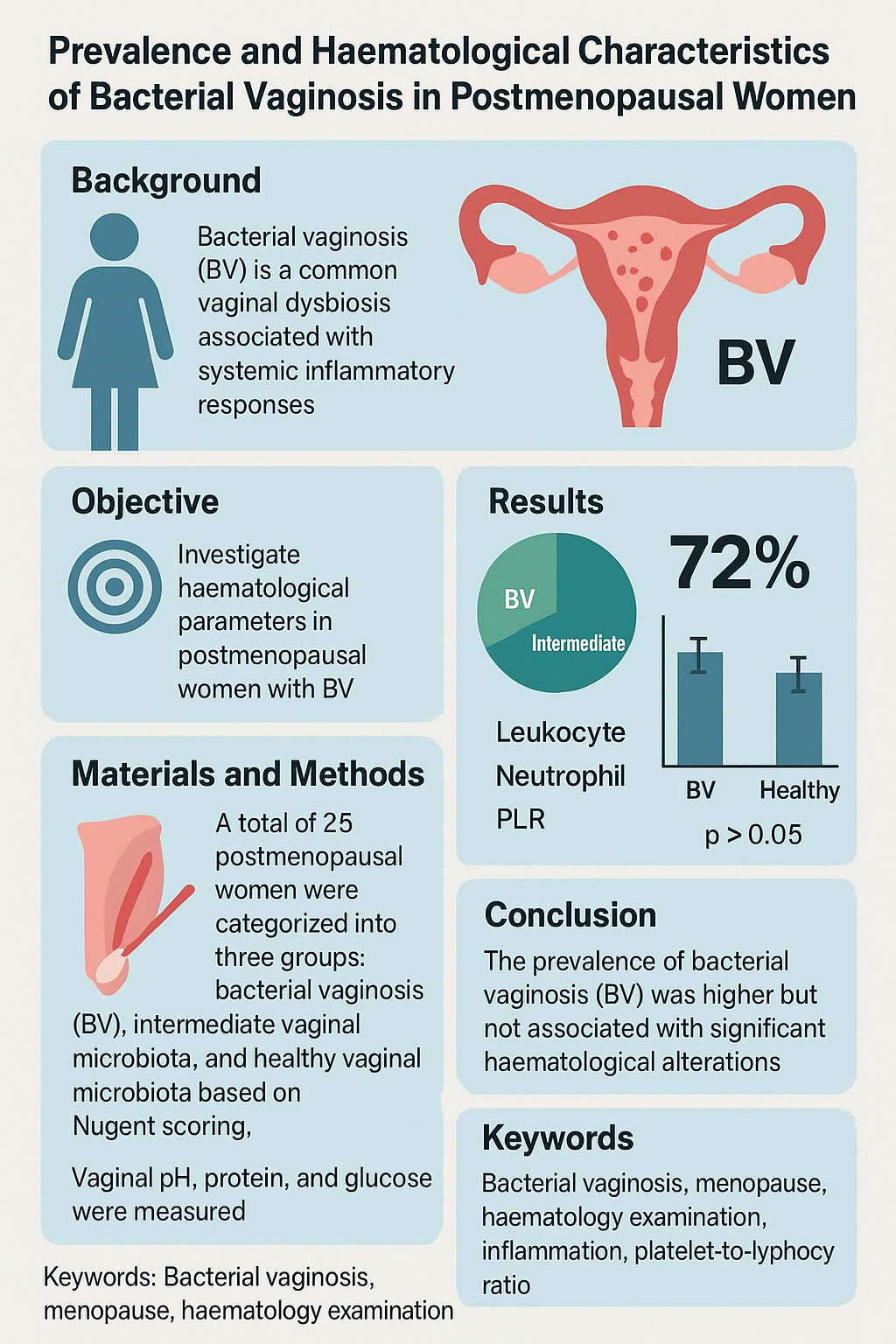
Background: Bacterial vaginosis (BV) is a common vaginal dysbiosis associated with systemic inflammatory responses. However, its hematological impact in postmenopausal women remains unclear. This study investigates hematological parameters in postmenopausal women with BV to assess potential systemic inflammatory alterations.
Objectives: This study aimed to investigate various hematological parameters across different BV conditions to better understand their potential role in BV diagnosis and pathophysiology.
Materials and methods: A total of twenty-five postmenopausal women were recruited and categorized into three groups: bacterial vaginosis (BV), intermediate vaginal microbiota, and healthy vaginal microbiota based on Nugent scoring. Vaginal samples were collected aseptically with the participants in the lithotomy position by swabbing the vaginal walls circumferentially near the cervical fornix. Nugent scoring was performed on Gram-stained smears to classify the subjects. Subsequently, Verify® urinalysis reagent strips were directly applied to the vaginal wall to measure pH, protein, and glucose levels. Additionally, hematological parameters including leukocyte count, lymphocyte, eosinophil, neutrophil, monocyte, basophil, platelet counts, and platelet-to-lymphocyte ratio (PLR) were assessed from peripheral blood samples. All data were statistically analysed and compared among the three groups using ANOVA and Kruskal–Wallis tests, with a significance level set at p<0.05.
Results: The prevalence of BV in postmenopausal women was 72%. Hematology parameters did not show significant differences across BV, intermediate, and healthy groups (p>0.05). Leukocyte, neutrophil, and PLR values were slightly higher in BV cases, but not to a statistically significant degree. These findings suggest that BV in postmenopausal women may not elicit strong systemic inflammatory responses compared to premenopausal populations. Additionally, pH, glucose, and protein levels did not differ significantly among the groups, highlighting the need to reconsider standard vaginal health biomarkers in postmenopausal women due to physiological changes induced by menopause.
Conclusion: The prevalence of bacterial vaginosis (BV) in this study was higher than that reported in previous studies; however, it was not associated with significant hematological alterations. Further research is needed to identify reliable systemic and vaginal biomarkers for BV diagnosis in this population, considering the potential influence of hormonal and immunological factors.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Verstraelen H, Swidsinski A. The biofilm in bacterial vaginosis: Implications for epidemiology, diagnosis and treatment: 2018 update. Curr Opin Infect Dis. 2019; 32(1): 38-42, doi: 10.1097/QCO.0000000000000516.
Muzny CA, Schwebke JR. Pathogenesis of bacterial vaginosis: Discussion of current hypotheses. J Infect Dis. 2016; 214(Suppl 1): S1-S5, doi: 10.1093/infdis/jiw121.
L. L. Stewart, L. A. Vodstrcil, J. Coombe, C. S. Bradshaw, J. S. Hocking. Prevalence of bacterial vaginosis in postmenopausal women: A systematic review and meta-analysis. Sex Health. 2022; 19(1): 17-26, doi: 10.1071/SH21083.
O. T. Van Gerwen, S. E. Smith, C. A. Muzny. Bacterial vaginosis in postmenopausal women. Curr Infect Dis Rep. 2023; 25(1): 7-15, doi: 10.1007/s11908-022-00794-1.
A. Challa, S. Sood, G. Kachhawa, A. D. Upadhyay, S. N. Dwivedi, S. Gupta. Diagnostic concordance between Amsel’s criteria and the Nugent scoring method in the assessment of bacterial vaginosis. Sex Health. 2022; 18(6): 512-4, doi: 10.1071/SH21149.
B. A. D. Genazzani, M. Milani. Postmenopausal Vaginal Atrophy : Non-hormonal therapy with a moisturizing bioadhesive vaginal gel. 08-0132_tr00E_M2[Internet]. 2003; 18:14-16. Available from: https://www.replens.eu/fr/wp-content/uploads/sites/2/2018/02/Atrophie-vaginale-post-m%C3%A9nopause.pdf.
F. Palma, A. Volpe, P. Villa, A. Cagnacci. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA study. Maturitas. 2016; 83: 40-4, doi: 10.1016/j.maturitas.2015.09.001.
S. Cauci et al. Interrelationships of interleukin-8 with interleukin-1β and neutrophils in vaginal fluid of healthy and bacterial vaginosis positive women. Mol Hum Reprod. 2023; 9(1): 53-8, doi: 10.1093/molehr/gag003.
R. P. Nugent, M. A. Krohn, S. L. Hillier. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991; 29(2): 297-301, doi: 10.1128/jcm.29.2.297-301.1991.
S. Panda, A. Das, A. Singh, S. Pala. Vaginal pH: A marker for menopause. J Midlife Health. 2014; 5(1): 34, doi: 10.4103/0976-7800.127789.
J. Saimin, Y. Purnamasari, S. A. Mulyawati, N. I. Purnamasari, Arismawati, F. Sandra. Vaginal acidity affects vaginal microbiota in postmenopausal women. Indones Biomed J. 2022; 14(2): 206-10, doi: 10.18585/inabj.v14i2.1836.
A. Swidsinski et al. Antimicrobial susceptibility of microbiota in bacterial vaginosis using fluorescence In Situ hybridization. Pathogens. 2022; 11(4): 1-15, doi: 10.3390/pathogens11040456.
B. J. Bain. Structure and function of red and white blood cells. Med. (United Kingdom). 2017; 45(4): 187-93, doi: 10.1016/j.mpmed.2017.01.011.
C. Escalda, J. Botelho, J. J. Mendes, V. Machado. Association of bacterial vaginosis with periodontitis in a cross-sectional American nationwide survey. Sci Rep. 2021; 11(1): 1-9, doi: 10.1038/s41598-020-79496-4.
T. Chen et al. Dysbiosis of the rat vagina is efficiently rescued by vaginal microbiota transplantation or probiotic combination. Int J Antimicro. Agents. 2021; 57(3): doi: 10.1016/j.ijantimicag.2021.106277.
M. et all Vakhshoori. The impact of platelet-to-lymphocyte ratio on clinical outcomes in heart failure: a systematic review and meta-analysis. Ther Adv Vaccines. 2024; 18: 1-22, doi: 10.1177.
Motta F, Di Simone N, Selmi C. The impact of menopause on autoimmune and rheumatic diseases. Clin Rev Allergy Immunol. 2025; 68(1): 1-15. Available from: https://doi.org/10.1007/s12016-025-09031-8.
Averyanova M, Yureneva S, Kiseleva V, Yakushevskaya O, Iskusnykh M, Pavlova A, et al. Effect of menopausal hormone therapy on cellular immunity parameters and cytokine profile. Biomedicines. 2024; 12(8), doi: 10.3390/biomedicines12081892.